1. Background
The cause of COVID-19 is a coronavirus belonging to the beta coronavirus group (1). This virus is one of the major pathogens that primarily target the human respiratory system and cause pneumonia-like symptoms (2), and even may involve the digestive system (3). This coronavirus was first discovered in Wuhan, China, in 2019 and spread worldwide (4). The related disease inflicts both humans and animals and causes respiratory involvement and lung damage. This virus has a high human-to-human transmission rate (5). According to the latest World Health Organization report, globally, 621 million people were infected with COVID-19, and 6.5 million died up to October 16, 2022 (6).
This disease is associated with symptoms such as fever, dry cough, and fatigue in 80% of cases (7). The severity of the disease is related to individuals' age and comorbidities, and those severely affected by the coronavirus are admitted to the intensive care units (ICU) (8). About 80% of cases are asymptomatic or experience mild disease symptoms. Another 15% become seriously ill and will need oxygen and are hospitalized. Ultimately, 5% need ventilators and are kept in intensive care units (9). Furthermore, many people with COVID-19 suffer from different symptoms after recovery, similar to the initial COVID-19 symptoms, such as weakness, fatigue, anxiety, and depression (10). Post-covid symptoms occur in 90% of cases, with clinical presentations ranging from mild symptoms such as headaches to severe incidents such as stroke (10). In mild cases, COVID-19 symptoms which may last up to two weeks and even three to six weeks or more in severe cases (11). Therefore, national health systems should develop specific strategic plans for patients with long covid and its consequences (12).
With the spread of COVID-19, the World Health Organization declared it a pandemic and considered preliminary public health measures to control it, including banning unnecessary outdoor activities such as sports and recreational activities, limiting access to parks and playgrounds, and imposing a quarantine on those who may be infected, as well as social distancing and avoiding social gatherings, limiting contact with older people and those with feeble health (13). Using these public health measures, citizens faced changes in behavior, physical activity level, and different dimensions of daily activities. Nonetheless, the health priority was avoiding the disease; low levels of physical activity and a sedentary lifestyle had their own consequences and imposed the risk of deteriorating their health due to chronic diseases (14). Therefore, the establishment of occupational balance for COVID-19 survivors to return to their everyday life as soon as possible should be a priority.
Occupational balance is considered a fundamental concept in rehabilitation, especially in occupational therapy (15). Occupational balance, which is an individual and subjective concept, is defined as having a proper fit and balance both in terms of quantity and variety between performing various activities needed and enjoyed by individuals, such as work, self-care, leisure, socialization, and rest (16). These activities have a pattern and personal value and importance in life. Occupational balance can be considered from three aspects: First, the time spent on activities; second, the type of activities and their characteristics; and third, major life activities (17). A proper occupational balance is defined as one of the health aspects that has a positive and meaningful relationship with the satisfaction and quality of life (18). Occupational imbalance, which is defined as the inability to participate in the desired or interesting activities, doing too much of one or more limited activities, or inability to perform activities properly, reduces not only the life quality and satisfaction but also causes mood changes such as depression and anxiety (19). A wide range of personal problems, such as physical, cognitive, and psychological disabilities, and environmental and social problems, such as the lack of access to facilities to perform necessary activities, can affect occupational balance (20). Disruption in the daily routine by causes such as COVID-19 can lead to anxiety and depression (9).
Given the clinical conditions caused by long-term immobility and skeletal and muscular problems, these patients need rehabilitation interventions after hospital discharge. Particularly, when patients still have breathing or movement problems, they should continue their rehabilitation programs in specialized rehabilitation departments to increase their chances of recovery. If the COVID-19 complications are low and patients are at home, they may need home or outpatient rehabilitation. In these cases, major rehabilitation is done to restore motor skills and improve the mental status of these people. In both cases, the rehabilitation program should be based on specific patient disorders (21). As mentioned, the balance between individuals' daily activities and life patterns has changed during the COVID-19 pandemic; hence, there is a need for new interventions for this group of people (22). Several studies have examined the importance of occupational balance in COVID-19 patients, including a review study on occupational dimensions and the status of rehabilitation in COVID-19 patients (1) and the effect of inactivity caused by COVID-19 on the motor performance of older people (23), postural balance and its effect on the performance of non-hospitalized patients with COVID-19 (24), and the effect of mild COVID-19 on the occupational balance of young people (25).
