1. Background
In December 2019, the emergence of a new pneumonia in Wuhan, China, entered a new phase of a dangerous epidemic and became a global health emergency in the world. This viral disease, called COVID-19, has a latent period of 1 to 14 days, with fever, dry cough, and severe fatigue being the most important complications (1). Over the past two years, COVID-19 has become a dangerous pandemic and one of the major health problems worldwide. Due to the lack of definitive treatment for this disease, all governments have tried to control the spread of the virus through restrictions and quarantines, which have led to changes in the lifestyles of different populations (2). Lifestyle changes lead to changes in social relationships, loss of opportunities, and reduced relationships while reducing mobility and physical activity levels (3). Previous findings about pandemics, such as those caused by Severe Acute Respiratory Syndrome (SARS), show that the social consequences of such pandemics include anxiety, stress, and mental disorders (4). Undoubtedly, all these consequences can affect people's sleep quality.
The results of some studies show that sleep problems are more common in the young population than in other groups (5). Various aspects of life, such as consciousness, memory, cognitive function, body energy level, and physical function, are affected by insufficient sleep (6). Stress is an integral part of human life in an epidemic, which has a negative relationship with sleep quality. Under stress, the quality and duration of sleep are significantly affected (7). A study conducted by Casagrande et al. (2020) on Italians found that 57.1% of the participants had poor sleep quality during the COVID-19 period (2). In Spain, the sleep quality of homeless people improved during the quarantine period of COVID-19 (8).
Exercise and physical activity have been shown to improve the quality of life, and no doubt sleep quality can be widely affected by this factor (9). Many studies have been done on sleep and life qualities in different groups of society, so many studies reported that exercise can have a positive effect on sleep quality (10-12). In COVID-19, all the people who had recreational or professional physical activity suffered much physical and mental damage due to the restrictions. In England and the region of Scotland, many people aged 18 to 72 years had the lowest amount of physical activity, while there was a positive relationship between sleep quality and the level of physical activity in these people (13). Therefore, the question arises as to whether the sleep quality of athletes from recreational to professional levels has changed during this period (14-16).
It seems that exercise and physical activity can improve the sleep quality of people (12, 17, 18). Sadeghipour et al. reported that the quality of life in physically active students and men was higher (19). Mon-Lopez reported that the training volume for Spanish handball players has significantly decreased during COVID-19, as has the sleep of male players. However, the sleep quality of professional male players has also significantly decreased (8). Zar et al. reported that active soldiers had better sleep quality than soldiers who had lower levels of physical activity (20). However, it can be said that the quality of sleep is particularly important for certain groups of people, such as students, because it has a significant impact on their academic performance. Research shows that during the COVID-19 epidemic, the anxiety caused by this disease greatly affects the quality of students' sleep (21). Therefore, it is crucial to focus on other factors that can minimize the negative impact of such epidemics on students' sleep quality. One such factor is exercise and physical activity.
2. Objectives
Limiting factors such as quarantine in pandemics such as COVID-19 reduce a person's physical activity, which may also affect sleep quality. The current study aimed to compare the sleep quality in active and inactive students during the COVID-19 pandemic in Iran.
3. Methods
3.1. Participants
In this cross-sectional study with a post-event design, a total of 326 students from Persian Gulf University (182 females: 80 physically active and 102 inactive, and 144 males: 68 physically active and 76 inactive) volunteered to participate. The data required for this research was collected electronically via the student's academic emails in 2020. Individuals with at least 3 sessions of exercise per week (45 minutes per session) were defined as a "physically active" group, and those who did not engage in any physical activity during the week (other than daily activities) were included in the inactive group (Based on the self-declaration of the participants at the beginning of the research) (20, 22). Participation in the study was voluntary, and all subjects completed an informed consent form. First, the demographic characteristics of the participants, such as age, height, and weight, were recorded. Data were then collected using questionnaires: The Petersburg Sleep Questionnaire and the Demographic Characteristics Questionnaire.
In the current research, ethical principles were followed, informed consent was obtained from all participants, and they were assured of the confidentiality of the research information. This research was approved by the Research Ethics Committee of Jahrom University of Medical Sciences, Jahrom, Iran (ethics code: IR.JUMS.REC.1399.044).
3.2. Petersburg Sleep Questionnaire
The Petersburg Sleep Questionnaire was used to measure sleep quality, which included 9 questions, categorized into 7 clinically derived components of mental quality of sleep, delayed sleep, duration of sleep, efficiency and effectiveness of sleep, sleep disturbance, amount of sleeping pills, and dysfunction (23). All the above components were calculated in the morning and based on the results of the questionnaire. Each question was scored on a Likert scale between 0 and 3, and a score of 3 on each scale is known as the maximum negative. The overall score of this questionnaire is between 0 and 21, and the higher the score, the lower the sleep quality of the respondent. A score above 5 indicates poor sleep quality. The reliability and validity of the questionnaire have been confirmed in previous reports, with a reliability of 0.83 and a validity between 86.5 and 89.6 (24).
