1. Background
Coronary heart disease is a major global cause of mortality, with atherosclerosis being the primary underlying condition, leading to the formation of calcified plaques. The burden of coronary atherosclerosis is quantitatively assessed through calcium scoring, a well-established parameter in computed tomography (CT) imaging of coronary arteries. Various studies have identified the coronary artery calcification score as an independent and robust predictor of morbidity and mortality related to coronary atherosclerotic diseases (1-6). Calcification can occur not only in arterial vessels but also in the aortic and mitral valves, both of which can be evaluated using CT techniques.
Despite the potential clinical significance, coronary CT studies often do not include assessments of aortic and mitral valve calcium scores. It has been reported that the aortic valve calcium score is strongly correlated with aortic stenosis (5). Aortic stenosis is the third most prevalent cardiovascular disease, following coronary artery disease and hypertension, with an increasing incidence in Asia and other regions due to rising life expectancy. Mitral valve calcification, on the other hand, has been associated with an elevated risk of stroke, atrial fibrillation, and cardiovascular mortality (6-8). Research into the pathophysiology of aortic and mitral valve calcification remains an active area of investigation. However, studies have shown that valve calcification and coronary atherosclerosis share similar risk factors (9-11).
Coronary atherosclerosis occurs when the lining of the heart's blood vessels becomes dysfunctional, leading to the activation of chronic inflammatory factors. Similarly, histopathological studies have identified endothelial damage and inflammation in calcified aortic and mitral valves (12). These findings suggest that the mechanisms underlying coronary artery, aortic, and mitral valve calcification may overlap. Despite the similarities in the literature regarding these calcifications, the precise relationship between coronary artery calcification and calcifications in the aorta or mitral valve remains unclear.
2. Objectives
The present study aimed to investigate the correlation between coronary artery calcification scores and aortic artery calcification, as well as calcification in the mitral and aortic valves. This research seeks to contribute to the understanding of the shared and distinct mechanisms underlying these forms of calcification.
3. Methods
3.1. Study Population
This cross-sectional study was conducted with patients consecutively referred to Modarres Hospital in Tehran with suspected coronary artery disease, who were evaluated using chest CT scanning. Exclusion criteria included low image quality, a history of any coronary or valvular diagnostic or therapeutic intervention, a history of heart valve diseases, endocarditis, or any type of cardiomyopathy, a history of congenital heart disorders, and the presence of any abnormal morphology in the aorta or heart valves. The various stages of this project were approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.MSP.REC.1403.077).
3.2. Study Assessments
Initially, through patient interviews, background information, including demographic characteristics, was collected. The study checklist documented participants' medical history, including hypertension, diabetes, hyperlipidemia, family history of heart disease, and history of smoking or opium use. Patients underwent chest CT evaluation, and the calcium score in the coronary arteries, aortic artery (at different sections), and the mitral and aortic valves was determined using the Agatston method with Syngo.via software. All imaging was conducted by an experienced radiologist with over 10 years of expertise in imaging.
The calcium score for the aortic valve was measured from the sinotubular junction to the aortic valve leaflets, while the mitral valve calcium score was assessed between the left atrium and left ventricle, including the leaflets. All measurements were performed by the radiologist to ensure consistency and accuracy. Finally, the correlation between the coronary artery calcification score and the calcification scores at the three positions—the aortic artery, aortic valve, and mitral valve—was analyzed.
3.3. Statistical Analysis
Quantitative data were expressed as mean ± standard deviation (SD), while categorical variables were presented as percentages. The chi-square test was employed to compare qualitative variables. Data analysis was performed using SPSS software, version 23, and a significance level of less than 0.05 was considered statistically significant.
