1. Background
Obesity is a harmful accumulation of body fat that has a detrimental effect on health and well-being. It results from a positive energy balance due to extra calorie intake and/or insufficient physical activity. It is a multifactorial disorder resulting from the interaction of genetics, environment, and lifestyle (1). Obesity in children and adolescents is associated with severe physical complications such as cardiovascular problems, metabolic disorders (hypertension, insulin resistance, and hyperlipidemia), orthopedic difficulties, night apnea, asthma, and psychosocial complications such as low self-esteem and isolation from society. If obesity is not identified and treated, its complications will continue to adolescence and cause lifetime problems (2).
In recent decades, rapid lifestyle changes have occurred due to the industrialization of societies. The global prevalence of obesity has doubled in the last four decades in childhood at the age of 5 - 19 and in the age group of 2 - 4 years (3). The World Health Organization has developed a plan to end childhood obesity (WHO ECHO) and created a comprehensive and integrated package of recommendations for addressing childhood obesity. In Iran, we are witnessing a growing trend of childhood obesity. National studies have measured the prevalence of overweight, obesity, and abdominal obesity. Therefore, the Iranian version of the program to end childhood obesity (IRAN ECHO) was adopted by examining children's habits, lifestyles, and nutrition and providing corrective suggestions (4).
In 2005, the US Preventive Services Task Force (USPSTF) found that body mass index (BMI), adjusted for age and sex (calculated as weight in kilograms divided by height squared in meters), can be used as a reliable method for detecting overweight or obesity in children over six years and adults (5). Numerous studies have been performed to evaluate the accuracy and importance of this indicator in diagnosing overweight children. The Centers for Disease Control and Prevention (CDC) insisted on recording BMI in the growth chart for children after the age of two years. Since 2011, the International Cardiovascular Society has also stated the need for screening children aged two years and older for obesity based on BMI (6, 7). However, the need for training on calculating this index can be an obstacle to its widespread use, so they have always been looking for an easier way to identify the onset of obesity in children (8). Such an approach can help increase clinical assessment and public health surveillance of overweight and obesity, especially in developing countries because of the more prevalence of obesity in these communities (9).
Mid-upper arm circumference (MUAC) is an easy, practical, and cost-effective method to identify children and adults with malnutrition. Although numerous studies have been done in this regard, there are limited articles on the possibility of using this index to identify obesity in children (10).
2. Objectives
This study aimed to investigate the relationship between MUAC and BMI in children aged 6 - 12 years.
3. Methods
This cross-sectional study was carried out at Lavizan primary schools in a residential area. All normal healthy students willing to cooperate were included in the study using a census method. The sample included 455 subjects, comprising 177 boys and 278 girls, in the age range of 6 - 12 years. The prevalence of normal BMI in Iranian children was considered 70% (3), and based on Cochran's sample size formula, we needed at least 322 subjects. We considered an accuracy level of 0.05 and a confidence level of 95% for our study.
First, the principals, school officials, and parents were justified. Also, the ethical code of IR.AJAUMS.REC.1397.084 was received. Our researcher was trained for sampling to collect anthropometric data (height, weight, BMI, and MUAC). In order to reduce errors, measurements were performed twice, and an average was calculated. Also, to validate the data, all measurements were made by the same person, scale, and tape measure with confirmed accuracy. All children aged 6 - 12 years were included in the study. Children who did not want to cooperate, had the severe disease in the last months, and had weight loss were excluded from the study.
For children, BMI is presented as a percentile, which plots the child's BMI next to other children's BMI of the same age and sex. The BMI between the fifth and 85th percentiles is considered normal and healthy. Falling below the fifth percentile is considered underweight. Falling between the 85th and 95th percentiles is considered overweight, and more 95th percentile is considered obesity. If BMI is more than the 120th percentile, it is considered excessive obesity (11).