3.3. Statistical Analysis
Descriptive statistics (mean and standard deviation) were used. The Kolmogorov-Smirnov test assessed the normality of the data distribution, and the independent t-test evaluated them. Also, statistical analyses were performed using IBM SPSS 18.0 software (Armonk, NY: IBM Corp.), and α = 0.05 was considered the significance level.
4. Results
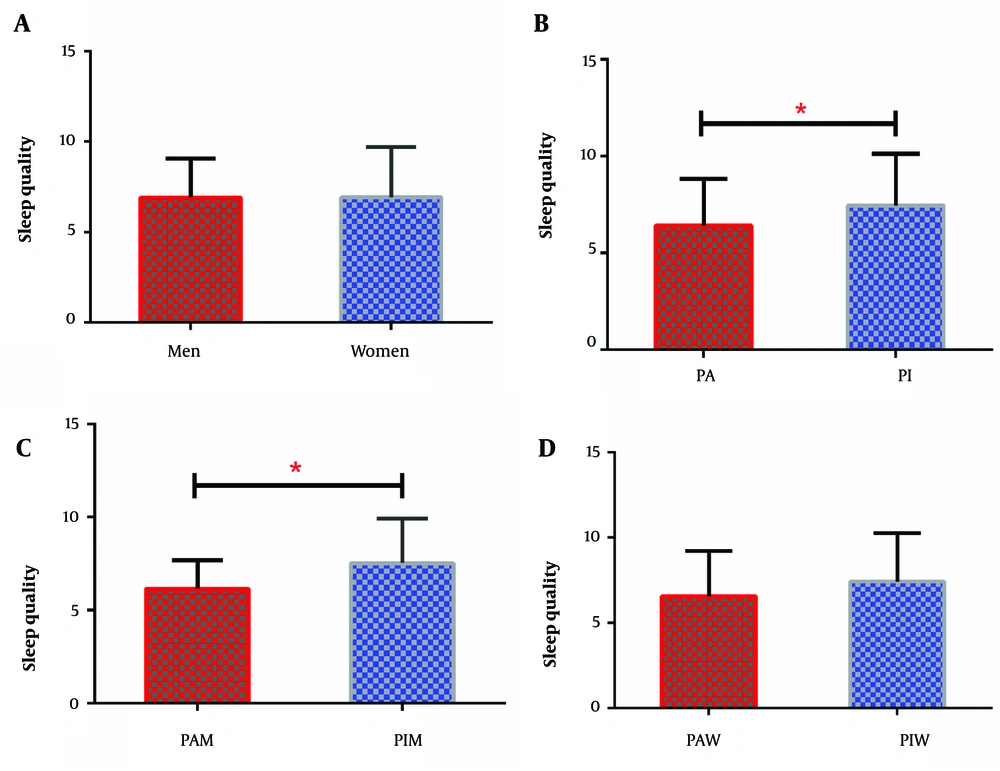
The results showed that male students scored lower than female students on the subscales of sleep latency (P = 0.320), habitual sleep efficiency (P = 0.936), the use of sleeping medication (P = 0.101), and daytime dysfunction (P = 0.217) and as a result, they were in a better situation. On the other hand, female students scored lower than male students on the subscales of subjective sleep quality (P = 0.430), sleep disturbances (P = 0.636), and sleep duration (P = 0.002), and as a result, they were in a better condition. In general, we found no significant difference in the overall sleep quality between male and female students (P = 0.953) (Table 1, Figure 1A).
