1. Background
The ideal execution of motor tasks in medicine is essential for physicians and medical practitioners to perform medical procedures legitimately. Over the past years, a considerable amount of research has attempted to understand optimal conditions to perform motor skills, mostly focused on motivational and attentional components. Wulf and Lewthwaite (1) developed the optimizing performance through intrinsic motivation and attention for learning (OPTIMAL) theory, which shows the essential role of motivational and attentional components in the optimal performance of motor skills. The influential factors in the OPTIMAL theory are (1) enhanced expectancies for future performance, (2) supporting learners’ autonomy, and (3) promoting an external focus of attention. Enhanced expectancies and autonomy are considered motivational factors, and external focus of attention is considered an attentional factor to optimize motor skill performance (1).
A key principle in the OPTIMAL theory is that motivational and attentional needs must be met for optimal motor performance to occur. In the OPTIMAL theory, enhanced expectancies refer to beliefs about what is to occur, which are based on previous experience. Autonomy alludes to circumstances in which an individual is permitted to control or select a few items of execution conditions. Finally, the external focus of attention alludes to concentrating on the movement objective or impact (1). Furthermore, regarding the OPTIMAL theory, self-efficacy plays an important role, because enhanced expectancies and autonomy support (AU) are invoked through the self-efficacy structure. Self-efficacy is, for the most part characterized as the conviction in one’s capacity to succeed in particular circumstances or to perform a skill (2). Several studies have tested the effects of the instructions based on the motivational and attentional factors in the OPTIMAL theory (i.e., enhanced expectancies, AU, and external focus of attention) and found that these factors positively affect performance and self-efficacy in a variety of motor tasks and across a range of age groups (3-16).
However, the OPTIMAL theory has received less attention in medical education. The probable reason may be that the researchers who studied these factors were mainly specialists in the field of sports science and employed mostly sports skills. Therefore, the effects of motivational and attentional factors in the OPTIMAL theory on the performance of medical motor skills such as laparoscopy and suturing, have rarely been investigated. Hence, it is not clear whether these motivational and attentional factors in the OPTIMAL theory can be generalized to the optimal performance of medical motor skills. Accordingly, this study was designed to examine the effects of motivational factors regarding the OPTIMAL theory (enhanced expectancies and AU) on the performance of medical motor skills.
Based on the OPTIMAL theory, enhancing expectancies in the form of positive feedback impacts motor performance and self-efficacy (1). Positive feedback could be presented in various forms, including social-comparative feedback, self-modeling, and feedback on “good” trials (1). In this study, we applied social comparative feedback (SCF) to enhance expectancies for future performance, which resulted in executers to accept that their execution is predominant to that of their counterparts. In the literature, it has been shown that positive SCF enhances motor performance in a delayed retention test (17-19). For example, Ávila et al. (17) investigated the effects of SCF on the learning of the throwing skill in children. The subjects in the SCF group were given fake feedback recommending that their execution was superior to that of a counterpart. The results showed that positive SCF resulted in greater throwing accuracy and higher perceived competence compared to the control (CO) group. Additionally, Chiviacowsky et al. (18) investigated the effects of positive temporal-comparative feedback on putting golf balls. During practice, the temporal-comparative feedback group was told that the mean of their execution was superior to past trials. The results indicated that positive SCF led to better motor performance and perceived competence relative to the CO group. The above-mentioned findings reveal that positive SCF influences the performance of motor tasks and emphasizes the essential role of the motivational part of feedback in motor performance. Nevertheless, as far as we know, the effects of enhanced expectancies in the form of positive SCF on the performance of medical motor skills have not been examined in previous studies. To fill the gap in this area, the current research aimed to investigate the effects of positive SCF on the performance and self-efficacy of the suturing motor skill in medical trainees.
The second factor examined in the present study was AU which is considered a motivational factor in the OPTIMAL theory. Autonomy alludes to circumstances in which an individual is permitted to control or select a few items of execution conditions (1). Several studies have shown that AU facilitates motor performance and self-efficacy in a variety of motor skills when compared with the control condition (6, 7, 20, 21). For instance, Chiviacowsky and Wulf (7) and Chiviacowsky et al. (20) found that AU benefits performance in a sequential timing task and throwing skill, respectively. Furthermore, there is a body of evidence that AU increases self-efficacy. For example, Chiviacowsky (6) found that AU resulted in higher self-efficacy after the acquisition phase compared with the control condition. Wulf et al. (15) demonstrated that AU led to higher self-efficacy than the yoked group. Wulf and Lewthwaite (1) argued that the potential fundamental mechanisms for the advantages of the AU condition might incorporate easing of execution through upgraded handling of skill-related delusions and greater self-regulatory responsiveness. Advantages of autonomy also incorporate the opportunity to improve desires for future executions, too (1).
