1. Background
The glenohumeral joint, also known as the shoulder joint, is one of the most mobile joints in the skeletal system. However, this exceptional mobility comes at the cost of stability. A critical component in maintaining the integrity of the glenohumeral joint is the labrum. Anterior labrum injuries and various pathologies are often associated with anterior displacement of the humerus. Such injuries compromise the labrum's stabilizing mechanism, increasing the risk of shoulder dislocations (1). Additionally, traumatic injuries to the glenoid, including fractures and dislocations, or its biomechanical characteristics, such as glenoid inclination and version relative to the humerus, can impact the stability and function of the shoulder joint. These conditions may lead to pain, limited movement, and a higher susceptibility to future injuries, often requiring medical intervention and rehabilitation to restore normal shoulder function (1).
Anterior labrum injuries are commonly linked to glenohumeral joint instability, a frequent orthopedic condition. The glenohumeral joint is formed by the articulation of the glenoid cavity of the scapula (socket) with the head of the humerus (ball). Unlike the hip joint, which is deep and inherently stable, the glenoid fossa is shallow, providing a wide range of motion but rendering the joint intrinsically unstable. The labrum, a fibrocartilaginous ring, deepens the glenoid fossa and enhances joint stability. Glenohumeral joint instability refers to the inability to maintain the humeral head within the glenoid cavity during shoulder movement. It can manifest as anterior, posterior, or multidirectional instability (2).
The glenoid, or glenoid cavity, is a crucial anatomical structure in the scapula (shoulder blade). It is a shallow, cup-like depression on the lateral side of the scapula that forms an integral part of the shoulder joint, also known as the glenohumeral joint. The glenoid cavity articulates with the head of the humerus, allowing for the shoulder's extensive range of motion, essential for activities like lifting and throwing. To provide additional stability, the glenoid cavity is deepened by the glenoid labrum, a fibrocartilaginous structure that holds the humeral head in place. Injuries or biomechanical alterations involving the glenoid or humerus can significantly affect the shoulder joint's stability and function, resulting in pain, movement restrictions, and a heightened risk of future injuries. Restoring normal shoulder function in such cases often necessitates medical intervention and therapeutic rehabilitation (3).
2. Objectives
Anterior instability typically occurs when the humeral head is displaced anteriorly, often due to one of the following mechanisms: Traumatic dislocation (4), repetitive microtrauma, repetitive overhead activities or high stress on the shoulder joint, such as throwing a baseball, or congenital predisposition.
Patients with glenohumeral joint instability and anterior labrum injuries usually present with frequent shoulder dislocations, shoulder pain, a sensation of instability, and a limited range of motion. An injury to the labrum and associated glenohumeral capsule/ligaments is known as a "Bankart's lesion." Damage to these soft tissue-reinforcing structures is thought to increase the shoulder's vulnerability to recurrent dislocations. A fracture of the adjacent anterior inferior glenoid, typically occurring in conjunction with an anterior glenohumeral dislocation, is sometimes referred to as a "bony Bankart" (in contrast to "soft Bankart" or "fibrous Bankart") (5). Patients who have experienced multiple dislocations are more likely to develop ALPSA lesions, often resulting from chronic injury rather than acute dislocation. An ALPSA lesion refers to the separation of the anterior inferior labrum from the glenoid, with the periosteum and scapula remaining intact but significantly elevated (6). Treatment of ALPSA typically involves surgical repair to restore the labrum and ligaments to their proper positions and address any associated bone or soft tissue damage. Rehabilitation is often necessary following surgery to regain shoulder strength and stability.
Shoulder Perthes is an anterior glenohumeral injury that occurs when the anterior inferior labrum is torn and lifted off the glenoid edge but remains connected to the elevated periosteum of the anterior glenoid. Although the labrum may appear properly positioned, it no longer functionally stabilizes the humeral head due to the compromised stabilizing action of the inferior glenohumeral ligament (7).
The purpose of this study was to use MRI to determine the angles between the glenoid and the humerus, employing the techniques outlined by Friedman et al. and Poon and Ting (PT). Additionally, the data were compared between the two glenoid groups.
