1. Background
Osteoporosis is a disease marked by reduced bone mass, deterioration of bone tissue, and microfractures that elevate the risk of bone fractures (1). It is the most common bone disease in humans and represents a major public health issue (2). The condition can be classified into two categories: Primary and secondary osteoporosis. Primary osteoporosis typically manifests in the seventh decade of life, associated with aging and gender differences. Although it affects both genders, women are more susceptible due to their lower bone mass and longer life expectancy. Secondary osteoporosis results from external factors, such as certain medications or disorders of the thyroid and parathyroid glands (3, 4).
The anticipated growth in the global elderly population is a significant factor contributing to the rapid increase in osteoporosis cases across many countries, especially in developing regions (5). Osteoporosis often remains undetected until a fracture occurs, which can lead to severe secondary health complications and even death (2). Pelvic fractures, in particular, pose the most severe complication of osteoporosis, with a mortality rate exceeding 20% within the first year following the fracture. Over half of the individuals experiencing these fractures are unable to return to an upright position. The initial diagnosis of osteoporosis is usually made after an acute clinical fracture or through a bone mineral density test, as radiographs are not a reliable indicator for diagnosis. Dual-energy X-ray absorptiometry (DXA, or DEXA) is the most precise method for assessing bone mineral density (6).
Fractures resulting from osteoporosis have emerged as a significant global health concern. The prevention of pathological fractures through the maintenance of bone density is currently achievable using both pharmacological and non-pharmacological treatment methods. A variety of drugs, including bisphosphonates and denosumab, have undergone extensive clinical trials to treat osteoporosis, yielding varied outcomes (6, 7).
Denosumab is a fully human monoclonal antibody of the immunoglobulin G2 subclass that inhibits the action of the receptor activator of nuclear factor kappa-B ligand (RANKL). Receptor activator of nuclear factor kappa-B ligand is a crucial regulator of osteoclastic bone resorption. By inhibiting the differentiation, activity, and survival of osteoclasts, denosumab reduces the rate of bone resorption and enhances bone mineral density, thereby diminishing the risk of bone fractures (8, 9).
2. Objectives
The risk of fractures among the elderly is projected to rise significantly in Iran due to the country's high aging rate. Furthermore, given the scarcity of research on the impact of denosumab on increasing bone mineral density in Iran, this study was undertaken to assess the change in bone density before and after a minimum of one year of treatment with denosumab in patients referred to two private clinics in Tehran.
3. Methods
This study was approved with the ethical code IR.AJAUMS.REC.1399.058 and received an RCT code of IRCT20210803052067N1 from AJA University of Medical Sciences. It was designed as a pre-post clinical trial. The participants consisted of 202 postmenopausal women, aged between 45 and 75, diagnosed with osteoporosis and scheduled to be treated with denosumab. The inclusion criteria were a T-score of bone density in the lumbar spine (L1 - L4) or femoral neck (or total) between -2 and -4 or patients at high risk of fracture according to FRAX criteria, which required drug treatment based on osteoporosis treatment guidelines. Exclusion criteria included sensitivity to denosumab or any component in its formulation (such as sorbitol, acetic acid, polysorbate 20, sodium hydroxide), a history of malabsorption, thyroidectomy, parathyroidectomy, bowel resection, or stages 4 and 5 renal failure. Participants who did not adhere to medication protocols or had malignant thyroid disease were also excluded from the study.
After obtaining consent from the participants, bone density and the risk of bone fracture were recorded on a checklist. Bone density was measured using the DXA method (with a Hologic Discovery Wi device). The risk of bone fracture was calculated using the FRAX instrument, an algorithm that estimates the 10-year probability of osteoporosis-related fractures based on clinical risk factors such as age, sex, BMI, and specific risk factors including a history of fragility fractures, parental history of fractures, smoking, prolonged use of glucocorticoids, rheumatoid arthritis, other causes of secondary osteoporosis, and alcohol consumption.
Denosumab 60 mg (Prolia, manufactured by Amgen) was administered in two doses as part of the treatment. The first dose was given after the initial bone density measurement, followed by a second dose six months later. Six months after receiving the second dose, bone density, and fracture risk were reassessed and documented on the checklist. The bone density and risk of bone fractures in patients before and after the treatment were then compared.
