1. Background
Scaphoid bone fracture is the most common fracture of the wrist (1-4). Its overall incidence is 2% to 3% of all fractures. About 60% to 80% of the cases occur in the middle part, usually between 25 and 35 years old, being more common in men. Its mechanism is falling on an outstretched hand, usually during exercise (5).
Since the scaphoid bone has no tendon attachment and has limited attachments to the ligaments, it has poor periosteal perfusion. About 80% of its surfaces are covered with articular cartilage, and its special circulation from the distal to the proximal is retrograde by fine arteries. Delicate perfusion and fewer soft tissue attachments make it susceptible to nonunion and necrosis (5).
Unfortunately, many cases of scaphoid fractures are not visible enough in early radiography. Therefore, they might not be detected and treated on time. Factors affecting the union include delayed treatment, fracture displacement, more proximal fracture, and smoking. Patients with nonunion usually refer late for treatment, often looking for signs of a recent fall (5).
There are two types of nonunion, including fibrous union, which is stable, and an unstable type that can have degenerative changes (6, 7). Since this fracture is more common in young men, its morbidity can affect the community's active population; hence, being unable to work and other economic problems are added to the costs of treatment (6). Nonunion is defined as the absence of bone trabeculation in radiological studies after six months of treatment (1). The prevalence of scaphoid nonunion is 12% and may eventually lead to complications such as deformity and instability (2, 3, 5, 8), degenerative changes (6, 7, 9-14), and symptomatic clinical cases requiring treatment (15-17).
The most commonly used treatment is open surgery, with an 84% success rate when used simultaneously with fixation and about 80% success rate when done alone, with a failure rate of 25% to 40% (9). The preferred surgical approach for open standard treatment is Palmar unless there is a proximal fracture or evidence of necrosis. In this approach, the Palmar branch of the radial artery should be ligated when opening the capsule, worsening the scaphoid's fine blood flow (1, 6, 7). In arthroscopic surgery, this damage is minimized, and according to our hypothesis, there can be better union and clinical results (1, 6, 14, 17, 18).
Open surgery has undesirable consequences, such as damage to soft tissue, small blood vessels, ligaments, rvola capsules, and delayed rehabilitation (6, 7). In arthroscopic surgery, we have a direct vision to meticulously restore the alignment of articular surfaces and detect accompanying damage besides the less soft tissue and vessel damage (6, 7, 18).
2. Objectives
In this study, we present the radiographic and functional results and complications of arthroscopic treatment of scaphoid nonunion in an organized manner.
3. Methods
This case series study was conducted on symptomatic patients with isolated and non-complicated scaphoid nonunion. Fifteen patients with a mean age of 29 years were operated on from October 2015 to October 2016 in Besat hospital in Hamadan city. The study was approved under the ethical approval code of IR.UMSHA.REC.1395.38 by the Hamadan University of Medical Sciences institutional review board. All patients signed informed consent before participation. A highly experienced surgeon with the number 4 level of expertise (the first author with more than 10 years of experience in wrist arthroscopy) did all the surgeries. The exclusion criteria included having: (1) a history of injury, fracture, and pathology in the operated wrist; (2) the presence of a fracture or injury other than scaphoid bone; (3) vascular necrosis; and (4) degenerative changes deformity and instability.
The patients were monitored with simple radiography and, if necessary, with a computed tomography scan or magnetic resonance imaging (MRI) before surgery, one week, three months, and one year after surgery. We followed the patients for one year to assess unionization (based on imaging methods) and function, including the range of active motion (the angle between the forearm and the third metacarpal by a goniometer) and grip strength (with a Jamar dynamometer). We also completed the standard disability questionnaires: Disabilities of the arm, shoulder, and hand (DASH), patient-related wrist evaluation (PRWE), and modified Mayo wrist scales. The surgical complications were also carefully noted.