2. Objectives
No study has compared hospital-discharged COVID-19 survivors with healthy people. Therefore, the aim of this study was to address this gap.
3. Methods
The present cross-sectional study was conducted from March to August 2022 at Imam Reza Military Hospital. The research population consisted of hospital-discharged COVID-19 survivors and healthy individuals. The inclusion criteria of COVID-19 survivors were as follows: Age of 18 - 70 years, history of hospitalization for COVID-19 at least one night (according to medical records), and 1 to 3 months should have passed after the discharge. The inclusion criteria for healthy people were as follows: No records of COVID-19 (or having a mild asymptomatic infection without hospitalization). Exclusion criteria of both groups included not completing the questionnaires, diseases with long-term and debilitating effects such as stroke, or progressive diseases such as Parkinson's disease, history of psychiatric disorders such as depression and chronic anxiety, hospitalization in the ICU, having acute medical problems before hospitalization, having hearing problems, having cognitive performance problems to understand questions, and inability to answer the questions. In the hospital-discharged COVID-19 survivors, a systematic random sampling method was used to select the cases. The cases were selected with a combination of the following three methods according to their feasibility for each person for selection of the healthy control group. First, sibling control, second, friend control, and third, neighborhood control with the condition that chosen cases should not have a history of hospitalization due to COVID-19. Furthermore, the gender of hospitalized and healthy people was matched. The caliper matching was done in all three methods so that those selected as the healthy group had a maximum age range of five years (five years older or younger) with cases in the hospitalized COVID-19 group. The sample size was calculated based on the confidence level (α = 0.05) and the test power (80%) (26). Based on this, 140 individuals were included in the study in two groups of 70.
3.1. Data Collection Tools
Occupational Balance Questionnaire (OB-Quest): This questionnaire included ten self-report questions based on seven components of occupational balance, and each question has a three-point scale. The questionnaire measures the individuals' understanding of the quantity and variety of their daily activities and is in the range of 10 (high occupational balance) to 30 (low occupational balance) (15). In the Chinese version, good validity and reliability were obtained (test-retest reliability with a Cronbach's alpha coefficient of 0.80 (27). A score of 17 to 30 was considered imbalance and difficulty in occupational balance, 17 to 23 was considered moderate, and 23 to 30 indicated a severe occupational imbalance. A score under 17 was considered a good occupational balance (10 to 16 was a good occupational balance). The questionnaire had good internal consistency, content validity, and test-retest reliability (28).
Hospital Anxiety and Depression Scale (HADS): This scale includes 14 questions that examine depression and anxiety. Seven questionnaire questions are related to depression, seven are related to anxiety, and they are scored from 0 to 3. The score of each section is between 0 and 21. A higher score indicates a greater level of depression or anxiety. A cut-off point of +8 for both depression and anxiety states the presence of anxiety or depression. The questionnaire has acceptable validity and reliability (a Cronbach's alpha of 0.78 for anxiety and 0.86 for depression) (29).
Fatigue Severity Scale (FSS): This questionnaire is used to determine the severity of fatigue. The FSS has nine items under which the individuals select the degree of agreement with each term (1 = strongly disagree, 7 = strongly agree). The total score of the questionnaire is in the range of 9 to 63, and a higher score indicates higher fatigue. The cut-off point of the questionnaire is 36, and a higher score indicated the presence of pathological fatigue. This instrument is very popular due to its ease of use, comprehensibility, and short time needed for completion. It also has excellent validity and reliability (a Cronbach's alpha of 0.93) (30).
