1. Introduction
Moyamoya disease (MMD) is a progressive cerebrovascular disorder characterized by the narrowing of the major blood vessels supplying the brain. This narrowing leads to the formation of abnormal blood vessels, known as collateral vessels, to compensate for the reduced blood flow (1). While MMD is most prevalent among Japanese individuals, it exhibits a global distribution with a wide range of clinical features and age at onset across different populations (2). The prevalence of MMD varies significantly across different regions, with East Asia reporting higher rates compared to other areas. Previous research in Japan has indicated a prevalence of 10.5 cases per 100,000 individuals and an incidence rate of 0.94 cases per 100,000 individuals (3).
The narrowing of vital cerebral blood vessels leads to the formation of aberrant collateral circulation at the brain stem (4). Females are diagnosed with the disease approximately 1.8 times more often than males, with the majority of diagnoses made during childhood (5). Research has demonstrated a significant association between MMD and a variety of factors, including atherosclerotic diseases, neurofibromatosis, rheumatologic diseases such as Sjögren's syndrome, infectious diseases like meningitis, and certain lifestyle behaviors such as smoking and cocaine abuse. Additionally, the use of medications that predispose individuals to thrombosis has been linked to an increased risk of developing MMD (6, 7).
The clinical spectrum of MMD encompasses both ischemic and hemorrhagic events. In children, progressive cerebral ischemia is the most common initial presentation, often manifesting as transient ischemic attacks or cerebral infarctions. Mental decline or seizures may also be early signs. Conversely, adults are more likely to experience intracranial hemorrhage as their first symptom, with ischemic symptoms occurring in approximately half of cases (8).
Current management of MMD primarily involves neuroprotective measures, revascularization procedures, and cognitive rehabilitation (9).
2. Case Presentation
A 43-year-old woman residing in the northwestern region of Iran (East Azerbaijan Province) with a 15-year history of ankylosing spondylitis, for which she has been receiving treatment, presented to Imam Reza Hospital with complete sensory and motor paralysis in her left hand while performing household chores. There was no history of smoking or cocaine abuse in the patient. According to the patient's husband, she has been experiencing intermittent blurred vision (with irregular intervals) for approximately 2 years. She sought medical attention at various hospitals in Tabriz and Tehran, where multiple sclerosis (MS) plaques were observed on MRI, leading to a diagnosis of MS and subsequent treatment. Blurred vision was the initial symptom of this disease (although the patient also complained of back pain, unrelated to vision and attributed to ankylosing spondylitis). The onset of blurred vision was associated with strenuous activities. According to the patient, MRI scans were performed at previous medical centers, but the documents are not currently available.
The patient was admitted to Imam Reza Hospital and was treated with aspirin, Plavix, sulfasalazine, and diclofenac. Upon admission, she experienced complete sensory and motor paralysis of the left hand. Sensory examinations (pain, temperature, position, vibration, two-point discrimination) were abnormal in the left hand. Muscle strength in the left hand was 0/5. Tendon reflexes were decreased. The patient demonstrated partial improvement in symptoms following initial treatments. Sensory symptoms fully recovered to pre-paralysis levels; however, motor symptoms did not fully recover. Specifically, strength in the left hand decreased from 5/5 (pre-symptoms) to 3/5 (post-paralysis and treatment) (Table 1) (10).
| Grade | Explanation |
|---|---|
| 0/5 | No contraction |
| 1/5 | Visible/palpable muscle contraction but no movement |
| 2/5 | The movement against gravity eliminated |
| 3/5 | The movement against gravity only |
| 4/5 | The movement against gravity with some resistance |
| 5/5 | The movement against gravity full resistance |
Necessary laboratory factors to investigate rheumatic diseases, including ANA, P-ANCA, RF, as well as thyroid function tests (TSH, free T4) and sickle cell anemia, were evaluated for the patient, and all were within the normal range. Following the initial presentation, the patient was admitted to the hospital for further evaluation and to determine the underlying cause of the recent symptoms. An MRI scan revealed MS plaques, and appropriate treatment was initiated.
