1. Background
Enuresis is the most common urologic condition in children who are mature enough, over 5 years of age, to achieve continence (1). It is classified as diurnal (daytime) and nocturnal (nighttime) enuresis also divided into primary (ie, never achieved dryness) and secondary (ie, dryness for at least 6 months) (2). The present study investigated nocturnal and primary enuresis. Enuresis prevalence rates are reported as 15%, 7%, and 1% in 5, 8, and 15 years of age, respectively. The enuresis odds ratio in boys and girls is 1.4:1 (3, 4). About the etiology of nocturnal enuresis, there is multifactorial pathology, such as delayed cortical maturation, genetic factors, psychological factors, behavioral disorders, and sleep disorders, as probable etiology. However, two-thirds of children with enuresis suffer from urinary incontinence that can be related to the problems of stimulating sleep. (5).
In addition, sleep disorders have been divided, based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria, into crooked and nightmares categories (6). sleep disorders are divided
based on the quantity or timing of sleep disorders and include insomnia and constant sleeping. Insomnia causes disturbance in the quality or quantity of sleep that depends on a specific disorder and might be associated with interference in sleep indicators (7, 8).
Nightmares are abnormal behaviors during sleep or transitions between sleep and wakefulness. In addition, cultural, climatic, and geographic factors influenced nightmare incidence, and specific incidence might play an important role in revealing nightmares. Therefore, a high prevalence of nocturnal enuresis in children can increase the incidence of sleep disorders, and sleep disorders can induce nocturnal enuresis incidence.
There are some drugs for the treatment of primary monosymptomatic nocturnal enuresis (PMNE) and sleep disorders; however, there are many side effects, and none of the drugs is crucial. Furthermore, the prevention of sleep disorders by reducing nocturnal enuresis can be more effective with fewer complications. Therefore, this study was conducted to determine the association between sleep disorders and nocturnal enuresis; nevertheless, such studies have been rarely performed outside Iran and never in Iran.
2. Objectives
This study aimed to survey children with PMNE about sleep disorders and evaluate their correlation.
3. Methods:
3.1. Study Setting
This case-control study was conducted on children in Amir-Kabir hospital, Arak, Iran.
3.2. Study Population
In this clinical study, 132 children with and without PMNE, including 66 children with PMNE as the case group and 66 healthy children as the control group, were selected using convenience sampling. The patients were selected from children referred to the Pediatric Clinic of Amir-Kabir hospital with PMNE diagnosis based on Nelson criteria. The inclusion criteria were patient selection based on Nelson criteria, 5-18 years of age, consent to participate in the research project, absence of mentally retarded and other physical diseases, absence of mental-emotional problems according to Nelson book, and absence of congenital kidney disease. The exclusion criteria were withdrawal from the study for no reason, no satisfaction with using their data in the study, and a severe liver, kidney, or cardiac disease.
3.3. Measurements
The study information was obtained from a questionnaire taken from a reference book (ie, Kaplan and Sadock’s Synopsis of Psychiatry) (9). While obtaining informed consent from the parents, sleeping checklists (including primary insomnia, primary hypersomnia, narcolepsy, sleep-related breathing disorder, circadian rhythm disorder, nightmare, sleep terror disorders, somnambulism, and uncertain insomnia) were gone through under a psychiatrist’s guide and diagnostic criteria and were completed for each of the sleep disorders. This study evaluated the patients for nine types of sleep disorders based on the DSM-IV-TR. For the calculation of the mean scores of sleep disorders in the two groups, 1 and 0 were given to positive and negative scores, respectively.
3.4. Statistical Analysis
Data analysis in SPSS software (version 23) was conducted using the chi-square test, with significance differences considered less than 0.05.
3.5. Ethical Considerations
Double publication, plagiarism, and data fabrication were considered in this study. Moreover, the current study was approved by the Ethics Committee of Arak University of Medical Sciences, Arak, Iran (ethics code: AUMS 91-135-7)
4. Results
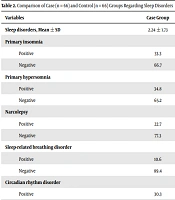
As shown in Table 1, there was a statistically significant difference in the mean scores of age between the groups (P = 0.28). Furthermore, based on Table 2, the total mean score of disorders was 1.31 ± 1.25, with 0.38 ± 0.78 and 2.24 ± 1.73 in the control and case groups, respectively (P = 0.001), with a significant difference. There were statistically significant differences in six of nine sleep disorders between the groups. Primary sleep insomnia in 22 (33.3%) and 4 (6.1%) (P = 0.001), primary hypersomnia in 23 (34.8%) and 1 (1.5%) (P = 0.001), narcolepsy in 15 (22.7%) and 0 (0%) (P = 0.001), circadian rhythm sleep disorders in 20 (30.3%) and 2 (3%) (P = 0.001), and nightmare disorder in 22 (33.3%) and 12 (18.2%) patients of the case and control (P = 0.036) groups were observed, respectively. Sleep terror disorders were observed in 29 (43.9%) and 2 (3%) patients of the case and control groups, respectively (P = 0.001). Three sleep disorders without significant differences were uncertain insomnia (P = 1.0), sleep-related breathing (P = 0.062), and somnambulism (P = 0.38).
