1. Background
Cesarean section is the most common surgery among women worldwide (1). Different techniques are used to make a Cesarean incision, the most common of which is the Pfannenstiel incision (2). The incision is located at a breadth of 2 fingers above the pubic symphysis and is approximately 10 - 15 cm in length (1). In general, scalpels are used to make various skin incisions (3); they are made of tungsten carbide and are applied as disposables in different sizes, suitable for the type and size of surgical incisions (4). Some advantages of scalpels include simple use, high cutting precision, and minimal damage to adjacent tissues (5). However, the use of scalpels can be associated with problems such as damage to the personnel and surgical team during application and serious damage to the skin and tissues of patients in case of displacement (6). Research shows that most hospital damages are scalpel-related injuries among operating room personnel (5). Today, various methods, such as the Sharpless technique, have been proposed to prevent and reduce these risks (7), where the scalpel is replaced with methods such as electrosurgery, laser, and ultrasound to make an incision (8).
Electrosurgery is widely used to cut through tissues and control bleeding during surgical procedures. There are two types of electrosurgery, namely monopolar and bipolar. Monopolar electrosurgery is used to make surgical incisions via a pencil to apply electrical energy to the patient's body and a plate connected to the patient's body to discharge energy. Some of the advantages of electrosurgery include limited blood loss and the coagulation properties of electricity (9). Moreover, electrosurgery limits damage to the personnel and surgical team, which could occur due to the use of scalpels (3). However, a lack of adherence to safety points might lead to damages such as burns (9). The use of electrosurgery in operating rooms has made it possible for surgeons to control intraoperative bleeding and prevent unwanted scalpel complications. Studies have also shown its effect on reducing the duration of surgery and postoperative pain (10, 11).
Various studies have been conducted to compare the two methods in terms of the duration of surgery, postoperative pain, and the amount of bleeding (10-12). In surgery on candidates of Cesarean section, bleeding at the surgical site significantly decreased with the use of the electrosurgery technique (10). In another research, American researchers found no significant difference between the two methods regarding the amount of bleeding (11).
2. Objectives
The use of electrosurgery and scalpel in the operating room in pregnant women who are candidates for Cesarean section is controversial; moreover, studies in this field are limited, and the results are contradictory. Therefore, the researchers decided to compare the outcomes of using scalpel and electrosurgery methods for anterior abdominal wall incision during Cesarean section.
3. Methods
This double-blind clinical trial is the result of a master's thesis approved by the Research Committee of Mazandaran University of Medical Sciences (code of ethics: IR.MAZUMS.REC.1399.135) and registered in the Iranian Registry of Clinical Trials (IRCT20200501047254N1).
The primary variables of the study included incision time, duration of surgery, hemodynamic status, intraoperative bleeding rate, injury to the surgical team, and the infant's Apgar score. The secondary variables were the time of spinal anesthesia wear off, postoperative pain, amount of pain medication received such as pethidine and diclofenac suppositories, and wound complications.
These variables were compared in scalpel and electrosurgery groups in Allameh Bohlool Gonabadi Hospital (Iran) in 2020. The research population included pregnant women who were candidates for a Cesarean section with spinal anesthesia. The inclusion criteria were an age range of 18 - 45 years, gestational age of 37 - 41 weeks, Pfannenstiel skin incision, and willingness to participate. The exclusion criteria were emergency Cesarean section, vertical skin incisions, incomplete medical files, chronic skin diseases (e.g., psoriasis and eczema), allergy to antibiotics, consuming anticoagulants, cardiovascular and pulmonary problems, and underlying diseases (e.g., diabetes, hypertension, liver disease, chronic anemia, kidney failure, and immunodeficiency). A total of 86 patients were included. First, all the patients were subjected to spinal anesthesia by an anesthesiologist and with the same drug. Then, the patients were randomized into two groups. In the electrosurgery group, 43 patients had electrosurgical skin incisions in which the superficial skin layer was opened with a scalpel, and the other layers were cut using the monopolar electrosurgery cutting mode with 120 W of sinusoidal power. For the 43 patients in the scalpel group, an incision was made from the skin to the uterus using scalpel blade No. 22.