3. Methods
After obtaining approval from AJA University of Medical Sciences and informed consent from participants, a retrospective comparative cross-sectional study was conducted on patients aged 18 to 70 years with anterior labrum injuries and individuals without such injuries who underwent shoulder MRI imaging for reasons unrelated to labrum injuries. Individuals with a history of shoulder surgery, lack of MRI scans, moderate to severe glenohumeral degenerative changes, or multidirectional instability without labrum tears were excluded from the study. Informed consent was obtained from all participants, and they were assured of the confidentiality of their information and the absence of any additional or harmful procedures during the project.
To collect data, MRI imaging with a standard shoulder protocol was used to evaluate glenoid inclination and version angles in both groups. These angles were measured at the middle level of the glenoid in coronal and axial MRI sections using the Friedman method and the PT method. The confounding effects of age and gender were minimized using the caliper matching method. After data collection, glenoid inclination and version angles were compared between the two groups. Additionally, the relationship between anterior labrum injuries and glenoid anatomy was assessed, and the influence of demographic factors on the likelihood of such injuries was examined.
Quantitative variables were reported as means and standard deviations, while qualitative variables were presented as frequencies and percentages. The t-test and Mann-Whitney tests were used to compare quantitative and qualitative data and analyze differences between the injury and control groups.
4. Results
Fifty-five patients with anterior labrum injuries and 55 patients from the control group were studied. A paired chi-square test was used to evaluate gender distribution between the two groups. The gender distribution in the anterior labrum injury group included 17 women and 38 men, while the control group had 18 women and 37 men, showing no statistically significant difference (P = 0.838) (Table 1).
| Variables | Anterior Labrum Injury | Control Group | P-Value |
|---|---|---|---|
| Gender | 0.83 | ||
| Male | 38 (69.1) | 17 (30.9) | |
| Female | 37 (67.3) | 18 (32.7) | |
| Version | 0.001 | ||
| Anteversion | 15 (27.3) | 7 (12.7) | |
| Retroversion | 40 (72.7) | 48 (87.3) | |
| Inclination | 0.001 | ||
| Caudal | 33 (60) | 17 (30.9) | |
| Cranial | 22 (40) | 38 (69.1) |
a Values are expressed as No. (%).
The age distribution analysis showed that the median age in the anterior labrum injury group was 23 years, with an interquartile range (IQR) of 8 years. In the control group, the median age was 31 years, with an IQR of 9 years. Additionally, the mean age in the control group was significantly higher at 31.4 years (SD = 7) compared to 24.3 years (SD = 5.2) in the anterior labrum injury group (P < 0.005).
A comparison between the two groups in terms of version was conducted using an independent t-test. The version rate in the case group was significantly more toward anteversion, which was statistically significant (P < 0.001). Moreover, anteversion increased the odds (odds ratio) of anterior labrum injury by 2.6 times, though this result was not statistically significant (P = 0.062, OR = 2.57, 95% CI).
The comparison of inclination was conducted using an independent t-test. The degree of inclination in the case group was significantly more caudal compared to the control group (P < 0.001). Additionally, an increase in caudal inclination raised the odds of anterior labrum injury by 3.35, a statistically significant result (P = 0.035, OR = 3.35, 95% CI).
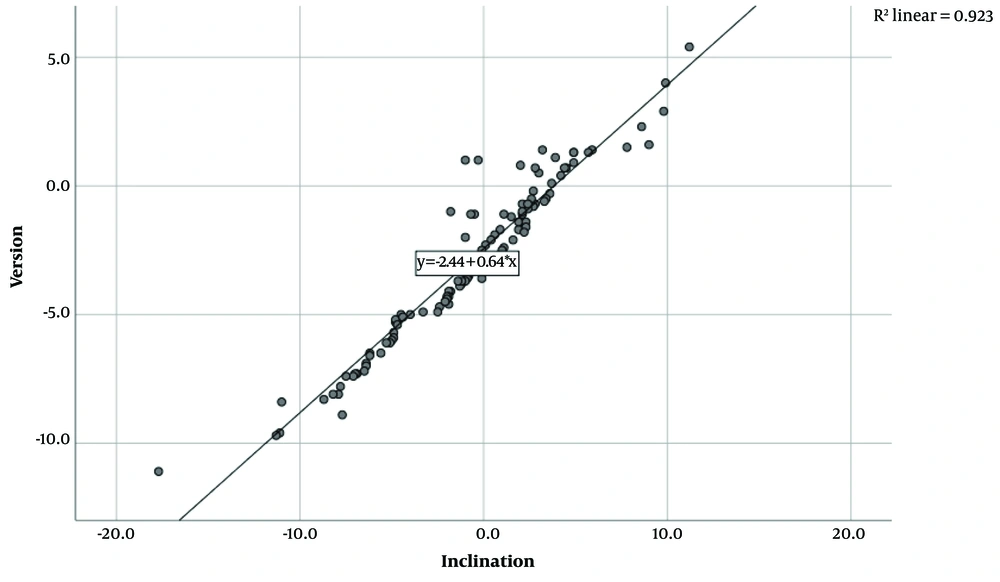
The relationship between inclination and version was assessed using linear regression analysis, and a significant association was found between these variables (P < 0.001, R = 0.961) (Figure 1).
