1. Background
Obesity is a major complex health concern with an increasing prevalence. Approximately 1.9 billion adults are overweight, and 610 million adults are obese (1, 2). Furthermore, obesity is associated with other health concerns such as diabetes, cardiovascular disease, and hypertension, all of which result in decreased life expectancy and quality of life (3). Metabolic and bariatric surgery is considered one of the safest and best choices for severe obesity, resulting in long-term weight loss (4, 5), improvement of obesity-related morbidity (6-9), and decreased mortality (10, 11) compared with nonsurgical options. The most common metabolic and bariatric surgeries are Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy (LSG) (12). Due to its higher effectiveness and fewer postoperative complications, LSG is considered the preferred procedure for bariatric surgery (13, 14). Bariatric procedures are associated with various micronutrient and vitamin deficiencies, such as deficiencies in zinc, vitamin B12, and vitamin D (15, 16).
Vitamin D is a steroid hormone pivotal for calcium homeostasis and bone mineralization. Furthermore, vitamin D is involved in many nonclassical actions, and vitamin D deficiency is related to cancer, diabetes, cardiovascular, and autoimmune diseases (17). There are concerns that serum vitamin D levels may be adversely affected by bariatric surgery (18). Studies have demonstrated that following bariatric surgery, mean vitamin D levels remained ≤ 30 ng/mL (75 nmol/L) despite various vitamin D replacement therapies (19). However, other studies have shown no significant difference in vitamin D levels after surgery (20).
2. Objectives
Considering the high prevalence of obesity and the increasing number of bariatric surgeries, as well as the significant complications of vitamin D deficiency, this study was conducted to investigate the effect of LSG on vitamin D levels.
3. Methods
3.1. Study Design
This retrospective study was conducted at Shahid Modarres Hospital in Tehran, Iran, in 2023. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, and approval for the study was obtained from the Institutional Review Board at Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1401.878). Signed consent forms were also obtained from all participants.
Three hundred patients with a body mass index (BMI) ≥ 40 kg/m² or a BMI between 35 kg/m² and 40 kg/m² with at least two comorbidities, such as diabetes mellitus or hypertension, who underwent LSG were enrolled using a non-probability sampling method. Patients with a history of diseases such as tuberculosis, sarcoidosis, and malnutrition, incomplete documents, failure to attend follow-ups, or lack of consent to participate in the study were excluded. All patients used a vitamin D supplement of 50,000 units per month (in capsule form), and those who did not follow the treatment were excluded from the study.
Demographic and general information such as age, education, height, weight, BMI, past medical history, previous history of vitamin D intake, and serum levels of calcium, parathyroid hormone (PTH), and vitamin D before and after surgery were recorded in a checklist.
3.2. Vitamin D Level Assay
The serum levels of PTH, vitamin D (IDS, UK), and calcium were measured using a single kit in a single laboratory (Pathobiology Laboratory Center of Shahid Modarres Hospital, Tehran, Iran) by the ELISA method.
3.3. Statistical Analysis
Data were analyzed using paired Student's t-test and Pearson’s correlation with SPSS v.26 software (IBM, Chicago, IL, USA). A P-value of < 0.05 was considered significant.
4. Results
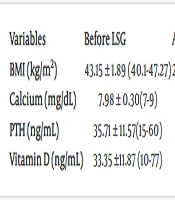
After applying the exclusion criteria, 245 patients who underwent LSG were finally enrolled. The majority of the patients were female (82.4% female versus 17.6% male). The mean age of patients was 34.98 ± 8.49 years (range 20 - 60) at the time of surgery. The mean BMI was 43.15 ± 1.89 kg/m² (range 40.1 - 47.27) before LSG and 29.83 ± 4.53 kg/m² (range 21.60 - 43.28) after LSG. Among the cases recruited, 31.4% used calcium supplements and 17.5% used vitamin D supplements.