4. Results
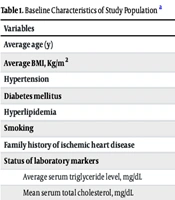
A total of 100 patients were included in the study, with a mean age of 60.9 ± 6.6 years, of whom 70% were male. The mean Body Mass Index (BMI) was 28.2 ± 2.5 kg/m². Regarding cardiovascular risk factors, the prevalence of hypertension was 38%, diabetes was reported in 30% of patients, hyperlipidemia was present in 26%, and 15% were current smokers. Additionally, 35% of the patients had a family history of ischemic heart disease. The baseline characteristics and laboratory marker statuses are detailed in Table 1.
| Variables | Values |
|---|---|
| Average age (y) | 60.9 ± 6.6 |
| Average BMI, kg/m2 | 28.2 ± 2.5 |
| Hypertension | 38 |
| Diabetes mellitus | 30 |
| Hyperlipidemia | 26 |
| Smoking | 15 |
| Family history of ischemic heart disease | 0.35 |
| Status of laboratory markers | |
| Average serum triglyceride level, mg/dL | 135 ± 45 |
| Mean serum total cholesterol, mg/dL | 220 ± 18 |
| Mean serum HDL level, mg/dL | 44 ± 11 |
| Mean serum LDL level, mg/dL | 130 ± 30 |
| Mean serum hemoglobin level, mg/dL | 12.2 ± 1.0 |
| Mean serum CRP level, mg/dL | 0.15 ± 0.10 |
Abbreviation: BMI, Body Mass Index.
a Values are expressed as mean ± SD or %.
Based on CT scan findings, aortic arch calcification was observed in 50% of patients, ascending aortic calcification in 20%, descending aortic calcification in 60%, aortic valve calcification in 18%, and mitral valve calcification in 3%. The mean calcium scores were 390 for the aortic arch, 52 for the ascending aorta, 565 for the descending aorta, and 529 for the coronary arteries.
Among the 100 patients studied, 18% had no coronary artery calcification (CAC = 0), 4% had minimal calcification, 20% had mild calcification, 15% had moderate calcification, 18% had severe calcification, and 25% had extreme calcification.
An analysis of the relationship between aortic calcification frequency and coronary artery calcification severity (Table 2) revealed that none of the patients without calcification or with minimal coronary calcification exhibited calcification in any position of the aortic artery. Among patients with mild, moderate, severe, and extreme coronary calcification, the frequency of aortic arch calcification was 5%, 12%, 8%, and 25%, respectively. The frequency of ascending aorta calcification was 0%, 5%, 5%, and 10%, respectively, while the frequency of descending aorta calcification was 10%, 10%, 15%, and 25%, respectively. Overall, a significant relationship was found between the frequency of coronary artery calcification and aortic artery calcification (P = 0.008).
| Zone | None | Minimal | Mild | Moderate | Severe | Extreme | P-Value b |
|---|---|---|---|---|---|---|---|
| Aortic arch | 0 | 0 | 5 | 12 | 8 | 25 | 0.008 |
| ascending aorta | 0 | 0 | 0 | 5 | 5 | 10 | |
| Descending aorta | 0 | 0 | 10 | 10 | 15 | 25 |
a Values are expressed as %.
b The analysis was performed by the chi-square test.
Similarly, when evaluating the relationship between the average score of aortic calcification and the severity of coronary artery calcification (Table 3), it was observed that none of the patients without calcification or with minimal coronary calcification exhibited calcification in any position of the aortic artery. Among patients with mild, moderate, severe, and very severe coronary calcification, the mean score of aortic arch calcification was 36, 60, 700, and 1300, respectively. The mean score of ascending aorta calcification was 0, 50, 200, and 400, respectively, while the mean score of descending aorta calcification was 150, 400, 900, and 1500, respectively. There was a significant correlation between the severity of coronary artery calcification and the average score of aortic artery calcification (P = 0.001) (Table 3).
| Zone | None | Minimal | Mild | Moderate | Severe | Extreme | P-Value a |
|---|---|---|---|---|---|---|---|
| Aortic arch | 0 | 0 | 36 | 60 | 700 | 1300 | 0.001 |
| ascending aorta | 0 | 0 | 0 | 50 | 200 | 400 | |
| Descending aorta | 0 | 0 | 150 | 400 | 900 | 1500 |
a The analysis was performed by the chi-square test.