The demographic information, including age, weight, height, body mass index (BMI), and gestational age, were extracted from the patients' files and recorded in a checklist designed by the researchers.
Surgical incision time was measured using a timer from the moment to the end of the surgical incision. A timer was also used to measure the length of surgery from the moment of starting the surgery to the wound dressing. The patients' hemodynamic status, including systolic and diastolic pressures and heart rate, were measured and recorded before the incision using anesthesia monitoring. The mentioned variables were also measured and recorded when making the incisions. The weighed blood gases and the volume of blood absorbed by the gases were added to the volume of blood in the suction to measure the amount of bleeding. The Apgar score of the newborns was measured and recorded in minutes 1 and 5 after birth. In case of injury to the surgical team or the patients during the surgical incision, the researchers who supervised the use of scalpel and electrosurgery during the surgery noticed and recorded that in the checklist.
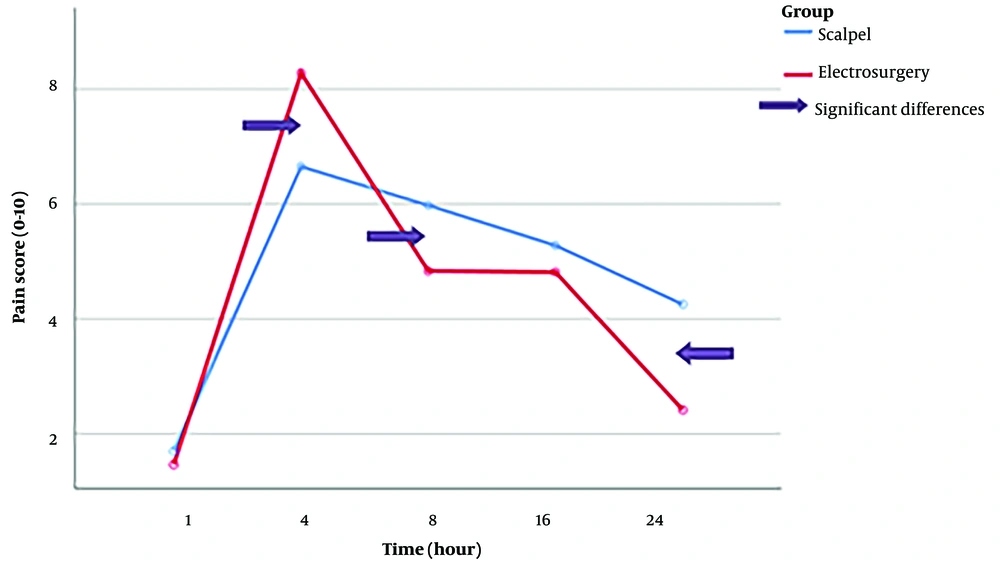
The time of the return of pain and the number of receiving analgesics, including diclofenac suppository and pethidine ampoules, as well as the patient's pain intensity according to the NRS (Numeric Rating Scale) criteria at 1, 4, 8, 16, and 24 hours after surgery were recorded to measure postoperative pain. The condition of the surgical wound was evaluated for wound length, wound infection, secretion rate, skin temperature at the operation site, spread of pain around the wound, and wound complications up to 24 hours after the surgery.
3.1. Statistical Analysis
Data analysis was performed in SPSS v. 22 (IBM Corp., Armonk, NY, USA) using the Kolmogorov-Smirnov test and Shapiro-Wilk test (to assess the normality of data distribution), t-test, Mann-Whitney U test (in case of abnormal data distribution), and chi-square and Fisher's exact test.
4. Results
The results related to the demographic information of the two groups showed that there was no significant difference between them in terms of demographic characteristics, including weight, height, BMI, age, gestational age, history of Cesarean section, and intra-abdominal adhesions (P > 0.05; Table 1).
| Scalpel | Electrosurgery | P-Value | |
|---|---|---|---|
| Age, y | 30.56 ± 5.68 | 32.42 ± 5.43 | 0.125 |
| Weight, kg | 74.40 ± 11.99 | 79.67 ± 13.37 | 0.057 |
| Height, cm | 159.30 ± 5.37 | 161.02 ± 6.62 | 0.189 |
| Body Mass Index, kg.m2 | 29.27 ± 4.25 | 30.79 ± 5.32 | 0.149 |
| Gestational age, w | 38.37 ± 0.69 | 38.40 ± 0.72 | 0.880 |
a Values are expressed as mean ± SD.
