1. Background
Nosocomial infections are those acquired following the provision of medical and health services in healthcare settings. These infections can appear during a patient's hospital stay or even after discharge (1). Hospital-acquired infections are a problem in healthcare facilities worldwide. The World Health Organization has renamed nosocomial infections as "infections associated with healthcare facilities" to emphasize that these infections are not exclusive to hospitals; they can occur in any healthcare setting, even in the most equipped and modern hospitals in advanced countries (2, 3). Among these, fungal infections are particularly concerning in high-risk hospital departments. Opportunistic fungi can cause invasive infections in patients with immunodeficiency and other health issues, although they typically do not affect individuals with healthy immune systems (4).
Fungi have a high adaptability to various environmental conditions. However, fungal contamination in indoor environments depends on several factors, including humidity, ventilation, temperature, the presence of organic matter in building materials, fungal load in the exterior of the building, and construction activities. Important fungi that cause invasive fungal infections include Candida yeast species, Aspergillus species, Zygomycetes such as Mucor and Rhizopus, and fungal agents like the genus Fusarium, which are also significant in causing opportunistic invasive infections (5, 6).
Currently, there is an increasing prevalence of hospital-acquired fungal infections, particularly in operating rooms, ICU departments, and units for blood transfusions, transplants, burns, and dialysis. These infections have become a significant health issue globally (7). Inpatient wards are particularly vulnerable to fungal contamination due to factors such as the physical and mental weakness of patients, requiring special care and design to prevent and reduce fungal contamination (8). Many studies have shown a significant relationship between hospital-acquired infections and fungal aerosols in these settings (9). Most microorganisms present in hospital environments become opportunistic pathogens, especially in immunocompromised patients (10).
Due to the ubiquitous presence of fungi, the widespread use of antibiotics, treatment methods, and patient isolation (which reduce bacterial infections), fungal infections have become an increasing problem over the past few years. Despite special care to reduce air pollution by fungal agents in certain departments, the air in many hospital wards with immunocompromised patients still contains many fungal agents (11). Studies conducted in Iran on the prevalence of hospital-acquired infections and the resulting extended hospital stays and associated costs demonstrate that these infections are a major medical, social, and economic problem. As treating these infections imposes significant costs on the healthcare sector, implementing infection control programs or even minor but effective changes in the practices of healthcare workers to control hospital infections could be highly beneficial and cost-effective from a health economics perspective (12). Therefore, increasing the awareness of healthcare center personnel about the importance of infection control is crucial for all hospital infection control programs. Given the high prevalence and mortality associated with fungal infections among hospital-acquired infections, it is essential to assess the awareness of department personnel to minimize the consequences and complications of these infections.
2. Objectives
This study aimed to investigate the average knowledge score of nurses in Zahedan teaching hospitals regarding fungal infections in 2023.
3. Methods
This study was a descriptive, cross-sectional study conducted in 2023. The study population included all nurses working at Zahedan University Teaching Hospitals, specifically Khatam Al Anbia, Ali Ebn Abitaleb, and Bu Ali Hospitals. The inclusion criteria were nurses working in these hospitals in 2023 who had at least one year of work experience and were willing to complete the questionnaire. The exclusion criteria were nurses who were unwilling to participate, did not complete the questionnaire, or had less than one year of work experience. Based on previous studies, the estimated sample size was 342 cases (13).
The data collection tool for this study was a two-part questionnaire. The first part included demographic information: Age, gender, education level, work experience, and workplace hospital. The second part was a researcher-designed questionnaire to assess the level of knowledge about fungal infections among the study population. The range of scores for each section and the overall score was divided into four levels of awareness: very low, low, moderate, and high (epidemiology: 0 - 1 very low, 2 - 3 low, 4 moderate, 5 high; prevention: 0 - 3 very low, 4 - 5 low, 6 - 7 high; treatment: 0 - 1 very low, 2-3 low, 4 high). To determine the validity of the data collection tool, the questionnaire was distributed among several experts in the fields of fungal infections and medicine, and their feedback was incorporated. The reliability score, as measured by Cronbach's alpha, was estimated at 0.86.