2. Objectives
To the best of our knowledge, the effects of AU on performing a medical motor skill have not yet been examined. Therefore, the aim of the current research was to investigate the effects of enhanced expectancies and AU on learning a medical motor skill (i.e., a vertical mattress suture). Based on the OPTIMAL theory, we assumed that the positive SCF and AU groups would show better motor performance and higher self-efficacy compared with the CO group.
3. Methods
3.1. Participants
Sixty-three right-handed medical students (aged between 18 and 20 years old) willingly participated in this study and were randomly assigned to SCF, AU, and CO groups. All participants were in the pre-clinical stage of their studies (years 1 and 2 of medical education). According to a self-reported questionnaire, none of the participants were familiar with the motor task of this study and had not performed it before. Therefore, they were naïve to the experimental task. Exclusion criteria included any condition that may have interfered with completing suturing techniques. We performed this study based on the Declaration of Helsinki, and our protocol was confirmed by the Islamic Azad University of Gonbad Kavous’ institutional review board (27.15.5.3137). Written consent was obtained from all participants.
3.2. Motor Task
A vertical mattress suture was chosen as the motor task in this study. Suturing is one of the fundamental skills for medical doctors. Furthermore, this is one of the most difficult and challenging surgical skills to acquire and master. The vertical mattress suture is a common suture technique used to close wounds. The vertical mattress suture has some advantages, including providing closure for both deep and superficial layers and allowing perfect eversion and vertical opposition of the superficial skin edges. Before performing the suturing task, the participant was gowned and gloved and then sat down at a table on which were the tools needed to perform the motor task including a mannequin with artificial lacerations and suturing-related instruments, such as needle, scissors, forceps, and silk sutures. Then, the participant watched a 1-hour video demonstration containing instruction given by an expert about vertical mattress suturing. The participant observed the video demonstration once uninterrupted and without any movements. After observation, the participant followed the protocol described in the next section.
3.3. Dependent Measures
3.3.1. Suturing Assessment
We used the University of Western Ontario Microsurgery Skills Acquisition/Assessment instrument (UWOMSA) to assess suturing skills. UWOMSA is a validated assessment tool for evaluating suturing skills and comprises 3 items, including quality of knot, efficiency, and handling. Every item has a score based on a 5-point Likert scale, and the total score is a maximum of 15. To assess the suturing performances, we filmed 10 trials of the participant (please see the Experimental Design section for further details), and then asked 2 experienced surgeons to score the videotaped performances using the UWOMSA guidelines. The inter-rater reliability of ratings provided by the 2 examiners was 0.82, indicating substantial agreement.
3.3.2. Self-efficacy
Self-reported self-efficacy was measured at several time points, including prior to the pretest, each training day, and the posttest. The total score of this questionnaire ranges from 0 (not certain at all) to 100 (completely certain) with a span of 10 identical breaks and measures the participant’s ability beliefs related to suturing. The scale was developed according to Bandura’s recommendations (2).
3.4. Experimental Design
The participants were tested individually on the pretest and posttest. Prior to entering the acquisition stage, all participants conducted the pretest in which they performed vertical mattress sutures and completed the self-efficacy scale. The suturing performance of participants in the pretest was filmed for further assessment. Then, the students participated in an acquisition phase in which they practiced the suturing task for 1 hour each day for 5 days. During the hour-long training sessions, participants attempted as many knots as possible. During the practice, the participants were free to watch the instructive video demonstration anytime they requested. Suturing performance was captured for specified trials (2 trials per session) with 2 cameras in the same position without any impedances or advice from the individuals filming. These recorded films were later used to assess the suturing performances. One day after the completion of the protocol, the students participated in the posttest, which was similar to the pretest. Regarding the self-efficacy component, it should be noted that the subjects completed the self-efficacy scale before the pre-test, before the start of training on the second, third, fourth and fifth days, and also before the post-test.
