1. Background
Low back pain (LBP) is one of the leading health problems known as the main cause of disability worldwide (1, 2). Low back pain could lead to functional disorders and occupational disabilities; therefore, apart from health-related problems, it could impose a considerable economic burden on both individuals and societies (3, 4). As a result, treating these patients or reducing the pain in patients who suffer from back pain is one of the major roles of the health system as it could either increase patients’ satisfaction or improve the productivity of society (5, 6). Several different therapeutic approaches, including medicines, chiropractic treatments, physiotherapy, and surgical modalities, have been previously introduced to cure and relieve LBP (7, 8). However, the mechanism of LBP is still unclear, and several contributing factors in the generation of LBP and the efficacy of treatments remain unknown.
Modic changes (MC) are a kind of change in the intensity of bone marrow signals and lesions of bone marrow seen within vertebral body endplates (9). The MC is routinely observed in magnetic resonance imaging (MRI) scans and has been suggested to be associated with LBP (9). The MC are more common in L4 - L5 and L5 - S1, and there is strong evidence regarding their association with age. They are also known as pain generators in the lumbar spine (10, 11). The effect of MC on different treatment modalities of LBP has been investigated in recent years. Numerous studies have investigated whether the presence or absence of MC could modify the outcome of different types of treatment.
According to a meta-analysis, MC does not affect the outcome of operative treatment in the cervical and lumbar spine (11). However, a study by Peterson et al. that investigated the effect of imaging-guided transforaminal-lumbar nerve root block showed that patients with MC had a lower tendency to improve, and this treatment provided worse outcomes in MC patients in comparison to those without MC (12). Conservative treatments are considered one of the most common therapeutic approaches in patients with LBP. However, there is a lack of data regarding the effect of MC on the efficacy of such treatments (13).
2. Objectives
The current study aimed to evaluate the efficacy of conservative treatments in patients with LBP in the presence and absence of MC. This study also investigated whether different types of MC could affect the effectiveness of conservative treatments in LBP patients.
3. Methods
This prospective cohort study was performed on 166 patients with LBP who were candidates for conservative treatments and were referred to an outpatient physiotherapy clinic in Tehran, Iran, in 2021. All patients were negative regarding disc herniation that was confirmed using an MRI scan within 3 months of symptoms presentation. Patients with serious underlying diseases, spinal cord infections and tumors, inflammatory spondyloarthropathies, trauma, acute fractures, severe osteoporosis, and Paget’s disease were excluded from the study. Moreover, patients with a history of spine surgery, focal neurological defects, pregnancy, and a body mass index higher than 30 kg/m2 were excluded.