The population studied in this research included all nurses working in Zahedan teaching hospitals in 2023, selected through the convenience sampling method. Upon entering the study, the researcher introduced themselves to the participants and explained the purpose of the study. Informed consent was obtained from all participants, and the study was conducted in accordance with ethical principles, including only those nurses who were willing to participate. Data analysis was performed using SPSS version 26 software, with a significance level of P-value ≤ 0.05.
4. Results
In the present study, data were collected from 342 nurses working in Zahedan teaching hospitals. The average age of the nurses was approximately 36 years. The average work experience of the studied group was around 133 months (Table 1).
| Variables | Numbers of Samples | Mean ± Standard Deviation | Minimum-Maximum |
|---|---|---|---|
| Age | 342 | 40.70 ± 36.8 | 26 - 54 |
| Work experience | 342 | 237.85 ± 133.02 | 12 - 479 |
The findings from the first part of the study show that the highest knowledge score regarding fungal infections was in the field of prevention (4.79), while the lowest knowledge score was in the field of treatment (1.9) (Table 2).
| Variables | Mean ± SD | Samples Number |
|---|---|---|
| Epidemiology | 2.48 ±1.74 | 342 |
| Diagnosis | 3.47 ±2.27 | 342 |
| Treatment | 1.90 ± 1.40 | 342 |
| Prevention | 4.79 ± 2.93 | 342 |
| Total score awareness | 12.63 ±4.53 | 342 |
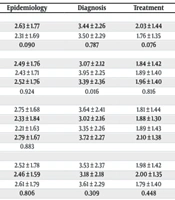
As shown in Table 3, the average total awareness score regarding fungal infections is higher for women than for men. Additionally, the findings indicate that there was no significant difference between gender and the knowledge of fungal infections in the different areas of epidemiology, diagnosis, treatment, and prevention, based on the P-values obtained from the independent t-test. However, there was a significant relationship between gender and the mean knowledge score of fungal infections in the field of diagnosis among nurses working in Zahedan teaching hospitals (P-value: 0.016). No significant relationships were observed between workplace, education level, and knowledge scores across different groups.
| Variables | Awareness Total Score | Epidemiology | Diagnosis | Treatment | Prevention |
|---|---|---|---|---|---|
| Sexuality | |||||
| Male | 12.76 ± 4.46 | 2.63 ± 1.77 | 3.44 ± 2.26 | 2.03 ± 1.44 | 4.67 ± 2.97 |
| Female | 12.49 ± 4.61 | 2.31 ± 1.69 | 3.50 ± 2.29 | 1.76 ± 1.35 | 4.92 ± 2.90 |
| P-value | 0.580 | 0.090 | 0.787 | 0.076 | 0.431 |
| Age | |||||
| 26 - 35 | 12.03 ± 4.32 | 2.49 ± 1.76 | 3.07 ± 2.12 | 1.84 ± 1.42 | 4.62 ± 3.08 |
| 36 - 45 | 13.25 ± 4.54 | 2.43 ± 1.71 | 3.95 ± 2.25 | 1.89 ± 1.40 | 4.99 ± 2.97 |
| 46 - 55 | 12.61 ± 4.65 | 2.52 ± 1.76 | 3.39 ± 2.36 | 1.96 ± 1.40 | 4.75 ± 2.79 |
| P-value | 0.135 | 0.924 | 0.016 | 0.816 | 0.639 |
| Education | |||||
| Ph.D. | 12.41 ± 3.97 | 2.75 ± 1.68 | 3.64 ± 2.41 | 1.81 ± 1.44 | 4.22 ± 2.57 |
| M.Sc. | 11.99 ± 4.16 | 2.33 ± 1.84 | 3.02 ± 2.16 | 1.88 ± 1.30 | 4.76 ± 2.65 |
| B.Sc. | 12.13 ± 4.71 | 2.21 ± 1.63 | 3.35 ± 2.26 | 1.89 ± 1.43 | 4.68 ± 2.76 |
| BA. | 13.53 ± 4.54 | 2.79 ± 1.67 | 3.72 ± 2.27 | 2.10 ± 1.38 | 4.92 ± 2.90 |
| P-value | No | 0.883 | |||