The mean of surgical incision time was less in the scalpel group (97.58 s) than in the electrosurgery group (113.07s), and the difference was significant (P-value = 0.012). Moreover, the mean duration of surgery significantly differed (P-value = 0.012; Table 2).
| Scalpel | Electrosurgery | P-Value | |
|---|---|---|---|
| Incision time, s | 97.58 ± 39.20 | 113.07 ± 41.28 | 0.049 |
| duration of surgery, min | 45.49 ± 17.90 | 37.12 ± 12.39 | 0.012 |
| Intraoperative bleeding, cc | 470.91 ± 172.77 | 513.69 ± 180.83 | 0.181 |
| Preoperative systolic blood pressure, BP, mmHg | 129.33 ± 13.13 | 133.74 ± 13.61 | 0.129 |
| Preoperative diastolic BP, mmHg | 81.51 ± 15.01 | 81.49 ± 13.57 | 0.994 |
| Intraoperative systolic BP, mmHg | 121.28 ± 14.43 | 101.67 ± 18.01 | <0.001 |
| Intraoperative diastolic BP, mmHg | 71.56 ± 15.24 | 59.84 ± 16.09 | 0.001 |
| Systolic BP changes, mmHg | -8.04 ± 14.70 | - 32.06 ± 18.56 | <0.001 |
| Diastolic BP changes, mmHg | -9.95 ± 21.13 | -21.65 ± 15.33 | 0.004 |
| Preoperative HR, min | 103.26 ± 14.76 | 99.44 ± 16.19 | 0.257 |
| Intraoperative HR, min | 99.70 ± 23.71 | 91.33 ± 26.04 | 0.123 |
| HR changes, min | -3.55 ± 21.10 | -8.11 ± 25.94 | 0.374 |
| Diclofenac consumption | 1.63 ± 1.11 | 1.23 ± 0.68 | 0.047 |
| Pethidine consumption | 1.00 ± 0.72 | 0.65 ± 0.61 | 0.023 |
| Surgical wound length, cm | 13.23 ± 1.58 | 13.79 ± 1.45 | 0.159 |
a Values are expressed as mean ± SD.
The results of the analysis of the hemodynamic status in the three sections of systolic and diastolic pressure and heart rate showed no significant difference between the two groups in terms of systolic blood pressure before the surgery, but this difference was significant during the surgery (P = 0.000). Thus, in the electrosurgery group, the mean systolic blood pressure during the surgery was lower than in the scalpel group. Changes in systolic blood pressure before and during the surgery were also significant (P = 0.000; Table 2).
The mean preoperative systolic blood pressure in the scalpel and electrosurgery groups was 129.33 and 133.74 mmHg, respectively, and the mean intraoperative blood pressure in the scalpel and electrosurgery groups was 121.28 and 101.67 mmHg, respectively, showing a reduction in this variable in the groups during surgical incision. Changes in this variable were reported to be 8.0465 mmHg in the scalpel group and 32.098 mmHg in the electrosurgery group.
In terms of preoperative diastolic blood pressure, the results were indicative of no significant difference between the two groups (P = 0.994). However, a significant difference was observed between the two groups during incision; in this regard, the intraoperative diastolic blood pressure of the participants in the scalpel and electrosurgery groups was reported to be 71.56 mmHg and 50.84 mmHg, respectively (P = 0.01). In addition, we detected a significant difference between the two groups regarding changes in the preoperative and intraoperative diastolic blood pressure (P = 0.004). Accordingly, the mean changes in the diastolic blood pressure were lower in the electrosurgery group (21.6512 mmHg) compared to the scalpel group (0.0535 mmHg). The results also showed that the electrosurgery method caused a greater decline in diastolic blood pressure compared to the scalpel group (Table 2).
No significant difference was detected between the groups in terms of heart rate before and during the surgery and changes in the heart rate before and during the surgery (P < 0.05).