Furthermore, the relative frequency of subtypes of anterior labrum injury in the case group was determined as follows: Thirty-three patients had bony Bankart injuries, accounting for 60% of cases; 12 patients had GLAD injuries, with a relative frequency of 21.8%; 4 patients had ALPSA injuries, comprising 7.3%; and 6 patients had Perthes injuries, with a relative frequency of 10.9%.
5. Discussion
Although there was no significant gender difference between the two groups in this study, the mean age of the control group was considerably higher than that of the anterior labrum injury group. In the anterior labrum injury group, the inclination was significantly more caudal compared to the control group, and the version was notably more toward anteversion. Additionally, a statistically significant increase of 3.35 in the likelihood of anterior labrum injury was associated with caudal inclination. While anteversion increased the odds of anterior labrum injury by 2.6 times, this difference was not statistically significant. Furthermore, the relationship between inclination and version was assessed using linear regression, which demonstrated a significant association.
Hohmann and Tetsworth investigated the relationship between anterior labrum injuries and glenoid version and inclination. Patients under 40 years old who underwent shoulder arthroscopies (study group) were compared with patients who had shoulder magnetic resonance imaging (MRI) for unrelated reasons (control group). Magnetic resonance imaging results from 130 patients in the control group (mean age 30.9 ± 7 years) and 128 patients in the study group (mean age 24.5 ± 8.6 years) with confirmed anterior traumatic shoulder dislocation were analyzed. In the study group, the mean inclination was 5.9 ± 1.6 degrees (inferior inclination), and the mean version was -1.7 ± 4.5 degrees (retroversion). In the control group, the mean inclination was -4 ± 6.8 degrees (superior inclination), and the mean retroversion was -5.8 ± 4.6 degrees. Significant differences in version and inclination were observed between the groups (P = 0.0001 and P = 0.0001, respectively).
The findings of their study clearly demonstrated that individuals with stabilized anterior instability of the shoulder had significantly greater glenoid version and inclination compared to the control group (8). These results align closely with the findings of our study.
The impact of the shoulder joint's morphological bone structure on anterior dislocation was examined by Kivrak and Ulusoy in 2023. The study included 80 patients, with 40 in the patient group and 40 in the control group. The glenoid width was measured at 25.61 ± 1.72 in the control group and 24.27 ± 1.58 in the patient group. The glenoid height was 36.49 ± 2.26 in the patient group and 36.74 ± 1.99 in the control group. The height-to-width ratio in the patient group was 1.5 ± 0.08, compared to 1.43 ± 0.05 in the control group. Glenoid version was -1.17 ± 0.53 in the patient group and -1.44 ± 1.1 in the control group. Glenoid inclination in the patient group was 3.93 ± 1.44, compared to 3.81 ± 2.64 in the control group. Glenoid depth was 1.69 ± 0.41 in the patient group and 2.12 ± 0.53 in the control group. Statistical analysis revealed significant variations in glenoid width (P < 0.001), glenoid height-to-width ratio (P < 0.001), glenoid version (P < 0.001), and glenoid cavity depth (P < 0.001). However, glenoid height and inclination were comparable between the groups (9). This study differed from ours in that it also assessed glenoid height, while the inclination remained comparable.