| Work location | |||||
| Ali Ebn Abitaleb | 12.88 ± 4.33 | 2.52 ± 1.78 | 3.53 ± 2.37 | 1.98 ± 1.42 | 4.85 ± 2.75 |
| Bu Ali | 12.20 ± 4.38 | 2.46 ± 1.59 | 3.18 ± 2.18 | 2.00 ± 1.35 | 4.57 ± 2.73 |
| Khatam Al Anbia | 12.54 ± 4.45 | 2.61 ± 1.79 | 3.61 ± 2.29 | 1.79 ± 1.40 | 4.54 ± 2.72 |
| P-value | No | 0.806 | 0.309 | 0.448 | 0.634 |
a Values are expressed as mean ± SD.
5. Discussion
This study aimed to evaluate the level of knowledge about fungal infections among nursing staff in Zahedan educational-medical hospitals in 2023. The findings showed that nurses' general knowledge about fungal infections is relatively low, with most participants falling into the "low knowledge" category. This is concerning because nurses play a critical role in patient care, particularly in managing and preventing hospital-acquired infections, including fungal infections (14).
Data were collected from 342 nurses working in teaching hospitals in Zahedan. The average age of the nurses was 40.70 ± 8.36 years, and their average work experience was 133.02 ± 237.85 months. In terms of gender, 181 (52.92%) nurses were female, and 161 (47.08%) were male. The average total score for nurses' awareness of fungal infections was 12.63 ± 4.53 out of 25 possible points, indicating that most nurses have a basic awareness but lack a comprehensive understanding of fungal infections.
The results showed no significant differences in the average total awareness scores across different groups based on work experience (1 - 5 years: 11.23 ± 4.89, 6-10 years: 12.62 ± 4.25, more than 10 years: 12.83 ± 4.51; P-Value = 0.146), gender (female: 12.76 ± 4.46, male: 12.49 ± 4.61), age (26 - 35 years: 12.03 ± 4.32, 36-45 years: 13.25 ± 4.54, 46-55 years: 12.61 ± 4.65; P-value = 0.135), education level (diploma: 12.74 ± 4.97, bachelor's degree: 12.63 ± 4.49; P-value = 0.882), or hospital affiliation (Ali Ebn Abitaleb: 12.88 ± 4.33, Bu Ali: 12.20 ± 4.38, Khatam Al Anbia: 12.54 ± 4.45; P-value = 0.510). These findings suggest that the level of awareness about fungal infections is similar among different groups. The average overall awareness score of 12.63 ± 4.53 out of a possible 25 points indicates that most nurses have a basic awareness but lack a comprehensive understanding of fungal infections. This finding is concerning because it suggests a widespread lack of awareness that could have serious implications for patient care and safety. While our study is among the first to specifically assess nurses' awareness of fungal infections in this region, other studies globally have raised similar concerns about healthcare workers' knowledge of nosocomial infections (15, 16).
The fact that over 70% of nurses had very low or low awareness about fungal infections is particularly concerning. Fungal infections, once considered rare, are now recognized as a significant cause of morbidity and mortality in immunocompromised patients (17). A study by Perlroth et al., consistent with the present study, showed that the prevalence of invasive fungal infections has increased significantly in the last two decades (18). In this context, the low level of awareness among nurses in Zahedan could lead to delayed diagnoses, incorrect management, and an increased risk of nosocomial fungal infections.