In addition, no significant difference was observed between the groups regarding intraoperative bleeding (P = 0.181). In this regard, the mean amount of bleeding in the scalpel and electrosurgery groups was estimated at 470.9±172.7 mL and 513.6±180.83 mL, respectively (P = 0.181).
The Apgar score of the newborns was not significantly different from each other. Skin damage was not observed in any of the surgical team members and patients after using the two-incision methods.
The two groups showed a significant difference in terms of the time of disappearance of spinal anesthesia and the return of pain; in 58.1% of pregnant women in the scalpel group, the effect of spinal anesthesia disappeared in less than 2 hours after the surgery, but only 34.9% of the electrosurgery group returned to normal after the surgery at this time (P = 0.019). In addition, the amount of diclofenac suppository (P = 0.047) and pethidine ampoule use (P = 0.023) in the scalpel group was significantly higher than in the electrosurgery group. After measuring the pain intensity of the patients using the pain NRS, the results showed no significant difference in pain 1 hour after the surgery (P = 0.317); nevertheless, there was a significant difference 4 hours after the surgery, and less pain was observed in the scalpel group (P = 0.012). There was a significant difference 8 (P = 0.014) and 24 (P = 0.001) hours after the surgery, and less pain was observed in the electrosurgery group. Sixteen hours after the surgery, no significant difference was shown between the two groups (P > 0.05; Figure 1).
The two groups were also compared in terms of the time of disappearance of spinal anesthesia, and a significant difference was observed (Table 3).
| Scalpel | Electrosurgery | P-Value | |
|---|---|---|---|
| Less than 2 hours | 25 (58.1) | 15 (34.9) | 0.019 |
| Between 2 and 3 hours | 15 (34.9) | 16 (37.2) | |
| More than 3 hours | 3 (7) | 12 (27.9) |
a Values are expressed as No. (%).
In both groups, there were no complications related to the surgical wound, and all the subjects were completely normal in terms of skin color, wound secretions, infection, or increased temperature of the wound 24 hours after the operation.
Besides, none of the participants and surgical team members were injured by electrosurgery or scalpel during the study.
5. Discussion
In the present study, 86 eligible patients who were candidates for elective Cesarean section by spinal anesthesia were randomly divided into two groups. Then, an incision was made in the anterior abdominal wall using a scalpel in one group, and electrosurgery was used in the other group.
An objective of the present study was to determine the incision time. The results indicated that there was a significant difference between the two groups in terms of incision time, indicating an increase in incision time in the electrosurgery group. In a study by AbdElaal et al., the surgical incision time was shorter in the electrosurgery group than in the scalpel group, contrary to our results (12). In addition, in the study of Caliendo et al., the incision time in the electrosurgery group was significantly shorter than in the scalpel group (11). This difference in the results may be due to differences in the surgical team's skill and speed of surgery in the use of electrosurgery in the two studies.
The next variable was the duration of surgery. The results indicated that the duration of surgery in the electrosurgery group was shorter than in the scalpel group (P < 0.05). This result was consistent with the results of the study by AbdElaal et al. (12) and Gupta et al., (13) which indicates the positive effect of electrosurgery on reducing surgery time. However, it was not in line with the results of the study by Isci Bostanci et al. (14). This inconsistency may be due to differences in the condition of the studied patients or the surgical team's speed of surgery. Despite the prolongation of incision time in the electrosurgery method, the duration of surgery in this group was shorter than in the scalpel group. Controlling the bleeding during surgical incision using electrosurgery may prolong the time required for the incision, but it prevents the prolongation of surgery by keeping the operation site clean. In this study, in the method of using a scalpel, due to bleeding from small bleeding vessels in the incision area, the operation site was not completely bloodless, and this issue had a negative effect on the speed of the surgery in this group.
According to the assessments, no significant difference was observed between the two groups in terms of preoperative systolic blood pressure. However, the variable was significantly different in the two groups during the incision. Moreover, a comparison of the two groups in terms of changes in systolic blood pressure demonstrated a significant difference. Diastolic blood pressure significantly decreased in the electrosurgery group. Meanwhile, no significant difference was observed between the two groups in terms of heart rate. Notably, the hemodynamic status of the subjects has not been reported in similar studies, although a sustainable hemodynamic status is an important point during and after the surgery, and attempts must be made by the surgical team to maintain it at a stable level (11, 12, 14). According to the results of the present study, making surgical incisions with an electrosurgery device led to a severe drop in the participants' blood pressure. Therefore, blood pressure drop and related complications should be anticipated in surgery with electrosurgery.