To add positive social comparison feedback to the protocol, the students in the SCF group were told that an expert rater would immediately evaluate their filmed performance in another room and the results would be presented to them at the end of the day. More specifically, students in the SCF group received feedback indicating that they performed better than their peers. Students in the CO group did not receive any SCF; however, they were told that an expert would also evaluate their filmed performance.
To add AU to the protocol, students in the AU group were told that they were free to choose the color of silk suture. There were silk sutures in white, black, and pink colors. It has to be noted that participants in the SCF and CO groups only used white silk sutures for their suturing performances. Indeed, we used this kind of AU based on a previous study by Lewthwaite et al. (22), which aimed to investigate the effects of task-relevant AU (i.e., color of golf balls) on learning a golf-putting task. The AU group was given the option of choosing the color of golf balls (white, yellow, or orange) for their performances, while the yoked group was not allowed to choose the color. Lewthwaite et al. (22) found that the choice group performed better than the CO group in the delayed retention test.
3.5. Data Analysis
One-way analysis of variance (ANOVA) was employed to compare the experimental groups in the pretest. Moreover, a 3 (“group”: SCF, AU, and CO) × 5 (“day”: 5-day training) ANOVA with repeated measures on the last factor was utilized to analyze suturing and self-efficacy scores in the training period. One-way ANOVA was applied to compare the experimental groups in the posttest. The significance level was set at P < 0.05.
4. Results
4.1. Suturing Assessment
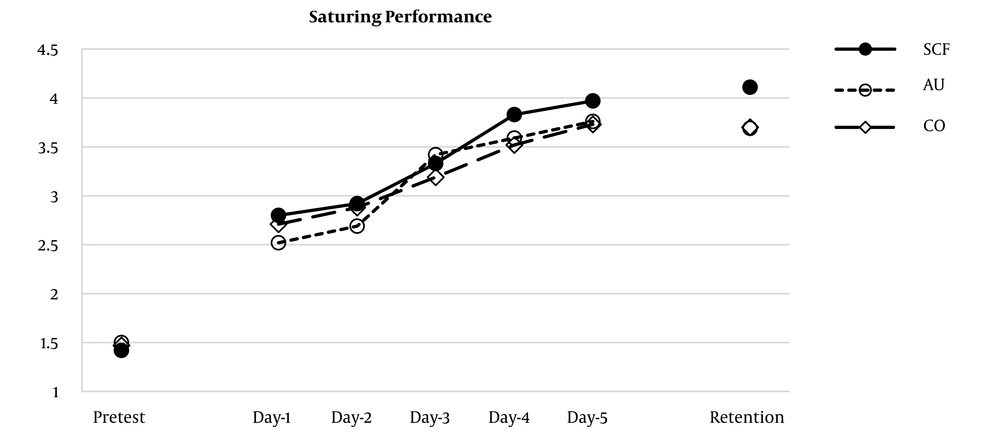
The mean and SD of suturing scores in the study are demonstrated in Table 1 and Figure 1. The results of the pretest showed no significant differences between groups before the training phase (F2,60 = 0.088; P = 0.916). Within the training period, main effect for the “group” was not significant (F2,60 = 1.66; P = 0.197). However, main effect for the “day” (F4,240 = 138.08; P = 0.00; εpar2 = 0.69), and the “group” × “day” interaction (F8,240 = 2.125; P = 0.034; εpar2 = 0.06) were significant. On the posttest, our findings revealed a significant main effect for the “group” (F2,60 = 6.04; P = 0.004). Here, the SCF group performed significantly better than the AU and CO groups (P = 0.007 and P = 0.018, respectively). However, no significant difference was found between the AU and CO groups (P = 0.934).