3.2. Data Collection Method
After receiving the recommendation letters, the eligible samples were selected from Imam Reza Military Hospital based on the inclusion criteria. Before sending the questionnaire to individuals, they were contacted and received information about the study, and then they received the electronic questionnaire designed by the Google Form program. The research aims and objectives were explained at the beginning of the electronic questionnaire. The questions of the electronic questionnaire included the demographic characteristics of the patients, the severity of the disease, the number of hospitalization days, and OB-Quest questions (n = 10), HADS questions (n = 14), and FSS questions (n = 9). The time needed to answer the questions and complete the questionnaire was approximately 20 - 30 minutes.
3.3. Data Analysis Method
For the analysis of the data, SPSS22 was used to determine descriptive statistics (frequency, percentage, and standard deviation), and analytical statistics were used to analyze the data. Furthermore, the Mann-Whitney U test, Pearson correlation coefficient, and t-test were used to compare occupational balance, anxiety, fatigue, and depression between the two groups, namely the hospital-discharged COVID-19 survivors and healthy people.
3.4. Ethical Considerations
The present research was approved by the Research and Technology Deputy of the Military University of Medical Sciences with an ethical code IR.AJAUMS.REC.1400.294. The research process and the individuals' roles in the research were described in the electronic questionnaire. If needed, people could contact the researcher for any questions or receive the results of the questionnaire and research. The participants were assured that their information would remain confidential.
4. Results
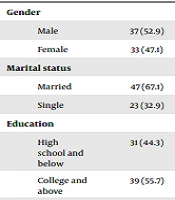
Table 1 presents the demographic characteristics of hospital-discharged COVID-19 survivors and healthy people.
| Variables | Covid-19 Group (n = 70) | Healthy Group (n = 70) | P-Value |
|---|---|---|---|
| Gender | |||
| Male | 37 (52.9) | 38 (54.3) | 0.865 |
| Female | 33 (47.1) | 32 (45.7) | |
| Marital status | |||
| Married | 47 (67.1) | 44 (62.9) | 0.595 |
| Single | 23 (32.9) | 26 (37.1) | |
| Education | |||
| High school and below | 31 (44.3) | 21 (30) | 0.482 |
| College and above | 39 (55.7) | 49 (70) | |
| Employment status | |||
| Employed | 43 (64.4) | 39 (55.7) | 0.492 |
| Unemployed | 27 (35.7) | 31 (44.33) | |
| Income | |||
| Above 10 m | 38 (54.3) | 39 (55.7) | 0.053 |
| Under 10 m | 32 (45.7) | 31 (44.3) | |
| Comorbidities | |||
| Yes | 30 (42.9) | 29 (41.4) | 0.864 |
| No | 40 (57.1) | 41 (58.6) |
Demographic Characteristics of Participants a
According to Table 1, most of the participants in both COVID-19 and healthy groups were male (54.3% vs. 52.9%), married (62.9% vs. 67.1%), had college degrees and higher (70% vs. 55.7%), were employed (55.7% vs. 64.4%), had an income level below 10 million tomans (55.7% vs. 54.3%), and had no underlying disease (58.6% versus 57.1%). The results indicated no difference between the two groups in terms of demographic characteristics (P > 0.05).
According to Table 2, most COVID-19 survivors were in the age range of 40 to 49 years, while the healthy cases group was in the age range of under 30 years.
According to Table 3, the COVID-19 survivors experienced higher anxiety (55.7%) and fatigue than healthy people, and the rate of depression in participants with COVID-19 was higher than in the healthy subjects. Participants with COVID-19 had a more impaired occupational balance at moderate (48.6%) and severe (21.4%) levels. However, the occupational balance of healthy individuals was at a good level (62.8%). The degree of occupational balance impairment was classified into three levels: Severe, moderate, and good, and the severe and moderate levels indicated occupational balance impairment.