Another goal was to compare the amount of bleeding in the two groups, which did not show a significant difference. Various studies have compared the volume of blood loss due to electrical and scalpel surgery. In a study by Elbohoty et al., the average blood loss was 20 g in the scalpel group and 11 g in the electrosurgery group, which was significantly lower in the electrosurgery group (10). In addition, AbdElaal et al. reported significantly less bleeding in the electrical surgery group compared to the scalpel group (12). Similar results were reported by Caliendo et al. (11). Therefore, the lack of a significant difference in the present study may be due to the measurement of the volume of blood loss during surgery, whereas these studies only measured bleeding at the time of the surgical incision. In addition, the Apgar score of the newborns in this study did not show a significant difference in the two groups, consistent with the findings of Isci Bostanci et al. (14). In our study, besides the infant's health, we also considered the health of the surgical team, which had not been investigated in other studies.
Examining the postoperative pain status showed that pain after surgical incision using electrosurgery is significantly less than after using a scalpel. Similarly, in the study by Elbohoty et al., the amount of analgesic received by the electrosurgery group was significantly lower than the scalpel group. However, their study measured postoperative pain only by measuring the number of analgesics received by the patients (10). In another study conducted by American researchers, pain was measured using the visual analog scale (VAS) in the first and second days after the surgery, and no significant difference was observed. Besides the pain measurement criteria, another difference between this and our study is the frequency and timing of pain measurement. In this study, pain was measured for the first time after 24 hours post-surgery, while pain begins immediately after the disappearance of the effect of spinal anesthesia. Furthermore, other pain-related factors that were measured in our study and could provide a better view of pain were not measured by them (11). In Spain, researchers evaluated patients' pain 24 and 48 hours after surgery based on VAS and concluded that there was no significant difference in pain between the two groups. This difference may be due to the difference in the tolerance threshold of the studied patients or in the use of postoperative painkillers because the amount of postoperative painkillers was not reported in the mentioned study (15). In another study, pain was measured using VAS 4, 8, 16, and 24 hours after the operation, and in line with our study, they reported a significant difference between the two groups. In this study, the amount of analgesic drug use (diclofenac suppository) was measured by the researchers; like our study, the rate of drug administration in the scalpel group was significantly higher than in the electrosurgery group (12). In our study, in addition to measuring pain 24 hours after the surgery and measuring the amount of analgesic drug received by the patients, the time of disappearance of spinal anesthesia was also measured, which was not considered in the mentioned study. The use of electricity to make a cut may reduce the sensitivity and transmission of nerve messages by affecting the pain receptors in the skin of the area. Therefore, the need for painkillers also decreases.
The other objective of this study was to examine wound complications following surgery; 24 hours after the Cesarean section, factors including wound length, wound skin color, wound discharge, wound infection, and increase in skin temperature at the wound site were measured. Based on the data obtained, the factors related to surgical wounds were normal in all the subjects, and no complications were observed that indicated infection at the surgical site. No significant difference was seen in any of the studies conducted by other researchers (10, 11, 14, 15). This finding confirms that the use of electrosurgery to make a surgical incision has no effect on wound healing and its related factors. However, the complications of the wound may vary according to the method of care and compliance with health tips.
5.1. Conclusions
Many gynecologists and obstetricians currently avoid electrosurgery for Caesarean section due to the fear of causing burns following its use and bitter experiences in this regard; still, the results of this study revealed that the use of electrosurgery correctly and in compliance with safety precautions causes no problem when making an incision in the anterior wall of the abdomen during Cesarean section; it even shortens the duration of surgery, which, in turn, reduces postoperative complications. It also has a positive effect on reducing postoperative pain. In terms of hospital costs, there is no difference between this and the scalpel technique, and it does not impose additional costs on the patient. However, due to the significant reduction in blood pressure when using the electrosurgery device, it is recommended that the intraoperative hemodynamic status of patients be monitored by the surgical team so that effective measures can be taken if their blood pressure decreases.