5. Discussion
The present study was designed and conducted to evaluate the relationship between coronary artery calcification and calcification in other parts of the cardiovascular system, such as the aorta. This investigation was based on the assumption that calcification can occur simultaneously across various regions of the cardiovascular system, a concept of critical importance for radiological interpretation and the assessment of vascular involvement severity. Our findings demonstrate that the severity of coronary artery calcification correlates with the severity and extent of calcification in different segments of the aorta. Specifically, both the number of calcified points and the scores indicating the intensity of involvement align closely between the coronary arteries and the aorta.
Recent studies suggest that calcification in various coronary arteries is associated with calcification in other cardiovascular regions, including heart valves and different sections of the aorta. The calcification process appears to follow a similar pathophysiology across these regions, leading to concurrent events in multiple areas of the cardiovascular system. According to research, this similarity arises from the shared underlying risk factors for cardiovascular diseases that predispose all parts of the cardiovascular system to calcification.
In our study, we explored the relationship between coronary artery calcification and the severity of aortic artery calcification. Notably, none of the patients without coronary artery calcification exhibited calcification in any part of the aorta. Conversely, the frequency and score of calcification in various segments of the aorta increased proportionally with the severity of coronary artery calcification. Specifically, greater calcification in the coronary arteries was associated with increased calcification in the aortic arch, ascending aorta, and descending aorta.
This finding is significant because the presence of coronary artery calcification can serve as a reliable predictor of calcification and, consequently, the activation of the atherosclerotic process in different parts of the aorta. Similarly, the presence of aortic calcification could predict coronary artery involvement, emphasizing the interconnected nature of calcification within the cardiovascular system.
Such a relationship has also been demonstrated in previous studies, although not all have confirmed a statistically significant association. In the study by Suwita et al., a significant but weak correlation was observed between coronary artery calcium scores and aortic artery calcium scores (13). Similarly, Hata et al. found that among different sections of the aorta, the highest calcification frequency occurred in the aortic arch (77.4%). Significant coronary artery calcification was observed in 39.1% of cases, and calcification in various areas of the aorta and aortic valve was significantly associated with coronary artery calcification, even after adjusting for cardiovascular risk factors and statin use (14).
In the study by Allison et al., adjustments for age, gender, and cardiovascular risk factors revealed that individuals with calcification in the thoracic aorta had the highest likelihood of annular calcium, while those with calcification in the abdominal aorta were more likely to have mitral valve calcification. Calcium increases in the abdominal and iliac aorta were significantly associated with calcium in the aortic annulus, and calcification in the thoracic aorta was significantly linked to calcium in the mitral annulus (15). This study underscored that calcification occurring in one part of the aorta is often related to calcification in other regions, with a widespread and simultaneous pattern of involvement across different areas.
More intriguingly, some studies have shown that calcification in the aorta may coincide with calcification in other vascular systems, such as the cervical and cerebral arteries (16). This suggests that calcification is a systemic phenomenon. Once the process is activated, it is not confined to a single area of the cardiovascular system. Instead, activation in one part can lead to widespread involvement in other regions. Therefore, understanding and identifying calcification in one part of the cardiovascular system could have broader implications for predicting and managing calcification in other areas.
5.1. Conclusions
As a final conclusion, our study demonstrated that the occurrence of calcification in the aorta (observed in 82% of cases) was associated with a 20 - 60% prevalence of calcification in various segments of the aorta. This finding highlights that calcification in the coronary arteries is closely and simultaneously accompanied by the progression of calcification in different sections of the aorta. Furthermore, our results revealed a strong correlation between the severity of coronary artery calcification and both the frequency and score of calcification in the aorta. This underscores the systemic and simultaneous nature of calcification, indicating that calcification in one part of the cardiovascular system often reflects widespread involvement in other regions.