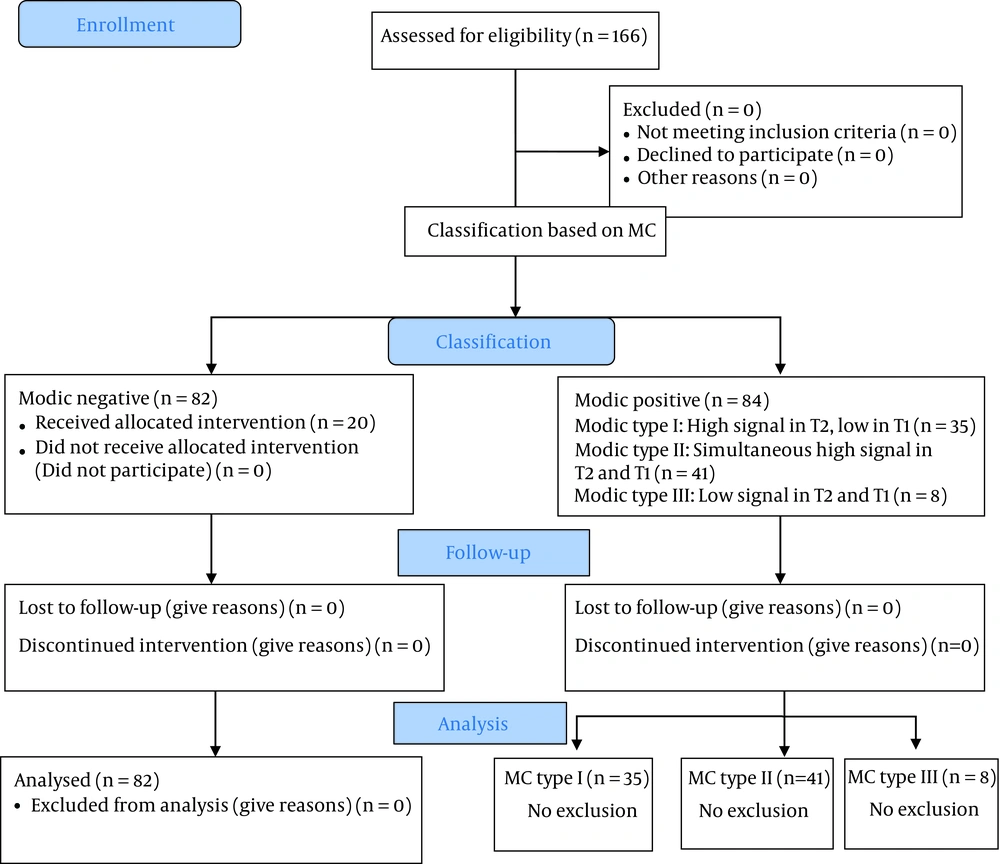
Before enrollment, the MRI scans were evaluated by a radiologist, and the patients were categorized into four groups regarding MC status. Then, the data on demographic variables were collected, and the Japanese Orthopedic Association (JOA) score was determined as a measure of back pain and disability using a valid and reliable questionnaire for each participant (14). Then, all study participants underwent 6-month conservative treatments in an outpatient physiotherapy clinic affiliated with Iranian Armed Forcec. The treatment procedure included heat therapy, ultrasound waves, transcutaneous electrical nerve stimulation (TENS), and special sports exercises (Williams and McKenzie). After 6 months, all the patients were visited by a neurosurgeon, and the JOA score was re-estimated for all of them. The primary outcome was the JOA change score calculated through posttreatment JOA score minus the baseline JOA score. The patients were defined as improved if the change score was higher than 0 (Figure 1).
3.1. Ethical Approval
The current study was reviewed and approved by the Review Board and Ethics Committee of AJA University of Medical Sciences (ethics code: IR.AJAUMS.REC.1400.323).
3.2. MRI Evaluation
The MRI scans were evaluated by a radiologist, and the patients were categorized into four groups. This phase aimed to determine the presence of MC. The MC cases were investigated in three groups, including type I, type II, and type III. The MC type I was defined as a high signal in T2 and low in T1 at or near the end of the vertebral body adjacent. According to the definition, the MC type II was addressed with simultaneous high signal in both T1 and T2, representing fat replacement in the hematopoietic part of the bone marrow. Finally, the MC type III was addressed as a low signal in T1 and T2 (sclerotic form) (15, 16).
3.3. Statistical Analysis
Baseline characteristics were described based on the presence and absence of MC. Mean, and standard deviation were reported for all continuous variables. The median was used to describe the data if the normality assumption was violated. The patients were also categorized based on the change in JOA score over the study period as improved and not-improved and provided frequency proportion and 95% confidence interval (CI). Baseline and posttreatment JOA scores were compared between the MC patients and no MC group using an independent t-test. One-way analysis of variance was also used to compare the mean scores of JOA for different types of MC. The non-parametric Kruskal-Wallis test was used to compare the median change scores of JOA between the compared groups. The proportion of improved cases between different groups was compared using the Chi-square test. The effects of MC positive and different types of MC adjusted for all potential confounders were also investigated using multiple linear regression. All statistical analyses were performed using Stata software (version 17.0; College Station, Texas, USA). P-values less than 0.05 were considered significant.