| Variables | Males | Females | P-Value |
|---|---|---|---|
| Subjective sleep quality | 1.22 ± 0.68 | 1.14 ± 0.74 | 0.430 |
| Sleep latency | 1.14 ± 1.05 | 1.30 ± 1.19 | 0.320 |
| Sleep duration | 0.75 ± 0.74 | 1.05 ± 0.67 | 0.002 b |
| Habitual sleep efficiency | 1.02 ± 0.79 | 1.03± 0.91 | 0.936 |
| Sleep disturbances | 0.88 ± 0.58 | 0.84 ± 0.59 | 0.636 |
| Use of sleeping medication | 0.67 ± 0.59 | 0.82 ± 0.69 | 0.101 |
| Daytime dysfunction | 0.90 ± 0.71 | 1.04 ± 0.85 | 0.217 |
| Overall sleep quality | 6.90 ± 2.14 | 6.92 ± 2.74 | 0.953 |
Comparisons of Sleep Quality and its Subscales in Subjects a
Comparisons of sleep quality in different research groups. A, Between male and female subjects; B, Between active and inactive subjects; C, Between active male and inactive male subjects; D, Between active and inactive female subjects. Data are shown as the mean ± standard error of the mean. * P ≤0.05 considered significant. PA, physically active; PI, physically inactive; PAW, physically active female; PIW, physically inactive female; PAM, physically active men; PIM, physically inactive men
Physically active students scored lower than physically inactive students on different subscales of sleep quality. However, only sleep quality (P = 0.003), sleep disturbances (P = 0.015), and daytime dysfunction (P = 0.005) were significantly lower in physically active students. In general, physically active students had better overall sleep quality than physically inactive students (P = 0.003) (Table 2, Figure 1B).
| Variables | Group | P-Value | |
|---|---|---|---|
| Physically Active | Physically Inactive | ||
| Subjective sleep quality | 1.03 ± 0.72 | 1.32 ± 0.69 | 0.003 b |
| Sleep latency | 1.25 ± 1.07 | 1.23 ± 1.22 | 0.916 |
| Sleep duration | 0.83 ± 0.73 | 0.87 ± 0.75 | 0.711 |
| Habitual sleep efficiency | 0.95 ± 0.89 | 1.11 ± 0.84 | 0.171 |
| Sleep disturbances | 0.76 ± 0.55 | 0.96 ± 0.61 | 0.015 b |
| Use of sleeping medication | 0.74 ± 0.67 | 0.79 ± 0.65 | 0.609 |
| Daytime dysfunction | 0.85 ± 0.80 | 1.15 ± 0.78 | 0.005 b |
| Overall sleep quality | 6.43 ± 2.36 | 7.46 ± 2.64 | 0.003 b |
Comparisons of Sleep Quality and its Subscales in Active and Inactive Groups a
On the subscales of subjective sleep quality (P = 0.601), sleep latency (P = 0.279), sleep duration (P = 0.785), habitual sleep efficiency (P = 0.405), and daytime dysfunction (P = 0.358), physically active male students obtained better scores than physically inactive male students. The subscales of sleep disturbances (P = 0.005) and the use of sleeping medication (P = 0.021) were significantly lower in physically active students, so physically active male students were in a better condition. In general, it was found that physically active male students had lower scores and better status in the overall sleep quality than physically inactive male students, as there was a significant difference in the overall sleep quality between physically active male students and physically inactive male students (P = 0.003) (Table 3, Figure 1C).
| Variables | Male Group | P-Value | |
|---|---|---|---|
| Physically Active | Physically Inactive | ||
| Subjective sleep quality | 1.17 ± 0.75 | 1.26 ± 0.62 | 0.601 |
| Sleep latency | 1.00 ± 0.98 | 1.26 ± 1.10 | 0.279 |
| Sleep duration | 1.02 ± 0.62 | 1.07 ± 0.71 | 0.785 |
| Habitual sleep efficiency | 0.94 ± 0.77 | 1.09 ± 0.82 | 0.405 |
| Sleep disturbances | 0.67 ± 0.53 | 1.04 ± 0.58 | 0.005 b |
| Use of sleeping medication | 0.50 ± 0.50 | 0.80 ± 0.63 | 0.021 b |
| Daytime dysfunction | 0.82 ± 0.71 | 0.97 ± 0.71 | 0.358 |
| Overall sleep quality | 6.14 ± 1.54 | 7.52 ± 2.38 | 0.003 b |
Comparisons of Sleep Quality and its Subscales in Physically Active and Physically Inactive Male Students a
On the subscales of sleep latency (P = 0.502), sleep duration (P = 0.872), habitual sleep efficiency (P = 0.263), sleep disturbances (P = 0.345), and the use of sleeping medication (P = 0.553), physically active male students obtained better score than physically inactive male students. The subscales of subjective sleep quality (P = 0.002) and daytime dysfunction (P = 0.003) were significantly lower in physically active students than in physically inactive female students. It was found that physically active female students had lower scores and better status in overall sleep quality than physically inactive female students. However, there is no significant difference in the overall sleep quality between physically active female students and physically inactive female students (P = 0.071) (Table 4, Figure 1B).