| Groups | Pretest | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Retention |
|---|---|---|---|---|---|---|---|
| SCF | 1.42 ± 0.55 | 2.80 ± 0.66 | 2.92 ± 0.63 | 3.33 ± 0.63 | 3.83 ± 0.59 | 3.97 ± 0.51 | 4.11 ± 0.52 |
| AU | 1.50 ± 0.54 | 2.52 ± 0.37 | 2.69 ± 0.48 | 3.42 ± 0.36 | 3.59 ± 0.30 | 3.76 ± 0.25 | 3.69 ± 0.40 |
| CO | 1.47 ± 0.58 | 2.71 ± 0.33 | 2.88 ± 0.35 | 3.19 ± 0.37 | 3.52 ± 0.37 | 3.73 ± 0.40 | 3.70 ± 0.37 |
4.2. Self-efficacy Scores
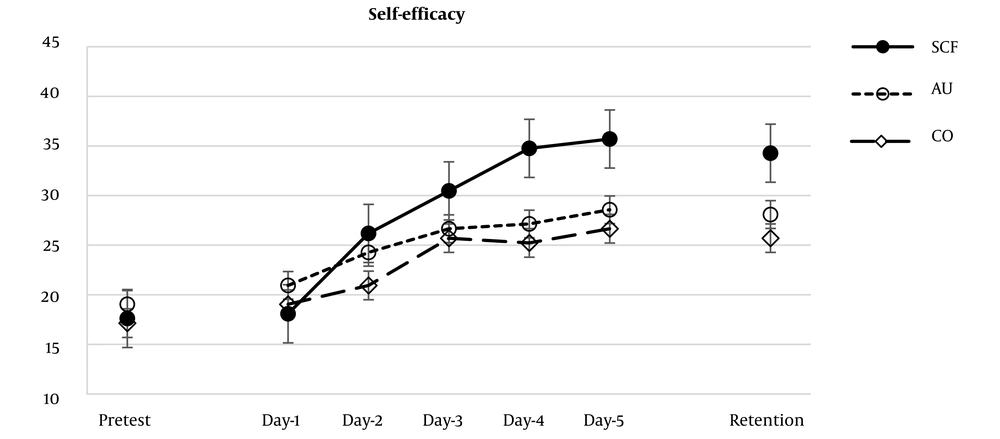
The mean and SD of self-efficacy scores in the study are demonstrated in Table 2 and Figure 2. The analysis of the pretest demonstrated no significant differences between the groups before entering the training period (F2,60 = 0.518; P = 0.598). During the training period, the main effect for the “group” was significant (F2,60 = 7.35; P = 0.001; εpar2 = 0.19). The SCF group reported significantly higher self-efficacy scores compared with the AU and CO groups (P = 0.048 and P = 0.001, respectively). Nevertheless, there were no significant differences between the AU and CO groups (P = 0.362). The main effects for the “day” (F4,240 = 58.03; P = 0.000; εpar2 = 0.49) and the “group” × “day” interaction (F8,240 = 5.98; P = 0.000; εpar2 = 0.16) were significant. These results indicate that participants in the SCF group increased their self-efficacy scores during the practice phase, while the self-efficacy of participants in the AU and CO groups did not change. Our findings revealed a significant main effect for the “group” on the retention test (F2,60 = 11.46; P = 0.000; εpar2 = 0.41). The SCF group reported significantly higher self-efficacy scores compared with the AU and CO groups (P = 0.004 and P = 0.000, respectively). Nonetheless, there was no significant difference between the AU and CO groups (P = 0.407).
| Groups | Pretest | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Retention |
|---|---|---|---|---|---|---|---|
| SCF | 17.61 ± 6.24 | 18.09 ± 6.79 | 26.19 ± 6.69 | 30.47 ± 7.40 | 34.76 ± 8.13 | 35.71 ± 7.46 | 34.28 ± 7.46 |
| AU | 19.04 ± 7.00 | 20.95 ± 6.24 | 24.28 ± 7.46 | 26.66 ± 5.77 | 27.14 ± 4.62 | 28.57 ± 5.73 | 28.09 ± 5.11 |
| CO | 17.14 ± 5.60 | 19.04 ± 6.24 | 20.95 ± 5.38 | 25.71 ± 5.07 | 25.23 ± 5.11 | 26.66 ± 4.83 | 25.71 ± 5.07 |
4.3. Regression Analysis
Self-efficacy scores in the pretest did not significantly predict executions in the pretest (F1,61 = 0.781; P = 0.380; adjusted R2 = 0.013; β = -0.112). However, self-efficacy scores during the practice phase significantly predicted suturing performances during the practice phase (F1,61 = 8.45; P = 0.005; adjusted R2 = 0.122; β = 0.349). Moreover, self-efficacy scores in the retention test significantly predicted suturing performances in the retention test (F1,61 = 5.63; P = 0.021; adjusted R2 = 0.085; β = 0.221).