The distribution of awareness scores across different domains provides additional insights, highlighting a lack of understanding about the prevalence, incidence, and risk factors of fungal infections. Research by Vallabhaneni et al. emphasized that understanding the epidemiology of fungal infections is crucial for their prevention and control (19). Without this awareness, nurses may fail to recognize high-risk patients or situations, leading to missed prevention opportunities. In the domain of prevention, more than 60% of nurses showed very low or low awareness. A study by Kaur and Chakrabarti demonstrated that simple preventive measures, such as hand hygiene, environmental cleaning, and judicious use of antibiotics, can significantly reduce the prevalence of nosocomial fungal infections (20).
The low awareness among nurses in Zahedan highlights a critical gap in the implementation of vital preventive measures, which may increase the risk of fungal infections in these hospitals. The awareness scores related to diagnosis are also concerning, with more than 60% of nurses falling into the categories of very low or low awareness. This lack of awareness can lead to delayed or missed diagnoses, which is particularly problematic for fungal infections. As noted by Rautemaa-Richardson et al., early and accurate diagnosis is essential for the effective management of fungal infections, as delays can lead to the spread of infection and worse outcomes (21). The low diagnostic awareness among nurses may contribute to such delays and underscores the need for targeted training in this area.
Similarly, in the field of treatment, over 60% of nurses had very low or low knowledge. While nurses may not prescribe antifungal treatments, their understanding of these treatments is essential for proper use, monitoring for side effects, and patient education. Menzin et al. found that incorrect antifungal treatment can lead to increased mortality and healthcare costs (22). Therefore, improving nurses' knowledge about antifungal treatments is critical for optimal patient care.
Interestingly, the study did not reveal significant differences in awareness scores based on factors such as work experience, gender, age, education level, or hospital. This suggests that low awareness is a systemic problem and not confined to specific groups. This finding contradicts some studies, such as the one by Sessa et al. in Italy, which showed that knowledge about nosocomial infections increased with years of experience (15). The absence of such a trend in this study may indicate a lack of continuous professional development and highlight the need for targeted and mandatory training programs for all nurses, regardless of their experience or qualifications.
The persistently low awareness across various hospitals in Zahedan (Imam Ali, Bu Ali, and Khatam Al Anbia) also points to a problem at the city or possibly regional level. This issue suggests the need for a coordinated, multi-institutional approach to improving awareness of fungal infections. A study by Safdar and Abad emphasized that successful infection control programs require a multidisciplinary approach and institutional commitment (23). Therefore, healthcare managers in Zahedan should consider developing and implementing a comprehensive city-wide educational program on fungal infections.
The implications of these findings are significant. Nurses' lack of knowledge about fungal infections can lead to increased rates of nosocomial fungal infections, delayed diagnoses, mismanagement, and ultimately poorer patient outcomes. A study by Chakrabarti et al. in India found a prevalence of nosocomial fungal infections as high as 6.4%, with significant mortality attributed to them (24). Although specific data for Zahedan is not available, the low levels of awareness suggest that the risk could be similarly high. Additionally, the economic impact of nosocomial fungal infections is considerable. A study by Borg estimated that each case of nosocomial candidemia (a type of fungal infection) resulted in substantial additional hospitalization costs (25). Given the resource constraints in many health systems, including Iran, the potential financial burden of nosocomial fungal infections due to low awareness is a critical concern.
5.1. Conclusions
Overall, the results indicate that a significant majority of nurses have limited general awareness about fungal infections. This trend is consistent across all evaluated areas: Epidemiology, prevention, diagnosis, and treatment. The absence of significant differences in knowledge scores based on factors such as work experience, gender, age, education level, or hospital affiliation suggests that this lack of awareness is a systemic issue, not limited to specific groups. This underscores the need for comprehensive, institution-wide interventions targeting all nursing staff. Given that fungal infections are increasingly recognized as important contributors to morbidity, mortality, and healthcare costs, particularly in vulnerable patient populations, the low level of awareness among frontline healthcare providers is alarming and must be addressed.