3.1. Surgical Technique
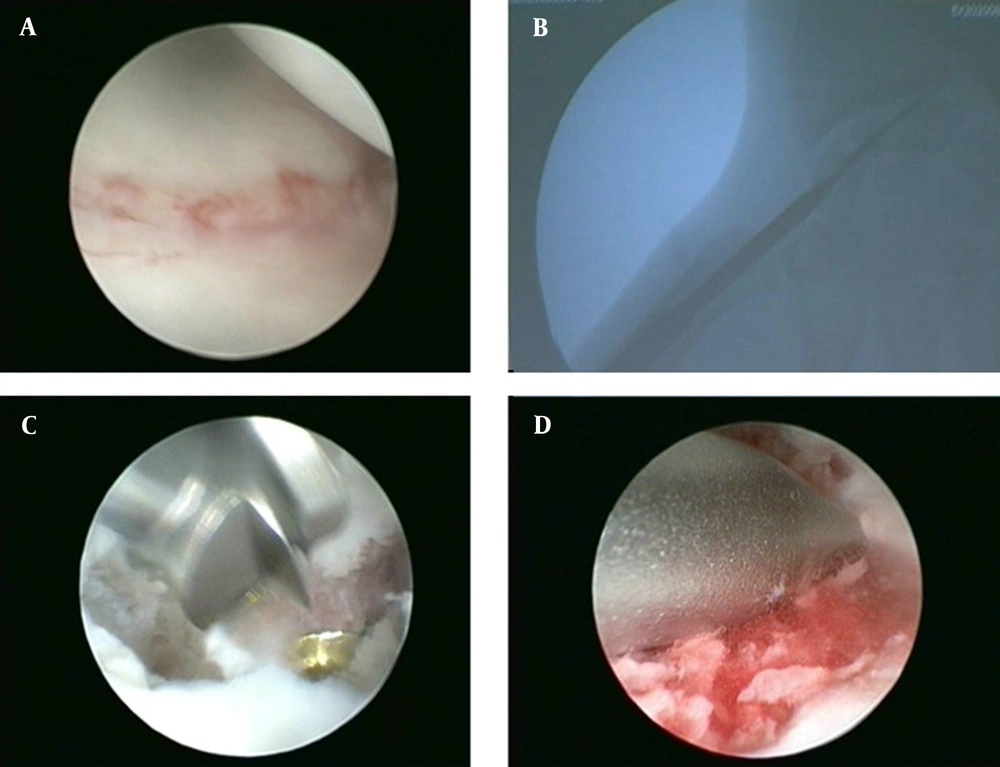
Under general anesthesia, we placed a tourniquet on the arm and applied counter traction. A traction tower was used to apply traction. Chinese finger traps were used to apply the required traction of 30 N to 50 N. At the beginning of all the wrist arthroscopy procedures, we did a radiocarpal assessment using 3 - 4 and 6 R portals. Following the radiocarpal diagnostic arthroscopy, we inserted the scope through the ulnar mid-carpal portal to visualize the scaphoid nonunion (Figure 1A). Then, the place of the nonunion was cleaned and debrided with a shaver and was refreshed by burr using a radial midcarpal portal (Figure 1B).
Then, the perfusion of the proximal segment was examined after the temporary removal of the tourniquet based on the presence or absence of punctate bleeding. Afterward, two fracture segments were connected with two percautaneous pins and were reduced by traction maneuver, extension, and supination, while we assessed the joint surface reduction from an arthroscopic view.
After reduction, the pins were driven to the next fragment under fluoroscopic control for temporary fixation and a guide for Herbert screw insertion. Then, we drilled through the cannulated drill bite on the pin, and the fixation with the Herbert screw was applied (Figure 1C), but it was not fastened until the cancellous graft was harvested from the distal radius and inserted in the fresh nonunion side using a Jamshidi bone marrow biopsy needle (Figure 1D). Afterward, the weight was removed so that bone grafts rested in the nonunion site by distal carpal bones. The screw was firmly tightened. After the surgery, the wrist was kept in a thumb Spica cast for four to six weeks. Then, the range of motion and physio-therapy started and continued for up to six weeks if necessary.
4. Results
There were 15 patients in this study. They were all men with a mean age of 29 years. The interval between the initial trauma and surgery was an average of 12 months. Among them, 12 patients had fractures in the dominant hand and three in the non-dominant hands. Regarding the trauma mechanism, 12 patients had scaphoid fractures due to falling and three patients due to direct trauma. Regarding the anatomical location of the fracture, 10 patients had scaphoid waist fractures, while in five patients, it was in the proximal pole. Four of them were smokers.