3.1. Data Analysis
The data were processed using SPSS version 23, where the mean and standard deviation for quantitative variables and the absolute and percentage frequencies for qualitative variables were calculated. The data distribution was normal. A statistically significant level was set at less than 0.05 for analyzing the data with the paired t-test.
4. Results
4.1. General Characteristics of Study Participants
The average age of the participants in this study was 69.0 ± 8.0 years, with an average height of 157 ± 5.46 cm and an average weight of 68.7 ± 8.29 kg. Additionally, the mean body mass index (BMI) of the participants was 27.9 ± 3.1. All participants had a history of undergoing treatment, as documented in Table 1.
| Parameter | Value a | Minimum | Maximum |
|---|---|---|---|
| Age, year | 69.0 ± 8.0 | 40 | 83 |
| Weight, kg | 68.7 ± 8.29 | 44 | 98 |
| Height, cm | 157.0 ± 5.46 | 137 | 170 |
| Body mass index, kg/m2 | 27.9 ± 3.1 | 20.30 | 38.30 |
a Values are expressed as man ± SD.
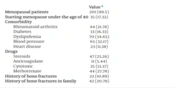
The study included 201 menopausal patients and 25 individuals under the age of 40. Among these participants, 44 had rheumatoid arthritis, 60 suffered from hypertension, 32 had diabetes, 70 were diagnosed with dyslipidemia, and 22 had heart disease, as detailed in Table 2.
A total of 47 patients received steroids; 11 were treated with anticoagulants, 25 with cytotoxic drugs, and 44 with methotrexate. Furthermore, 22 patients reported a history of prior fractures, and 42 had a family history of fractures, as indicated in Table 2.
| Value a | |
|---|---|
| Menopausal patients | 201 (99.5) |
| Starting menopause under the age of 40 | 35 (17.32) |
| Comorbidity | |
| Rheumatoid arthritis | 44 (21.78) |
| Diabetes | 33 (16.33) |
| Dyslipidemia | 70 (34.65) |
| Blood pressure | 65 (32.17) |
| Heart disease | 23 (11.38) |
| Drugs | |
| Steroids | 47 (23.26) |
| Anticoagulant | 11 (5.44) |
| Cytotoxic | 25 (13.37) |
| Methotrexate | 44 (27.78) |
| History of bone fractures | 22 (10.89) |
| History of bone fractures in family | 42 (20.79) |
a Values are expressed as No. (%).
Table 3 shows the frequency distribution of patients based on bone density in the spine and femur before starting treatment with denosumab.
| T-Score, g/cm2 | Spine | Femur |
|---|---|---|
| < -1 | 10 (4.95) | 11 (5.44) |
| -1.1 to -1.5 | 10 (4.95) | 23 (11.38) |
| -1.6 to -2 | 39 (19.30) | 34 (16.66) |
| -2.1 to -2.5 | 44 (21.78) | 63 (34.18) |
| -2.6 to -3 | 47 (23.26) | 28 (13.86) |
| -3 > | 52 (25.74) | 43 (21.28) |
| Total | 202 (100) | 202 (100) |
a Values are expressed as No. (%).
4.2. Comparison of the Bone Density of Study Participants Prior to and Following Treatment
As demonstrated in Table 4, the T-score of the spine and hip, along with the risk of bone fractures, showed significant improvement after denosumab treatment across all patients, regardless of age. This improvement was also observed across different age groups of patients before and after the treatment.