| Variables | Covid-19 Group (n = 70) | Healthy Group (n = 70) |
|---|---|---|
| Depression | ||
| Yes | 32 (45.7) | 4 (5.7) |
| No | 38 (54.3) | 66 (94.3) |
| Anxiety | ||
| Yes | 39 (55.7) | 10 (14.3) |
| No | 31 (44.3) | 60 (85.7) |
| Fatigue | ||
| Yes | 54 (77.1) | 17 (24.3) |
| No | 16 (22.9) | 53 (75.7) |
| Occupational imbalance | ||
| None | 21 (30) | 44 (62.8) |
| Moderate | 34 (48.6) | 23 (32.8) |
| Severe | 15 (21.4) | 3 (4.4) |
Frequency and Percentage of Depression, Anxiety, Fatigue, and Occupational Balance Level in the Participants a
Table 4 indicates that the mean prevalence of depression (8.46 ± 3.78 versus 4.29 ± 2.91), anxiety (9.34 ± 4.38 versus 4.46 ± 3.09), and fatigue (44.29 ± 10.02 vs. 28.49 ± 9.87) were higher in COVID-19 survivors than in the healthy individuals. The lack of occupational balance in COVID-19 survivors was also higher than the healthy individuals (19.03 ± 4.16 vs. 15.32 ± 32). The results indicated that there was a significant difference between the two groups in terms of depression, anxiety, fatigue, and lack of occupational balance (P = 0.001).
| Variables and Group | Mean ± SD | P-Value |
|---|---|---|
| Depression score | < 0.001 | |
| Healthy | 4.29 ± 2.91 | |
| Covid-19 | 8.46 ± 3.78 | |
| Anxiety score | < 0.001 | |
| Healthy | 4.46 ± 3.09 | |
| Covid-19 | 9.34 ± 4.38 | |
| Fatigue score | < 0.001 | |
| Healthy | 28.49 ± 9.87 | |
| Covid-19 | 44.29 ± 10.02 | |
| Occupational balance score | < 0.001 | |
| Healthy | 15 ± 3.32 | |
| Covid-19 | 19.03 ± 4.16 |
Depression, Anxiety, Fatigue, and Occupational Balance Scores in Individuals with COVID-19 Compared to Healthy Cases
According to Table 5, the level of depression and anxiety (r = 0.773) had a direct correlation with the lack of occupational balance (moderate and severe levels) (r = 6.77). The incidence of anxiety and fatigue with depression (r = 0.773 in both variables) had a higher correlation with the lack of occupational balance (r = 585 versus r = 521). Lack of occupational balance was also correlated with depression (r = 677) and anxiety (r = 585) more than fatigue (r = 521).
| Depression | Anxiety | Fatigue | Occupational Imbalance | |
|---|---|---|---|---|
| Depression | ||||
| Pearson correlation | 1 | 0.773 | 0.500 | 6.77 |
| Sig. (2-tailed) | - | 0.000 | 0.000 | 0.000 |
| Anxiety | ||||
| Pearson correlation | 0.773 | 1 | 0.457 | 0.585 |
| Sig. (2-tailed) | 0.000 | - | 0.000 | 0.000 |
| Fatigue | ||||
| Pearson correlation | 0.773 | 0.457 | 1 | 0.521 |
| Sig. (2-tailed) | 0.000 | 0.000 | - | 0.000 |
| Occupational balance | ||||
| Pearson correlation | 0.677 | 0.585 | 0.521 | 1 |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | - |
Intergroup Correlation Between Depression, Anxiety, Fatigue, and Occupational Balance Scores in Cases with COVID-19
5. Discussion
Despite the high prevalence of COVID-19 and the abundance of studies in this field, the occupational balance, which is a fundamental concept of occupational therapy, and problems and complications of COVID-19 patients, especially hospital-discharged COVID-19 survivors, have remained understudied. In other words, this research was the first study on occupational balance and activities from an occupational therapy perspective. The results demonstrated a decrease and lack of occupational balance in the hospital-discharged COVID-19 survivor group compared to the healthy individuals. Furthermore, additional problems such as depression, anxiety, and fatigue were also seen in hospital-discharged COVID-19 survivors. The healthy cases did not show any fatigue, anxiety, and depression, possibly owing to extensive vaccination and reduction of COVID-19 restrictions during the study.
Lack of occupational balance was also correlated with depression more than fatigue. The results indicated that the scores of the hospital-discharged COVID-19 survivors’ group were significantly higher than those of healthy controls, indicating a lower occupational balance in hospital-discharged COVID-19 survivors. The occupational balance in daily life activities indicated health. In this regard, Rodriguez-Rivas et al. reported that at least half of the individuals' daily life was disrupted, and their range of activities decreased due to COVID-19. This result is consistent with the general results of the present study (31).