| Variables | Female Group | P-Value | |
|---|---|---|---|
| Physically Active | Physically Inactive | ||
| Subjective sleep quality | 0.97 ± 0.71 | 1.37 ± 0.74 | 0.002 b |
| Sleep latency | 1.36 ± 1.10 | 1.22 ± 1.31 | 0.502 |
| Sleep duration | 0.75 ± 0.77 | 0.72 ± 0.76 | 0.872 |
| Habitual sleep efficiency | 0.96 ± 0.94 | 1.13 ± 0.86 | 0.263 |
| Sleep disturbances | 0.80 ± 0.56 | 0.89 ± 0.63 | 0.345 |
| Use of sleeping medication | 0.85 ± 0.71 | 0.77 ± 0.67 | 0.553 |
| Daytime dysfunction | 0.86 ± 0.83 | 1.28 ± 0.81 | 0.003 b |
| Overall sleep quality | 6.56 ± 2.63 | 7.42 ± 2.83 | 0.071 |
Comparisons of Sleep Quality and its Subscales in Physically Active and Physically Inactive Female Students a
5. Discussion
In the present study, we showed that during the COVID-19 quarantine period, physically active students generally had better sleep quality. Researchers did not find a similar study comparing athletes' and non-athletes' sleep quality in COVID-19 restriction time. However, in the study by Liu et al., patients with COVID-19 were divided into two groups, and the group that used progressive muscle relaxation technology had better sleep quality and less anxiety. They believed that the reason for this effect on sleep quality and anxiety in the subjects is the creation of a balance in the anterior hypothalamic nucleus due to muscle activity (1). Ferendiuk et al. also stated that by reducing the activity of the sympathetic nervous system, the side effects of stress and anxiety are reduced. Thus, mental and physical relaxation is created (25). Zar et al. also emphasized the importance of physical activity in improving psychological aspects. They showed that active soldiers had better sleep quality than inactive soldiers (20). However, the findings show that during the quarantine period of the epidemic, psychological symptoms (stress, anxiety, depression) increase over time (26), which can affect sleep quality. Mon-Lopez et al. stated that during the COVID-19 quarantine, mental health is severely affected by reduced levels of physical activity, negatively affecting sleep quality due to lifestyle changes (8).
In the present study, both groups of male and female athletes had better scores than non-athletes on the sleep disorder subscale. In a study by Duong, both groups of male and female students had fear and anxiety of getting infected with COVID-19 and, as a result, high sleep disorder (27). Accordingly, it can be said that athletes have a higher mood in the face of conditions similar to COVID-19 and have a higher sleep quality. In a study by Facer-Childs et al., athletes reported longer sleep time and more sleep delay than non-athletes. The researchers found that athletes slept longer than before the pandemic. Also, excessive screening was a primary factor in delaying athletes' sleep (28). In our study, screening may be one of the reasons for the significant difference in sleep delay between athlete and non-athlete students. However, according to the study conducted by Washif et al., the quantity and quality of sleep among athletes did not significantly change during the quarantine period in the training camp despite the COVID-19 restrictions (29). This suggests that exercise, even in a quarantine training environment, can have a positive impact on athletes' mental well-being without compromising their sleep quality.
However, there is a hypothesis that disease quarantine can be associated with negative psychological effects due to reduced levels of physical activity, especially in athletes. However, two separate studies in Italy (30) and Spain (8) reported that levels of physical activity increased during home quarantine and had positive effects on mental health. In contrast, Ingram et al. stated that any restriction on physical activity can negatively affect sleep quality. In their study, they found that the COVID-19 quarantine was associated with decreased levels of physical activity, which reduced the quality of sleep (13). It appears that the disparity in culture, education, welfare, and economic stability among different countries could potentially be factors contributing to this variation.
In the present study, although the level of physical activity of athletes during quarantine was not examined, they had a low overall quality of sleep score. However, they were better than non-athletes on only three subscales of habitual sleep efficiency, sleep disturbances, and daytime dysfunction. Although this issue shows the positive effect of being an athlete on sleep quality, similar to the previous study, it also shows the effect of COVID-19 restrictions on athletes' sleep quality subscales. New findings have observed a relationship between stress and sleep quality (31). In the present investigation, regardless of the condition of the sports, the sleep quality of girls and boys did not differ significantly, which can be attributed to the high stress caused by COVID-19.
Our study has several limitations. Our results are based on self-report data, and we did not obtain data about influencing psychological conditions.
Overall, the results of the present study showed that athlete students had a higher sleep quality than non-athlete students. During the COVID-19 pandemic, athletes, both amateur and professional, were deprived of their sports activities. Examining the impact of the virus and its consequences on the sleep quality of these individuals is also worth considering. Given that there are still COVID-19 limitations in Iran at the time of writing this article, it is recommended that after these restrictions, motivational programs be developed to increase the level of physical activity to prevent the negative effects of quarantine on sleep quality that can affect student performance.