An investigation of the impact of anatomical degenerative variables of superior labrum lesions (SLAP) on rotator cuff tears was conducted by Virk et al. in 2017. The study included 421 middle-aged patients who underwent arthroscopic surgery to address rotator cuff injuries. The patients were divided into two groups based on the presence of superior labrum injuries (SLAP). The magnitude and angles of rotator cuff tears were examined in both groups, along with glenoid inclination, glenoid length, humeral head diameter, acromio-humeral distance (AHD), head-glenoid difference (HGD), and glenoid head angle (HGA). The study's findings demonstrated that an HGD greater than 10 mm could serve as an anatomical predictor of degenerative SLAP (1). HGD appears to raise the likelihood of anterior labrum injury, much like anteversion and caudal inclination, though this was not assessed in the current investigation.
A study by Funakoshi and Arciero in 2022 sought to determine the correlation between glenoid version and the degree of glenoid bone loss in individuals with a history of anterior shoulder dislocations. This retrospective case-control study included 72 individuals with recurrent unilateral anterior shoulder instability (ASI). Magnetic resonance arthrograms (MRAs) were analyzed, revealing that the occurrence of glenoid defects was almost five times more likely when retroversion exceeded 4 degrees. Additionally, the study demonstrated a strong correlation between the degree of glenoid bone loss and both the bone's version angle and the frequency of prior dislocations (2). A distinguishing feature of this study was the inclusion of the number of dislocations as a variable.
In a separate study by Burkhart et al. in 2020, the focus was on evaluating glenoid morphological factors, such as version, in cases with isolated anterior and posterior labrum tears exceeding 180 degrees. Parameters such as diameter ratio, glenoid version using the vault method, glenoid defect percentage, superior-inferior and anterior-posterior diameter, and other glenoid morphology criteria were assessed. Patients were divided into three groups: Those with anterior tears (group 1), posterior tears (group 2), and labrum tears greater than 180 degrees (group 3). Group 2 exhibited the greatest retroversion (19.9 ± 4.71 degrees), followed by group 3 (14.21 ± 4.59 degrees) and group 1 (11.24 ± 5.3 degrees), with statistically significant differences in glenoid version across all group comparisons. Group 3 had the least amount of glenoid bone loss, though the difference was not statistically significant. Furthermore, no statistically significant differences were observed for other measured metrics. Interobserver reliability for all measurements ranged from good to excellent (3). It appears that increasing the sample size in this trial could lead to more definitive conclusions.
Lippitt and Matsen the correlation between glenoid version and labral tears and unilateral instability. They categorized participants into three groups: The anterior instability or labrum tear group (33 individuals), the posterior instability or labrum tear group (34 individuals), and the stable controls group (n = 30). Using Friedman’s technique, the posterior pathology group (-9 degrees) demonstrated significantly greater retroversion compared to the anterior pathology group (-5 degrees) (P = 0.0104) and the control group (-4 degrees) (P = 0.0005). However, there was no statistically significant difference (P = 0.38) between the anterior pathology group and the control group (4). The smaller sample size of this study compared to the current one could explain the lack of significance in certain findings.
In 2023, Spiegl et al. assessed and compared glenoid version among patients with ASI, posterior shoulder instability (PSI), and a control group. The ASI group included 100 patients, the PSI group 65 patients, and the control group 100 patients. For the ASI group, the mean glenoid version values were -16 degrees for the vault version, -9.1 degrees for the simplified vault version, and -9.2 degrees for the chondrolabral version. The PSI group exhibited mean glenoid version values of -21 degrees, -13.4 degrees, and -16.6 degrees for the vault, simplified vault, and chondrolabral versions, respectively. The control group showed mean versions of -17.8, -9.5, and -9.8 degrees for the vault, simplified vault, and chondrolabral versions, respectively. The study revealed that the PSI group had significantly greater retroversion compared to the other two groups (P < 0.001). However, the degree of glenoid version in the ASI group was not significantly different from the control group (P = 0.009) (5).
As with any research, limitations exist. Future studies should incorporate larger sample sizes and assess additional factors such as glenoid height, HGD, and the frequency of dislocations to provide a more comprehensive analysis.
In conclusion, our study found that anteversion is a predisposing factor for injury, while caudal inclination significantly increased the ratio of anterior labrum injury. Furthermore, linear regression analysis confirmed a significant connection between inclination and version.