Descriptive statistics, mean and standard deviation, were used to describe the data. Pearson's and Spearman's correlation coefficients in SPSS version 25 software were used to analyze the data. The Kolmogorov-Smirnov test was used to check the normality of the data. We used the Mann-Whitney U test to test the average height, weight, and BMI based on gender. The Kruskal-Wallis test was used to analyze arm circumference based on BMI class (P < 0.05). Receiver operating characteristic (ROC) curve was used to determine the cutoff points on the graphs. According to previous studies, the best area was placed below 0.1-0.9 on the ROC curve (12). Finally, the Youden index was used to evaluate the sensitivity and specificity of the cutoff point on the ROC curve (13).
4. Results
We collected and analyzed the data of 455 students aged 6 - 12 years, including 278 (61.1%) girls with an average age of 9.19 ± 1.8 years and 177 (38.9%) boys with an average age of 8.15 ± 1.6 years. The average height was 135 ± 12 cm, the average weight was 31.85 ± 11.2 kg, the average MUAC was 21 ± 3.1 cm, and the average BMI was 17 ± 3.6 kg/m2 (Table 1).
| Minimum | Maximum | Mean ± SD | |
|---|---|---|---|
| Age (y) | 6 | 12 | 8.79 ± 1.80 |
| Height (cm) | 106 | 165 | 135.05 ± 12.03 |
| Weight (kg) | 15 | 68 | 31.85 ± 11.2 |
| MUAC (cm) | 15 | 31 | 20.94 ± 3.15 |
| BMI (kg/m2) | 11.54 | 30.18 | 17.03 ± 3.62 |
Most children (73.7%) had normal BMI, which was 71.9% and 69.5% in girls and boys, respectively. The distribution of BMI was higher in girls than in boys. The distribution of BMI was significantly different among girls (P = 0.034), while both underweight and obesity were reported more in boys than in girls (Table 2).
| Sex/BMI | No. (%) |
|---|---|
| Female | |
| Underweight | 44 (15.8) |
| Normal weight | 200 (71.9) |
| Overweight | 18 (6.5) |
| Obese | 16 (5.8) |
| Male | |
| Underweight | 31 (17.5) |
| Normal weight | 123 (69.5) |
| Overweight | 9 (5.1) |
| Obese | 14 (7.9) |
In both groups of girls and boys, there was a significant and direct correlation between age and height, age and weight, age and MUAC, age and BMI, height and weight, height and MUAC, height and BMI, weight and MUAC, weight and BMI, and MUAC and BMI (Table 3). There was a significant difference between the mean height of girls and boys, and girls were significantly taller than boys (P < 0.05).
| Variables | Age | Height | Weight | MUAC | BMI |
|---|---|---|---|---|---|
| Female | |||||
| Age | 1 | 0.855* | 0.728* | 0.577* | 0.467* |
| Height | 0.855* | 1 | 0.862* | 0.702* | 0.581* |
| Weight | 0.728* | 0.862* | 1 | 0.894* | 0.893* |
| MUAC | 0.577* | 0.702* | 0.894* | 1 | 0.878* |
| BMI | 0.467* | 0.581* | 0.893* | 0.878* | 1 |
| Male | |||||
| Age | 1 | 0.797* | 0.633* | 0.371* | 0.200* |
| Height | 0.797* | 1 | 0.840* | 0.526* | 0.351* |
| Weight | 0.633* | 0.840* | 1 | 0.744* | 0.772* |
| MUAC | 0.371* | 0.526* | 0.744* | 1 | 0.708* |
| BMI | 0.200* | 0.351* | 0.772* | 0.708* | 1 |
a * There is a correlation (P < 0.001)
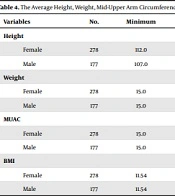
The average weight was significantly higher in girls than boys (P < 0.05). The BMI was significantly higher in girls than boys (P < 0.05), and there was no significant difference between the mean MUAC of girls and boys in the same age group (P > 0.05) (Table 4).