| Variables | Before | After | P-Value b |
|---|---|---|---|
| In all patient groups | |||
| Spine T-score, g/cm2 | -2.55 ± 0.06 | -2.00 ± 0.07 | 0.000 |
| Femoral T-score, g/cm2 | -2.10 ± 0.10 | -1.88 ± 0.06 | 0.023 |
| Risk of major fracture | 23.0 ± 1.9 | 18.9 ± 1.5 | 0.000 |
| Risk of fracture in the femur | 8.5 ± 1.3 | 5.7 ± 0.9 | 0.001 |
| Age group under 60 years | |||
| Spine T-score, g/cm2 | -2.40 ± 0.14 | -1.90 ± 018 | < 0.001 |
| Femoral T-score, g/cm2 | -2.10 ± 0.11 | -1.80 ± 0.11 | < 0.001 |
| Risk of major fracture | 14.90 ± 1.43 | 13.00 ± 1.31 | < 0.001 |
| Risk of fracture in the femur | 3.60 ± 0.85 | 2.3 ± 0.48 | 0.010 |
| Age group between 60 and 70 years | |||
| Spine T-score, g/cm2 | -2.50 ± 0.11 | -2.00 ± 0.12 | < 0.001 |
| Femoral T-score, g/cm2 | -2.10 ± 0.10 | -1.70 ± 0.10 | < 0.001 |
| Risk of major fracture | 17.70 ± 1.31 | 15.31 ± 1.06 | < 0.001 |
| Risk of fracture in the femur | 0.010 | ||
| Age group between 70 to 80 years | 5.00 ± 0.82 | 3.40 ± 0.51 | |
| Spine T-score, g/cm2 | -2.70 ± 0.10 | -2.10 ± 0.10 | < 0.001 |
| Femoral T-score, g/cm2 | -2.30 ± 0.10 | -2.00 ± 0.10 | < 0.001 |
| Risk of major fracture | 19.80 ± 0.95 | 18.30 ± 0.87 | < 0.001 |
| Risk of fracture in the femur | 0.010 | ||
| Age group between 80 to 90 years | 6.40 ± 0.61 | 5.60 ± 0.54 | |
| Spine T-score, g/cm2 | -2.20 ± 0.28 | -1.7 ± 0.33 | < 0.001 |
| Femoral T-score, g/cm2 | -2.20 ± 0.17 | -1.90 ± 0.16 | 0.030 |
| Risk of major fracture | 22.8 ± 2.55 | 19.77 ± 1.54 | 0.030 |
| Risk of fracture in the femur | 7.90 ± 1.41 | 5.70 ± 0.62 | 0.031 |
a Values are expressed as mean ± S.E.M and analyzed by paired student's t-test.
b P <0.05 was considered significant.
5. Discussion
Fractures significantly contribute to disability and medical costs (10, 11). Denosumab (Prolia), a human monoclonal antibody administered via subcutaneous injection, effectively inhibits bone resorption by blocking the formation and activity of osteoclasts. The regimen requires a 60 mg dose every six months. Research indicates that a subcutaneous injection of 60 mg of denosumab every six months diminishes bone resorption and enhances bone mineral density (12-15).
In this study, the bone density of 202 patients receiving two doses of 60 mg denosumab every six months was examined. The results demonstrated a significant increase in the mean T-score of the spine and bones of patients before and after denosumab administration, indicating a shift from osteoporosis to osteopenia after one year. This finding aligns with the results of Lewiecki et al., where denosumab also increased bone density at all measured sites and reduced bone resorption, although their study compared denosumab to a placebo (13). Additionally, Miller et al. found that bone mineral density in patients treated with denosumab was significantly higher than in those treated with zoledronic acid (16). Petranova et al. reported a 3.9% increase in bone mineral density in the lumbar spine and a 1.3% increase in the femur with denosumab 60 mg injected subcutaneously twice a year in their study (17). Based on the outcomes of this research and those of other studies, it can be concluded that denosumab increases bone mineral density in Iranian patients.
In this study, treatment with denosumab significantly lowered the risk of major and hip fractures according to FRAX criteria. Petranova et al. reported a 13.3% decrease in the risk of major osteoporotic and acute fractures based on FRAX after using denosumab (17). Cummings et al. found that denosumab reduced the incidence of new vertebral fractures, hip fractures, and non-vertebral fractures compared to a placebo (8). Similarly, Pongchaiyakul et al. observed that women at high risk of osteoporosis who received denosumab experienced fewer pelvic and vertebral fractures than those who did not receive the drug (18).
5.1. Conclusions
The findings of this study indicate that denosumab enhances bone density and reduces the risk of bone fractures in postmenopausal women, including those in Iran. While some studies involved more frequent injections over a longer duration, this study demonstrates that just two doses at six-month intervals are sufficient to achieve the desired effect. Denosumab proves to be an effective medication for increasing bone density in postmenopausal women and reducing their risk of fractures.
One limitation of this study was its small sample size; future research in this area is recommended to be conducted on a larger scale. Additionally, the study did not include a control group due to the complications associated with discontinuing treatment in osteoporosis patients, which represents another limitation.