4. Results
The current study was performed on 166 patients with LBP who were referred to a physiotherapy clinic in Tehran, Iran, in 2021. Overall, 82 (49.4%) patients were negative regarding MC; however, 84 cases (50.6%) were MC-positive. The proportion of MC type I, type II, and type III was 21.1%, 24.7%, and 4.8%, respectively. Table 1 shows the baseline characteristics of patients with and without MC. The mean age values of MC-positive and -negative patients were 55.0 (13.0) and 52.4 (10.6) years, respectively (P = 0.160). The proportion of female gender was 43.9% and 51.2% in MC negative and positive groups, respectively (P = 0.347). The median duration of the pain in the MC negative and positive groups was 23.5 and 30.0 months, respectively (P = 0.291). The average JOA baseline scores were 14.4 (2.0) and 14.3 (2.3) in the MC negative and positive groups, respectively. No statistically significant difference was observed in this regard (P = 0.750) (Table 1).
| Characteristics | Modic-negative (n = 82) | Modic-positive (n = 84) | P-Value |
|---|---|---|---|
| Age | 52.4 ± 10.6 | 55.0 ± 13.0 | 0.160 |
| Female gender | 36 (43.9) | 43 (51.2) | 0.347 |
| Pain duration | 23.5 (12.0 - 50.0) | 30.0 (15.5 - 49.0) | 0.291 |
| Baseline JOA score | 14.4 ± 2.0 | 14.3 ± 2.3 | 0.750 |
Abbreviation: JOA, Japanese Orthopedic Association.
a Values are expressed as mean ± SD, No. (%) or median (Q1 - Q3).
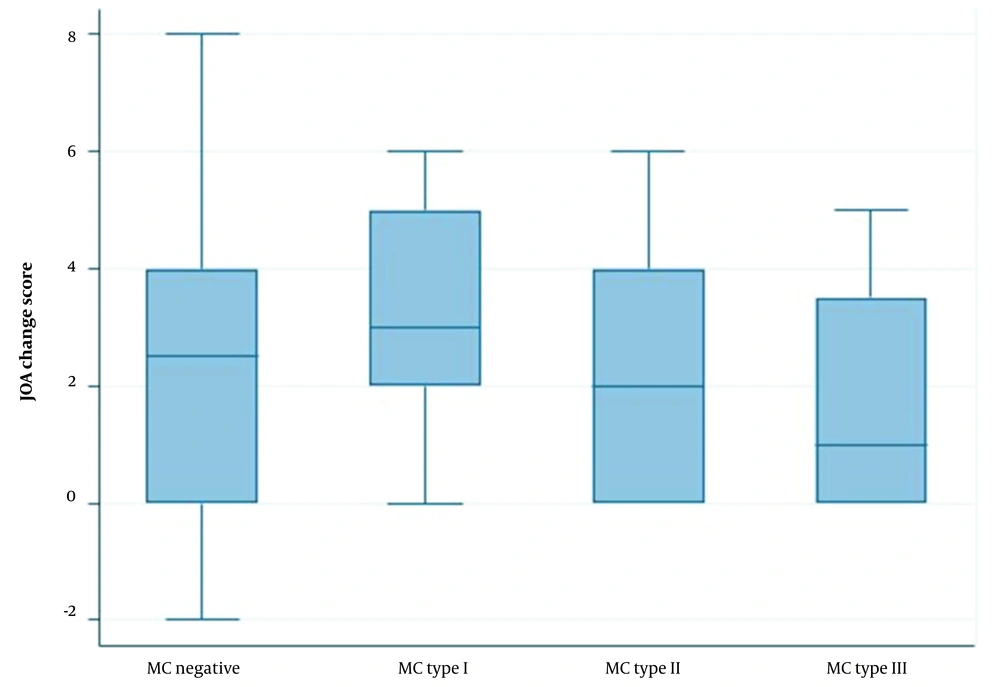
Posttreatment JOA scores in MC-negative and -positive patients were 17.1 (2.9) and 16.7 (3.4), respectively. However, no statistically significant difference was observed between the compared groups (0.540). The median change of JOA scores after 6-month conservative treatment was 2.5 and 2.0 in MC-negative and -positive patients (P = 0.630) (Table 2).