5. Discussion
The OPTIMAL theory suggests that enhancing expectancies for future performance and supporting learners’ autonomy promote motor performance and learning (1). However, the effects of these factors on the performance of medical motor skills (such as suturing) have rarely been investigated. Hence, it is not clear whether these factors can be generalized to the optimal performance of medical motor skills. Accordingly, the aim of the current research was to examine whether enhancing expectancies (e.g., by giving learners positive SCF) and AU (e.g., by giving participants the option of choosing the color of silk sutures) could lead to superior motor performance and learning and self-efficacy. According to the OPTIMAL theory, it was hypothesized that enhanced expectancies and autonomy support would lead to better motor performance as well as higher self-efficacy than the control condition.
Regarding enhanced expectancies, the results showed that positive SCF led to more successful learning than the control condition did regarding suturing quality. However, the results indicated no immediate effects for positive SCF on motor performance because we found similarities between groups regarding suturing quality in the training period. It means that when positive SCF was present within training, it led to an almost persistent (i.e., learning) impact because we found significantly higher suturing scores regarding the retention test in the SCF group than in the CO group. Consistent with previous studies (17-19), this study also indicated that positive feedback in the form of SCF was clearly more beneficial for motor learning of a medical motor skill compared to the control condition (i.e., traditional teaching). These findings confirm the first part of our hypothesis and indicate that positive SCF benefits learning motor medical skills.
Regarding AU, the results demonstrated that the autonomy condition did not lead to significantly higher accuracy suturing quality in the retention test compared to the CO condition. Moreover, our findings demonstrated no immediate impact for AU on motor execution because we observed no significant differences between the AU and CO groups regarding suturing quality during the training period. These findings indicate that giving people the freedom to manage training condition did not benefit motor performance or learning of a medical motor skill. In this regard, our findings are not in line with previous studies (6, 7, 20, 21).
More interestingly, positive SCF also influenced self-efficacy positively. Our findings revealed that positive SCF resulted in significantly higher self-efficacy scores during the training period and retention test compared to the control condition. These finding confirm the assumptions of the OPTIMAL theory, indicating that enhanced expectancies enhance motivation and motor learning (1). These findings are in line with Badami et al., (4, 5) and Saemi et al., (14), despite the fact that previous studies have only measured motivation after the acquisition phase. However, we measured self-efficacy also prior to the retention test, which led us to investigate the persistent impacts of enhanced expectancies on motivation in the no-feedback conditions. Our findings showed that that positive SCF had distinctly enhanced motivation during the training period and certainly, it endured at a higher state until the retention test than the control condition.
Our findings also have practical applications. An imperative topic for teachers is how to enhance the self-efficacy state of learners while learning novel medical motor skills. Our findings recommend that giving positive SCF could be employed as a valuable method to increase self-efficacy, which based on the OPTIMAL theory, later facilitates motor learning.
However, AU did not increase the level of self-efficacy. The results demonstrated that the AU group did not show significantly higher self-efficacy scores during the training period, or retention test compared with the CO group. The findings did not confirm the prediction of the OPTIMAL theory that AU would affect motivational states such as self-efficacy (1). The results also are not in line with the results of previous studies (6, 7, 20, 21). The present findings indicate that AU in the form of choosing the color did not increase motivation during the practice and retention test compared to the CO condition.
These findings can be interpreted by various explanations. Based on behavioral perspectives, it may be conceivable that positive SCF enhances the feeling of self-efficacy and self-confidence in the person and may consequently diminish worries and the need to assign attentional resources to self-regulatory activities. It may subsequently have led to higher goal-setting and have enhanced motor learning (1, 4). Based on neuroscientific perspectives, reward-related dopamine boosts the response of memories during rest that comes up with the consolidation of motor memories (1, 23, 24). Regarding the OPTIMAL theory, it is expected that the enhanced expectancies facilitate motor learning by making dopamine available for memory consolidation and neural pathway development, and come up with coherent goal-action coupling by readying the motor system for task performance (1). Performing under optimal motivational conditions (e.g., enhancing expectancies) is assumed to facilitate functional connectivity, that is, task-specific neural connections across distinct brain regions (3). Enhanced expectations resulted from positive SCF and their temporal match with training may have resulted in more coherent retention execution observed in the SCF group (1).
5.1. Conclusions
In summary, our findings support the OPTIMAL theory by demonstrating that enhanced expectancies in the form of positive SCF can facilitate learning of a medical motor skill, i.e., vertical mattress suturing. These findings also have practical applications. Such results suggest that professors and trainers in the field of medical education may have the choice to facilitate learning new medical motor skills in novices by enhancing learners’ expectancies during the training period.