The discharge of COVID-19 patients does not indicate their complete recovery and the end of their follow-up period. Long-term monitoring of these patients and different mental and physical health evaluations, and the assessment of their daily life performance is essential for their complete recovery and high quality of life. Therefore, the more accurate and comprehensive the evaluation is, the timelier interventions can be made according to the symptoms and complications. Therefore, ongoing contact with the patients, counseling services, and drug therapy can alleviate complications (32). Since the creation and maintenance of balance between different occupational activities is important for health, there is a need for more systematic evaluations to examine each occupational domain accurately through interviews. These evaluations can provide a correct understanding of the needs and resources to solve future problems and reduce the financial costs of the disease, with the consequence of easing the burden on national health systems.
In a study conducted two months after COVID-19hospitalization, Mendez et al. concluded that 58% of people had at least a moderate reduction in cognitive function, indicating that individuals had problems with occupational balance and could not solve problems and perform high-level cognitive activities such as executive functions (33). These results can justify the increase in an occupational imbalance during one to three months after hospitalization in the present study, while occupational balance did not decrease in healthy individuals. Therefore, the activity patterns and the balance between them were related to individuals' mental and physical health (34).
The results indicated that hospital-discharged COVID-19 survivors experienced more fatigue, anxiety, and depression than the healthy controls. In this regard, Wu et al. reported that there was a relationship between infectious diseases and mental stress and its consequences. Fatigue, anxiety, and depression, which can be caused by hospitalization (e.g., people experience fear during admission, hospitalization, and being labeled), may lead to different mental health issues (9). Another study similarly indicated that the occupational imbalance could be due to COVID-19 and its consequences or due to fatigue, anxiety, and depression (35).
In the case of the SARS virus, a four-year follow-up study indicated that chronic fatigue and psychiatric problems remained in the cases (36). Another study reported that psychiatric symptoms in people with Alzheimer's disease increased and significantly worsened five weeks after being infected with COVID-19 (37). Another study reported fatigue in half of the patients who recovered from SARS after three months (38). Islam et al. observed a direct relationship between the severity of COVID-19 consequences and the severity of its outbreak (10). Therefore, there was an inverse relationship between depression and occupational balance.
According to the content mentioned above, it is necessary to conduct more studies on the intensity and mechanisms of fatigue in activities and its remedies. For example, the energy-saving technique, which means prioritizing tasks during the day, is a method to control fatigue. Furthermore, improving mental health and maintaining the occupational balance after hospitalization due to COVID-19 can be achieved through increasing social support (39) and emotional support from the family, daily planning, performing valuable personal and social activities, high work activity levels, exercise, and doing regular physical activities (34). Various studies indicate that people who had problems due to their daily activity patterns, could regain their occupational balance only by making changes in daily activity patterns, the way of performing activities, and prioritizing them. Therefore, occupational balance is a relative state that can change according to life and personal conditions (40-42).
Given the cross-sectional nature of this study, the results, which were conducted within one to three months after discharge from the hospital, did not demonstrate the underlying mechanism of the relationship between the research variables. Furthermore, the limited number of participants may not have obtained accurate results, and therefore, a larger sample size with more participant diversity might lead to different results. If the participants had low levels of anxiety, depression, and fatigue, it would be possible to find the net effect of occupational balance damage. The use of a convenience sampling method and the self-reporting and online nature of the questionnaires were other limitations of the study.
5.1. Conclusions
The results of the present study indicated that occupational balance was lower in hospital-discharged COVID-19 survivors than in healthy people. Furthermore, they experienced higher anxiety, depression, and fatigue than healthy people after discharge. Therefore, people should receive appropriate training after discharge to create a balance between daily and favorite activities. Therapists can also design and implement new interventions to improve the occupational balance of COVID-19 survivors. Therefore, individuals' activity patterns and their favorite activities should be considered. This requires the serious attention of occupational therapists, managers, and health policy-makers.