| Comparison | Posttreatment JOA | JOA Change | ||
|---|---|---|---|---|
| Mean ± SD | P-Value | Median (IQR) | P-Value | |
| Modic negative vs. positive | 0.540 | 0.630 | ||
| Modic negative (n = 82) | 17.1 ± 2.9 | 2.5 (4.0) | ||
| Modic positive (n = 84) | 16.7 ± 3.4 | 2.0 (3.0) | ||
| Different types of Modic changes | 0.059 | 0.104 | ||
| Modic type I (n = 35) | 17.8 ± 2.7 | 2.0 (3.0) | ||
| Modic type II (n = 41) | 15.9 ± 3.6 | 2.0 (4.0) | ||
| Modic type II (n = 8) | 16.3 ± 3.9 | 1.0 (3.5) | ||
Abbreviations: JOA, Japanese Orthopedic Association; SD, standard deviation; IQR, interquartile range.
Posttreatment JOA scores were also compared between different types of MC groups. According to Table 2, the average baseline JOA score for the MC type I group was 14.8 (2.0), which increased to 17.8 (2.7) after 6-month conservative treatment. The JOA score was 13.8 (2.4) in the MC type II group at the baseline, and after 6-month treatment, with 2.1 points average increase that reached 15.9 (3.6). Finally, in the MC type III group, the average baseline and posttreatment JOA scores were 14.6 (2.1) and 16.3 (3.9), respectively. No statistically significant difference was observed in the baseline JOA score, pos-treatment JOA score, and JOA change score (P > 0.05) (Table 2). Figure 2 depicts the median change score of JOA for each Modic type. According to Table 3, 70.7% of MC-negative patients had an improvement in JOA scores. The proportion of improvement was 82.8%, 63.4%, and 50.0% in MC type I, type II, and type III, respectively. However, the observed difference was not statistically significant (P = 0.561) (Table 3).
| Modic Status | n/N | Proportion (95% CI) | P-Value |
|---|---|---|---|
| Negative | 58/82 | 70.7 (59.9 - 79.6) | |
| Modic type I | 29/35 | 82.8 (54.3 - 84.0) | |
| Modic type II | 26/41 | 63.4 (47.7 - 76.7) | |
| Modic type III | 4/8 | 50.0 (19.7 - 80.2) | 0.561 |
Abbreviation: CI, confidence interval.
The multiple linear regression also showed that after adjustment for potential confounders, there was no significant difference in JOA posttreatment scores between MC-negative and MC-positive patients (regression coefficient = -0.2, 95% CI: -0.8 - 0.3; P = 0.428). Furthermore, there was no significant improvement in the MC type II (regression coefficient = 0.7, 95% CI: -0.1 - 1.5) and MC type III (regression coefficient = 1.2, 95% CI: -0.2 - 2.7), compared to the MC type I (P > 0.05) (Table 4).
| Comparison | Posttreatment JOA | |
|---|---|---|
| Regression Coefficient | P-Value | |
| Modic negative vs. positive | ||
| Modic negative | Reference | |
| Modic positive | -0.2 (-0.8 - 0.3) | 0.428 |
| Different types of Modic | ||
| Modic type I | Reference | |
| Modic type II | 0.7 (-0.1 - 1.5) | 0.124 |
| Modic type II | 1.2 (-0.2 - 2.7) | 0.117 |
Abbreviation: JOA, Japanese Orthopedic Association.
a The model was adjusted for age, gender, baseline JOA score, and pain duration.