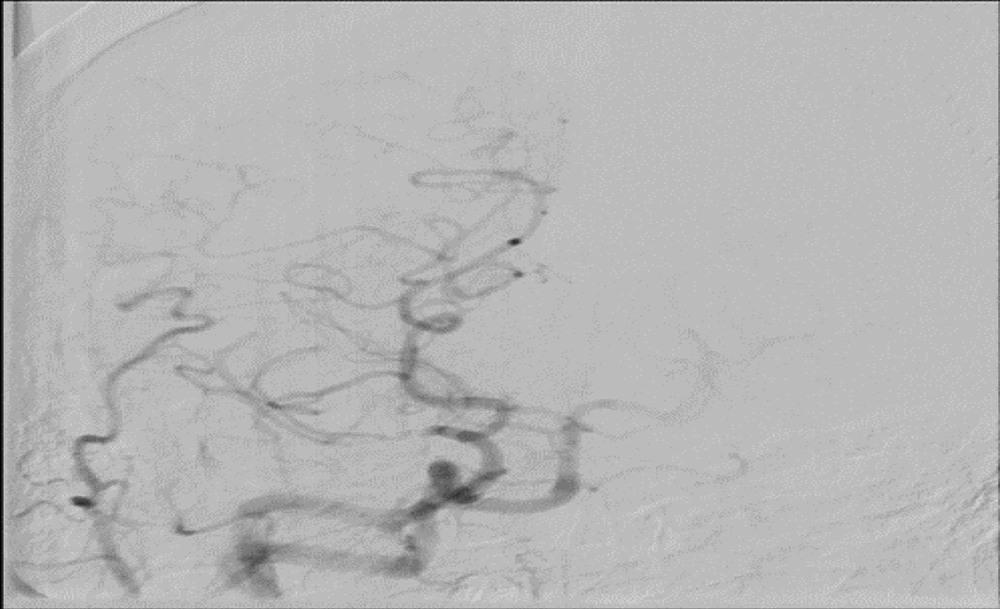
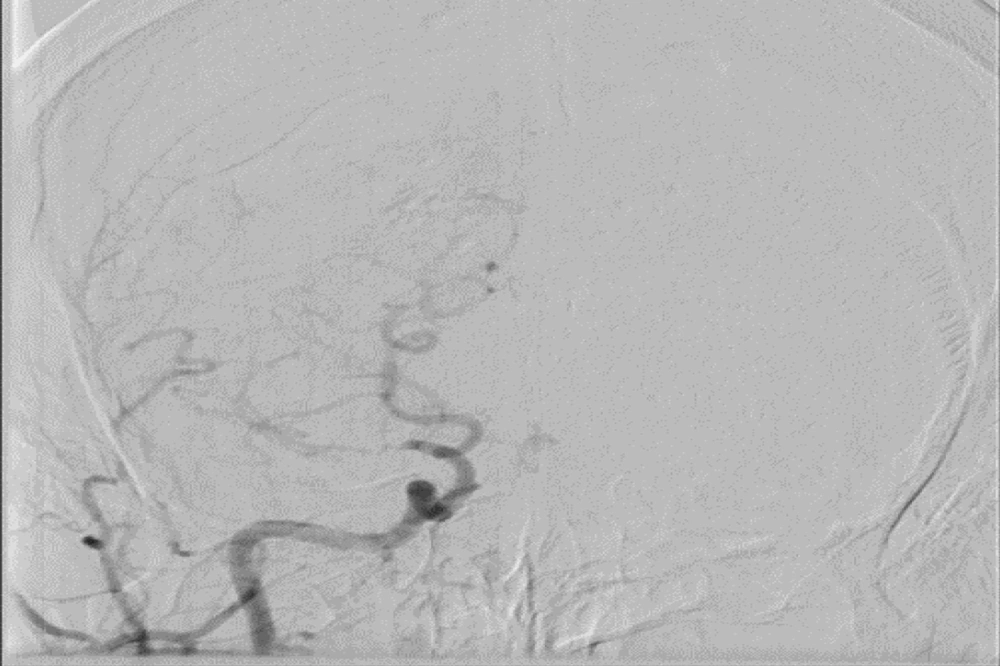
Approximately one week after admission, the patient was transferred to the intensive care unit (ICU) due to a worsening of the initial symptoms, including blurred vision and progressive weakness in the left hand. Vital signs were monitored frequently and remained within normal limits, but neurological symptoms did not show significant improvement. After two weeks of ICU monitoring and with no change in neurological status, cerebral angiography was performed (Figure 1 and 2).