| Group | Age (Mean ± SD) |
|---|---|
| Case | 9.24 ± 1.41 |
| Control | 8.89 ± 2.19 |
| Total | 9.06 ± 1.8 |
| P-value | 0.28 |
| Variables | Case Group | Control Group | Total | P-Value |
|---|---|---|---|---|
| Sleep disorders, Mean ± SD | 2.24 ± 1.73 | 0.38 ± 0.78 | 1.31 ± 1.25 | 0.001 |
| Primary insomnia | ||||
| Positive | 33.3 | 6.1 | 19.7 | 0.001 |
| Negative | 66.7 | 93.9 | 80.3 | |
| Primary hypersomnia | ||||
| Positive | 34.8 | 1.5 | 18.1 | 0.001 |
| Negative | 65.2 | 98.5 | 81.9 | |
| Narcolepsy | 0.001 | |||
| Positive | 22.7 | 0 | 11.3 | |
| Negative | 77.3 | 100 | 88.7 | |
| Sleep-related breathing disorder | 0.062 | |||
| Positive | 10.6 | 1.5 | 11.3 | |
| Negative | 89.4 | 98.5 | 88.7 | |
| Circadian rhythm disorder | 0.001 | |||
| Positive | 30.3 | 3 | 16.7 | |
| Negative | 69.7 | 97 | 83.3 | |
| Nightmare | 0.036 | |||
| Positive | 33.3 | 18.2 | 25.7 | |
| Negative | 66.7 | 81.8 | 74.3 | |
| Sleep terror disorders | 0.001 | |||
| Positive | 43.9 | 3 | 23.4 | |
| Negative | 56.1 | 97 | 76.6 | |
| Somnambulism | 0.38 | |||
| Positive | 15.2 | 4.5 | 9.9 | |
| Negative | 84.8 | 95.5 | 90.1 | |
| Uncertain insomnia | 1.0 | |||
| Positive | 0 | 0 | 0 | |
| Negative | 100 | 100 | 100 |
5. Discussion
This study aimed to consider the sleep disorders prevalence in children with PMNE. Although there has been no similar study on sleep disorders and urinary incontinence, and none of the current studies is in line with the present study, some studies previously conducted on sleep disorders in children with enuresis are reviewed in this section.
Park et al., in 2016, tried to find an association between sleep-disordered breathing and nocturnal enuresis (10). In addition, in a study on sleep disturbances and nocturnal enuresis performed by Azevedo Soster et al., they observed that children with nocturnal enuresis have high comorbidity with other sleep disorders, including parasomnias and sleep-disordered breathing (11). In a study conducted by Cohen-Zrubavel et al. in 2011 entitled “Sleep and Sleepiness in Children with Nocturnal Enuresis”, it was concluded that children with normal sleep enuresis have significantly higher disorders, and children with enuresis experienced higher levels of sleepiness. This finding indicates that children with enuresis suffer from frequent awakenings that can explain a higher threshold of stimulation in them (12).
Candra et al. investigated the prevalence of urinary symptoms in sleep problems in children with enuresis stimulation. In the aforementioned study, it was concluded that daily urinary symptoms in two-thirds of patients are associated with enuresis; however, it might be forgotten in the history taking. It seems that stimulated problems have a significant role in primary enuresis and instability symptoms of urinary tract infections (UTIs) in secondary enuresis and the detrusor muscle. In patients with urinary incontinence at night, a history of urinary frequency, nocturnal sleep irritation, UTIs, fecal incontinence, learning disorders, and psycho-social or family history of UTI increase doubt associated with urinary symptoms of voiding dysfunction (13). Tai et al. observed that urinary incontinence prevalence is similar to that reported in the northern part of Taiwan and western countries; nevertheless, it is higher than in Hong Kong and China. Difficulty in waking and wetting beds are only notable points associated with the intensity of urinary incontinence (14).
Carotenuto et al. demonstrated that the etiology and pathogenesis of PMNE are multifactorial, and it is believed that more than one factor affects each patient. There has not been an only reason that could show the etiology in the studies; however, multifactorial etiology has been observed in- case group studies. Most children with PMNE do not have psychiatric, neurologic, or urologic problems; therefore, they do not need medical treatments. Nonorganic reasons, such as emotional factors, are at the forefront of enuresis investigations; however, 2 - 3% of enuresis is based on organic reasons (15).
Although numerous different theories, including urodynamic, behavioral, genetic, hereditary, developmental, hormonal, neurologic, sleep disturbance, and psychological theories, can explain some selected cases, no one theory explains the true etiology and pathogenesis of PMNE. Other studies have also investigated this problem. Studies conducted in this field demonstrated that the removal of airways blockade can reduce nocturnal enuresis frequency (16). The findings of other studies also showed no significant difference in demographic characteristics between the two groups (17).
The limitation of the present study was considered false and defective questionnaires filling out by the parents; accordingly, when the effect of PMNE on the overactive bladder and other body systems were explained, they agreed to cooperate. Furthermore, it is recommended to devote attention to severity factors related to voiding dysfunction. It is also suggested to perform further studies with larger sample size and on the evaluation of mental disorders and confirm the results of the present study.
5.1. Conclusions
The PMNE has an important effect on sleep disorders (SD), which induces them in children, so we can reduce these sleep disorders in children by controlling PMNE.