5. Discussion
The current study was carried out to compare the outcome of 6-month conservative treatments, including heat therapy, ultrasound waves, TENS, and special sports exercises (Williams and McKenzie), in LBP patients with and without MC who were referred to an outpatient physiotherapy clinic in Tehran, Iran. This study also compared the effect of treatment on patients with different types of MC.
According to the obtained data, JOA average score was improved in both negative and positive MC patients. However, there was no statistically significant difference between the negative and positive MC groups regarding posttreatment JOA scores. In this study, there was also an upward trend in JOA scores in all types of MC over 6-month conservative treatments. There was no significant difference between different types of MC regarding postoperative JOA score and JOA change score. Overall, the percentage of patients with improvement in their clinical condition was 68.1%, with no significant difference between the compared groups (either negative and positive MC or different types of MC) in this regard.
There was a 68% improvement in the clinical condition of patients who received 6-month conservative treatments. These findings are comparable to the findings of a study by Annen et al., who observed that clinical conditions in 80% of patients with MC type I were improved over 3-month conservative treatments (17). This study showed that conservative treatment is a well-tolerated and effective therapeutic approach in LBP patients, patients with lumbar disc herniation with and without MC. In another study by Annen et al., the percentage of improved patients was only 52.2% which was considerably lower than the current study (13).
Along with all previous studies, conservative treatment was a safe and effective approach in patients with LBP regardless of their MC status leading to considerable improvement in the clinical condition of such patients (13, 17). Leemann et al. have shown that such treatments could provide significant improvement in the clinical condition of patients with LBP (18). Differences in the baseline characteristics of patients, such as age and chronicity of the pain, were the main reasons for these differences. Older ages and a higher proportion of chronic patients are related to less improvement. Moreover, longer follow-up was another reason to justify the observed difference in the improvement percentage.
In this study, there was no association between MC status and the percentage of patients with an improved clinical condition, and the presence of MC was irrelevant to pain improvement. Such findings are consistent with many previous studies. Ohtori et al. compared JOA scores between patients with and without MC and observed no statistically significant difference (19). Some other studies have also shown that MC had no clinical effect on treatment outcomes in patients with LBP (20-22). Moreover, in a meta-analysis by Lamberchts et al., it was concluded that MC could not be considered a predictive factor for postoperative pain or JOA score (11). Although most of these studies have evaluated more invasive treatment modalities, such as surgical procedures, their findings are consistent with the results of the present study. The study conducted by Annen et al. that evaluated the effect of conservative treatments has also shown similar results to the present study’s findings (13). The JOA change score after 6-month conservative chiropractic treatment was relatively higher, mainly due to older patients in MC groups. As it is already well-documented, older ages are associated with higher pain scores and disability.
The comparison of the baseline JOA score also showed no significant difference between MC and non-MC patients. There was also no significant association between different types of MC and baseline JOA scores. Such findings have been previously reported indicating that the presence of MC or a specific type of MC is not a potential risk factor for LBP and could not be considered a contraindication of conservative treatments (13). Previously repeated microtraumas leading to local inflammation and bacterial infection are two possible mechanisms already introduced in the etiology of MC type I (23-25). However, the results of previous studies in this regard are controversial.
5.1. Limitations
The current study was one of the rare attempts to investigate the efficacy of conservative treatments in patients with LBP with or without MC. However, some limitations should be regarded in interpreting the obtained findings. As the etiology of LBP remained unclear, several potential confounding factors have not been measured. This study also did not collect data on the chronicity of LBP, which could affect the obtained findings. The study sample size was also relatively small, particularly in some MC types, such as the MC type III, which could be considered another limitation of the current study that reduced the study power.
5.2. Conclusions
In conclusion, a 6-month conservative treatment was a safe and effective approach to improving the clinical condition of patients with LBP. However, there was no association between the presence of MC or any specific type of MC and treatment outcomes.