Angiographic findings were as follows:
- The right middle cerebral artery demonstrated severe stenosis.
- The left middle cerebral artery also showed severe stenosis, which may be due to hypoplasia.
- The left vertebral artery had mild stenosis at its origin.
- The left anterior cerebral artery was narrowing.
- The right and left common carotid arteries, left and right internal and external carotid arteries, right anterior cerebral artery, and bilateral posterior cerebral arteries were normal.
- The cerebral venous system was reported as normal.
Recent cerebral angiography findings suggest a diagnosis of MMD in this patient. The patient's progressive clinical manifestations and lack of response to medical therapy can likely be attributed to this condition. Based on current evidence, the preferred treatment for MMD is surgical revascularization. Medical therapies are generally less effective than invasive procedures. Therefore, the patient was advised to undergo surgery. The patient has not yet undergone surgery due to financial constraints and the high cost of the procedure. The current medication regimen includes amantadine, clopidogrel, and aspirin. The patient continues to complain of blurred vision and decreased muscle strength in the left hand, with no significant improvement.
3. Discussion
Females are diagnosed with MMD approximately 1.8 times more often than males, with the majority of diagnoses made during childhood (5). Our patient's gender aligns with the higher prevalence of this disease in women, but in this case, the disease was diagnosed in the 5th decade of life, suggesting that elderly individuals with risk factors should also be screened for MMD.
Research has demonstrated a significant association between MMD and a variety of factors, including atherosclerotic diseases, neurofibromatosis, rheumatologic diseases such as Sjögren's syndrome, infectious diseases like meningitis, and certain lifestyle behaviors such as smoking and cocaine abuse. Additionally, the use of medications that predispose individuals to thrombosis has been linked to an increased risk of developing MMD (6, 7). The patient's rheumatological disease, ankylosing spondylitis, was the sole identified risk factor. Previous research has shown associations between certain rheumatologic diseases and other conditions, but the relationship between MMD and ankylosing spondylitis remains unexplored.
Given the potential implications for diagnosis and treatment, it is crucial to conduct further studies to investigate this possible connection. If there is a connection between these two diseases, MMD could be included in the differential diagnosis of patients with ankylosing spondylitis who develop neurological symptoms during their disease.
The clinical spectrum of MMD encompasses both ischemic and hemorrhagic events. In children, progressive cerebral ischemia is the most common initial presentation, often manifesting as transient ischemic attacks or cerebral infarctions. Mental decline or seizures may also be early signs. Conversely, adults are more likely to experience intracranial hemorrhage as their first symptom, with ischemic symptoms occurring in approximately half of cases (8). Our patient's symptoms began with blurred vision and progressed to complete sensory and motor loss in the left hand, consistent with an ischemic process. Neuroimaging studies did not identify any evidence of cerebral hemorrhage.
Current management of MMD primarily involves neuroprotective measures, revascularization procedures, and cognitive rehabilitation (9). Among the proposed treatment methods, surgical revascularization is currently considered the most effective and optimal treatment. The patient presented in our article, due to financial constraints and the high costs associated with the treatment, was unable to undergo this procedure. Annually, a significant number of patients are forced to discontinue their treatment due to financial difficulties. This case highlights the urgent need for governments and patient support organizations to establish financial assistance programs specifically for patients with rare diseases like MMD.
3.1. Conclusions
The differential diagnosis between MMD and MS can be challenging due to overlapping clinical and radiological features. MRI findings, in particular, can be misleading, as both diseases may exhibit inflammatory plaques. The MMD should always be considered, especially in MS patients who do not respond to treatment.