According to the simple radiographic findings, the fracture was satisfactorily united after three months in all patients. No patient had complications directly associated with the surgical procedures, such as surgical site infection or sensory impairment. Regarding function, the means of a range of motion and wrist strength were compared in two parameters, including grip and pinch with the opposite hand (Table 1).
| Outcome | Affected Side | Contralateral Side |
|---|---|---|
| Extension mean (degree) | 59.58 | 72.91 |
| Flexion mean (degree) | 59.16 | 81.66 |
| Radial deviation mean (degree) | 22.08 | 25.83 |
| Ulnar deviation mean (degree) | 35.83 | 42.08 |
| Grip strength (kg) | 35.08 | 39.75 |
| Pinch strength (kg) | 11.7 | 13.04 |
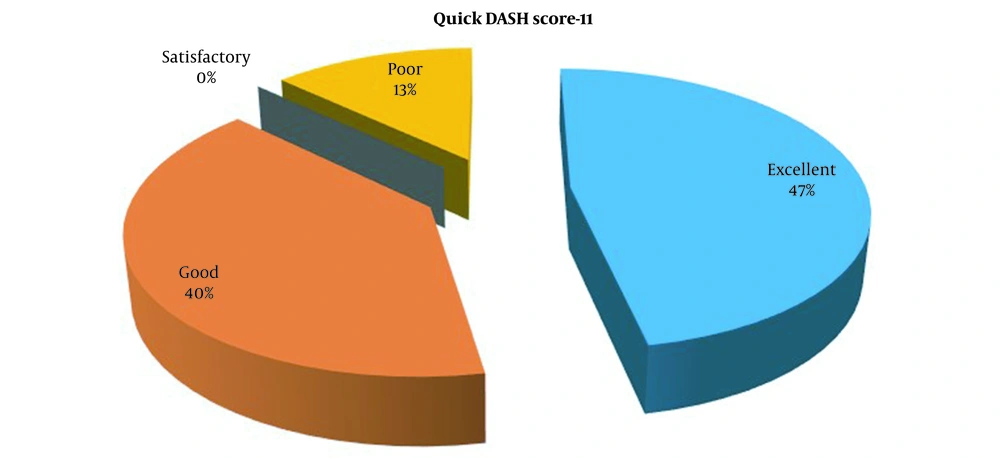
Wrist function was assessed with standard questionnaires. According to the DASH questionnaire, the patients' satisfaction rate was 47% excellent, 40% good, and 13% weak. Overall, the average score was 13.54, equivalent to good function (Figure 2).
According to the PRWE questionnaire, the mean patient satisfaction score was 16.11. The two scoring systems are designed based on the patient's satisfaction with the treatment and are answered exclusively by them subjectively (Table 2).
| Score | Mean |
|---|---|
| Quick DASH-11 | 13.54 (good) |
| PRWE | 16.11 |
| Mayo | 77.66 (satisfactory) |
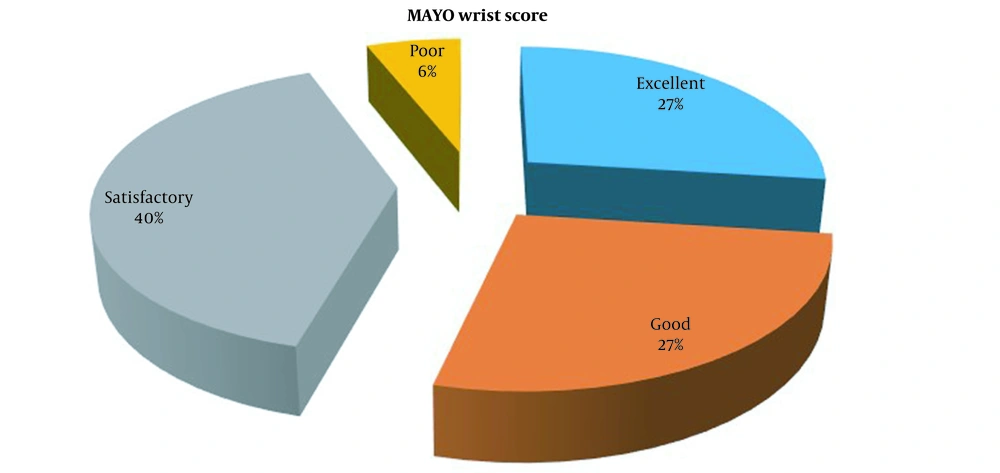
The Mayo scoring system evaluated the performance of the wrist. Of the patients, 27% had excellent, 27% good, 40% satisfactory, and 6% poor outcomes. This system evaluates the patient's objective and includes examination parameters (Figure 3).