| Variables | No. | Minimum | Maximum | Mean ± SD | Mann-Whitney (P-Value) |
|---|---|---|---|---|---|
| Height | < 0.001 | ||||
| Female | 278 | 112.0 | 165.0 | 137.47 ± 12.50 | |
| Male | 177 | 107.0 | 157.0 | 131.25 ± 10.16 | |
| Weight | < 0.001 | ||||
| Female | 278 | 15.0 | 68.0 | 33.77 ± 12.01 | |
| Male | 177 | 15.0 | 64.0 | 28.82 ± 8.92 | |
| MUAC | 0.34 | ||||
| Female | 278 | 15.0 | 31.0 | 21.22 ± 3.28 | |
| Male | 177 | 15.0 | 30.0 | 20.50 ± 2.87 | |
| BMI | 0.011 | ||||
| Female | 278 | 11.54 | 28.85 | 17.41 ± 3.78 | |
| Male | 177 | 11.54 | 30.18 | 16.44 ± 3.25 |
There was a significant difference between BMI and MUAC in both sexes (P < 0.001).
The ROC curve was used to determine the cutoff point, and the Youden index was used to evaluate the sensitivity and specificity of the cutoff point on the ROC curve. The area below the ROC curve for underweight and normal weight was less than 0.6, which means the MUAC in these two ranges cannot predict BMI.
The ROC curve was acceptable for BMI in the overweight range (the area below the curve was 0.834), and the results were very desirable in the obesity range among girls (the area below the chart was 0.958).
The ROC curve was acceptable for BMI in the overweight range (area below chart was 0.908), and the results were very desirable in the obesity range (area below chart was 0.938) in boys.
The cutoff point of MUAC was 23.75 cm in the overweight BMI (77% sensitivity and 80% specificity) and 24.75 cm in the obesity range (93% sensitivity and 88% specificity) in girls aged 6 - 12 years. The cutoff point of MUAC was 22.25 cm in overweight BMI (88% sensitivity and 83% specificity) and 25.25 cm in the obesity range (87% sensitivity and 90% specificity) in boys aged 6 - 12 years (Table 5).
| BMI | ROC | Youden Index | SD | Sensitivity | Specificity | MUAC |
|---|---|---|---|---|---|---|
| Overweight | ||||||
| Female | 0.834 | 0.582 | 0.031 | 0.778 | 0.804 | 23.75 |
| Male | 0.908 | 0.728 | 0.025 | 0.889 | 0.839 | 22.25 |
| Obese | ||||||
| Female | 0.958 | 0.82 | 0.014 | 0.938 | 0.882 | 24.75 |
| Male | 0.938 | 0.78 | 0.032 | 0.875 | 0.905 | 25.25 |
5. Discussion
Based on the present study, the correlation between all variables was significant (age and height, age and weight, age and MUAC, age and BMI, height and weight, height and BMI, weight and MUAC, weight and BMI, and MUAC and BMI) in both groups of girls and boys.
Determining the MUAC cutoff point from the ROC curve was not significant in children with underweight or normal weight, while in both sexes, it was significant in the range of overweight and obesity. A study in Pakistan on children aged 12 - 18 years showed that MUAC is a good indicator for screening obesity (14), so the results are similar to our study, but the age groups are different. The study on Polish school children (aged 7 - 18 years) indicated that MUAC was more accurate for screening than BMI (15). In that study, the researchers suggested MUAC as a socioeconomic predictor (15), which is somehow different from our study.
Another study in Nepal on adults showed that MUAC is a good tool for screening the underweight (16). Also, the age group and MUAC predicted the underweight, which is different from our study, but like our study, it showed the importance of MUAC. Also, a study in India explained the importance of MUAC in school-aged children as a predictor of BMI (17).
Measuring mid-upper arm circumstances is more straightforward than BMI estimation. Therefore, we recommend MUAC as a predictor of early diagnosis of overweight and obesity, especially for families, as a practical and cost-effective method.