1. Introduction
Traumatic brain injury (TBI) is a major health problem, with 64 - 74 million cases yearly worldwide, resulting in morbidity and mortality (1, 2). Additionally, extensive studies of US military veterans have shown that prior TBI is associated with chronic multisystem conditions, suggesting repeated severe head injuries may be associated with long-term health and functional status (3, 4). Brain damage can cause some psychological
disorders in patients (5).
Changes in social behavior various studies have linked the extent of TBI injury to social behavior and emotion recognition or empathy. It is estimated that 39% of people with moderate to severe TBI have deficits in emotion recognition and impaired empathy. It has recently been proposed that a history of even minor brain injury may predispose certain individuals to develop this pathologic process, now referred to as "chronic traumatic encephalopathy" or CTE (6). The presentation of CTE is variable and may include neurologic and/or psychiatric manifestations. The current CTE literature suggests two common syndromes: A behavior and mood-predominant illness, frequently accompanied by paranoia, which would be diagnosed as a psychiatric illness, and a predominantly cognitive disorder frequently diagnosed as Alzheimer's disease (7). Anger and hostility are also related to depression and anxiety (8, 9). There are few studies about the effects of bioresonance on neuropsychological disorders in a patient with a head injury, so it is desirable to report this case. It is necessary to mention that bioresonance is a non-invasive method for early disease diagnosis based on the emission of very low-frequency electromagnetic waves to the patient's body and then receiving feedback to retrieve the information obtained (10).
2. Case Presentation
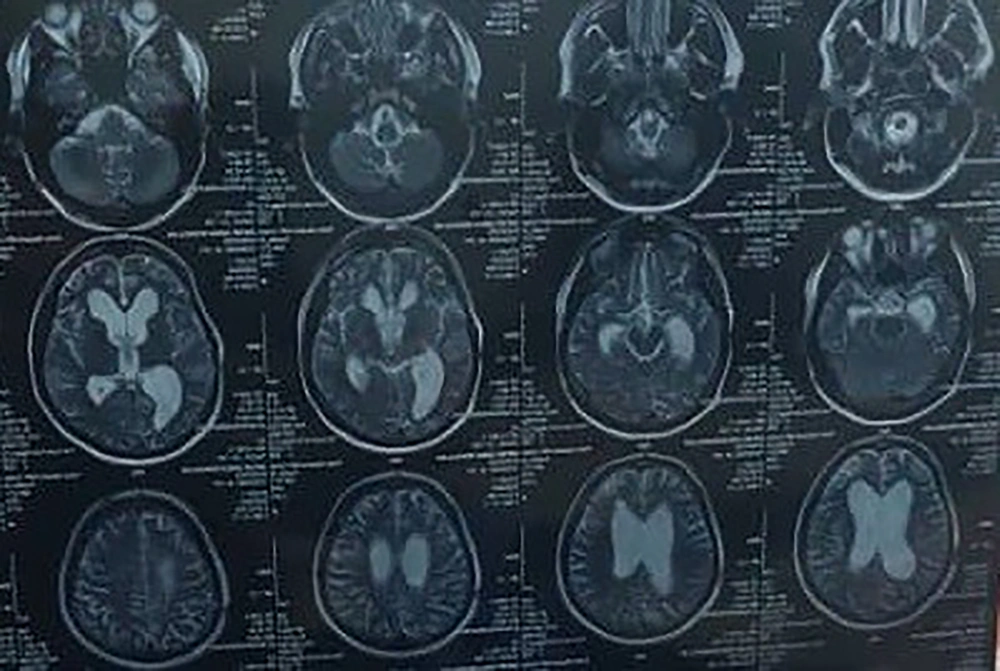
The patient is a 21-year-old man with behavioral and emotional changes since 5 years ago after multiple traumas. He spent 12 months semi-comatose before a surgeon put him in a ventricular shunt. He gradually regained consciousness but could not move. Also, during this period, the muscles of the upper and lower limbs contracted, and he could not walk. The patient also had difficulty not only speaking but also understanding speech. The worst complication that his family mentioned was emotional agitation and anger. He was visited by several doctors (neurologist, neurosurgeon), but his general condition did not change. During the last 5 years, he has taken drugs such as Depakine and Primidone. CT scan of the brain shows dilatation of the lateral ventricle (Figure 1).
In 2022, he was referred to the bioresonance center, where he was treated with bioresonance pharmaceutical complements. After 4 weeks of using the supplement, speech and understanding were measured by VAS, and the results showed improvement. It was noticeable that aggressive behavior gradually became normal behavior. The duration of treatment has been spent for 6 months.
3. Discussion
Brain damage can cause some mental disorders in patients. Magnetic therapy with very low-frequency electromagnetic frequency supplements is a non-invasive, safe, and simple method for healing injuries caused by various causes by different mechanisms like decreased edema and increased blood flow, and Aids in preventing post-ischemic lipid peroxidation (11). Some patients look for complementary methods instead of classical medicine for recovery. The bioresonance method is one of the complementary medicine methods that has received attention in recent years. Imanzade et al. studied that bioresonance can relieve phantom pain in patients with chronic and intractable pain (12). Also, in another study, bioresonance can reduce pain and increase muscle movements in a patient with avascular necrosis of the femur (13). There is no scientific evidence between bioresonance treatment and head trauma complications, so this study can guide other researchers to design more studies with high evidence to prove it. The authors express their gratitude to the patient for their cooperation and permission to publish the report.