Analytic analysis demonstrated a statistically significant difference in vitamin D and calcium levels before and after LSG (P < 0.001 for both). However, the difference in PTH levels before and after LSG was not statistically significant (P = 0.10) (Table 1). Furthermore, the study results demonstrated no statistically significant relation between vitamin D and calcium supplement intake (P = 0.5 for vitamin D, P = 0.6 for calcium). Analytic analysis also demonstrated no statistically significant relation between vitamin D levels and PTH levels (r = 0.56, P = 0.1).
| Variables | Before LSG | After LSG | P-Value b |
|---|---|---|---|
| BMI (kg/m2) | 43.15 ± 1.89 (40.1 - 47.27) | 29.83 ± 4.53 (21.60 - 43.28) | < 0.0001 |
| Calcium (mg/dL) | 7.98 ± 0.30 (7 - 9) | 8.06 ± 0.38 (7 - 9) | < 0.001 |
| PTH (ng/mL) | 35.71 ± 11.57 (15 - 60) | 36.37 ± 10.72 (19 - 59) | 0.1 |
| Vitamin D (ng/mL) | 33.35 ± 11.87 (10 - 77) | 38.08 ± 16.29 (14 - 85) | < 0.001 |
Serum Levels of the Studied Variables Before and After the Laparoscopic Sleeve Gastrectomy (LSG) a
5. Discussion
Changes in habits and lifestyles, expansion of urbanization, and inactivity have led to an increase in the prevalence of obesity. Obesity is associated with many complications and leads to increased mortality and morbidity. Despite all the treatments used to lose weight, bariatric surgery is still considered the most effective and cost-effective way to treat obesity. Contrary to all the beneficial effects of bariatric surgery, the results of some studies indicate nutritional deficiencies in micronutrients after bariatric surgery. One of these micronutrients is vitamin D, which plays an important role in the health and immunity of the body. Therefore, the aim of this study was to investigate the effect of LSG on the level of vitamin D after 4 years of follow-up of patients.
Our findings demonstrated a statistically significant difference between vitamin D level and calcium level before and after LSG (P-value < 0.001 for both). However, the relation between PTH before and after LSG was not statistically significant (P-value = 0.10).
In this regard, Ali et al. (20), reported that after 12 months of follow-up in 40 patients, the level of vitamin D and calcium increased significantly after LSG. The results of that study are similar to the present study. However, contrary to the results of that study, no significant change in PTH level was observed. The present study was conducted with a larger sample size, which can justify the difference in the results. Additionally, Fox et al. (21) also reached similar results in a 4-year study of 460 patients regarding the increase in vitamin D levels, which is consistent with the present study. In 2023, Rashnoo et al. (22) studied 120 patients who underwent LSG and reported that the level of vitamin D after one year was significantly higher than before the operation, which results are similar to the present study. Musella et al. (23) also reported that the prevalence of vitamin D deficiency and insufficiency decreased significantly after LSG.
The results of a study by Ruiz-Tovar et al. (24) in 2012 showed that LSG increases the level of vitamin D, which is similar to the results of the present study. However, contrary to the results of this study, the PTH level decreased significantly, and the calcium level remained unchanged. It is important to note that the mentioned study only examined women with morbid obesity, and this difference in the statistical population may account for the difference in the results.
Additionally, studies have investigated the differences between various bariatric surgery techniques on vitamin D levels. In this regard, Rodrigues et al. (25) reported in 2020 that patients undergoing the LSG procedure had better weight loss outcomes and were at a lower risk of vitamin D inadequacy than those undergoing RYGB. In the present study, although the effect of various bariatric surgery techniques on vitamin D levels was not investigated, the results of increasing vitamin D levels after LSG are similar to the results of the mentioned study.
The limitations of the present study include the absence of a control group and the lack of examination of various bariatric surgery techniques. However, the high sample size and long-term follow-up are the strengths of this study.
5.1. Conclusions
The results of the present study showed that 4 years after LSG, vitamin D and calcium levels increased significantly in patients with morbid obesity, although the observed increase in PTH levels was not statistically significant. According to the results of the present study and similar studies, LSG may be associated with a decrease in vitamin D levels, but if vitamin D supplementation is continued, its levels will remain at an optimal level.