5. Discussion
Treatment of scaphoid nonunion is complex and requires experience (5, 6). The typical surgical treatment is an open surgery with its own complications, including damage to the scaphoid's small blood vessels (6, 7). It is assumed that an arthroscopic surgical technique, thanks to less manipulation of the soft tissue of the area, not only reduces these injuries but also provides a direct, accurate, and magnified view of restoring the alignment of the extensive articular surfaces of this bone, contributing more to better reconstruction (6).
On the other hand, we know that 60% of extension-flexion movements, the most important motion in the wrist, occur on the surface of the radiocardial joint. In open approaches to scaphoid nonunion, the radiocarpal surface of the scaphoid is exposed, and preparing the nonunion site in this surface may induce some damage. However, in the arthroscopic method, we enter via the intercarpal articular surface, which has a more pronounced role in radial and ulnar deviation (6, 7).
In this study, we treated 15 patients with scaphoid nonunion with arthroscopic methods and evaluated their functional and radiological results were evaluated. After three months, according to simple radiographic evidences, all scaphoids were satisfactory united, and direct complications of surgical procedure, such as surgery site infection or sensory impairment, were not observed in any of the visits.
Slade et al. operated 15 patients with scaphoid nonunion using arthroscopic treatment. Of them, 13 had excellent, and three had good functional results. On average, within 14 weeks, all patients had an adequate union. They did not mention the number of complications (15).
Slade and Gillon published a review of 108 consecutive cases of scaphoid nonunion treated arthroscopically. They concluded that this treatment method is effective and safe. On average, 96% of the patients had good healing within 22 weeks. The rate of complications was 9%, which was mainly a site infection (18).
Kim et al. achieved an 86% union rate by examining 36 patients who had undergone arthroscopic surgery. They found that arthroscopic surgery positively affected the function of patients with scaphoid nonunion. Their patients did not experience any complications associated with the surgical procedure (16).
Kang et al. treated 33 patients who did not have deformity, necrosis, or arthritis after arthroscopic treatment. They showed that in terms of function, the changes were positive compared to before surgery, and the patients were in good condition. They reported that 97% of the union was successful and had no complications related to the surgical procedure (17).
In our study, one surgeon did all the surgeries to reduce the rate of error. Fortunately, union in the first trimester of surgery demonstrates the success of this method as the most important goal of treatment, and besides its uncomplicated, its value is more prominent. Functional results based on standard questionnaires also show the effectiveness of this treatment method in achieving desirable outcomes. Perhaps if there was a control group treated with open surgery, the difference in the results would be more apparent.
An issue considered in judging the performance results based on standard questionnaires was the subconscious use of the affected hand compared to the other. For example, in the case of multiple essential questions in the questionnaires, the patients had considered their healthy hands in that particular function due to adaptation to the condition, especially if the non-dominant hand was involved. Therefore, they had fewer complaints, which might be the reason for a large percentage of differences between the scores of patient and physician response assessment systems.
5.1. Conclusions
Arthroscopic treatment of scaphoid nonunion seems to be an effective method with low complications and favorable results. The ultimate goal of treating this disease is to prevent degenerative changes in the wrists. We recommend doing a prospective long-term study that can provide a more realistic picture of its long-term outcomes. Small sample size and lack of long-term follow-up were some of the limitations, similar to the previous studies on this subject.