1. Background
The pleura, a serous membrane lining the lungs, mediastinum, diaphragm, and chest cavity, consists of two layers: The visceral pleura and the parietal pleura. A specific balance between hydrostatic and oncotic pressures in the visceral and parietal pleural arteries, along with effective lymphatic drainage, maintains the pleural space's normal low fluid content of 0.1 to 0.2 mL/kg of body weight (1, 2). Disturbance of this balance, through either excessive production or impaired absorption of pleural fluid, can lead to pleural effusion (PE). Pleural effusion is clinically significant, with nearly 1.5 million cases identified annually in the United States (3, 4). Clinically, pleural effusion typically presents with symptoms of dyspnea, cough, and chest pain, and patients often exhibit reduced breath sounds and dullness on percussion during physical examination (5).
To identify the underlying cause of PE, it is categorized into exudative pleural effusion (EPE) and transudative pleural effusion (TPE). Transudative pleural effusion arises from systemic factors that disrupt the pleural fluid balance without altering pleural surfaces or local capillaries. In contrast, EPE results from local factors affecting pleural surfaces, often necessitating more invasive diagnostic procedures, such as pleural biopsy or thoracoscopy (6, 7). To differentiate EPE from TPE, pleural fluid is aspirated, and the levels of protein or lactate dehydrogenase (LDH) in the pleural fluid and serum are analyzed. In 1972, Light and colleagues developed criteria that have since become the gold standard for differentiating exudative from transudative pleural effusions, demonstrating high sensitivity and specificity (8-10). Imaging methods such as chest X-ray and ultrasound can also aid in diagnosing PE (7, 11).
Given the clinical importance of accurately distinguishing between exudative and transudative pleural effusions, we designed and conducted a study to evaluate the diagnostic utility of computed tomography (CT) scan and ultrasound findings in determining the nature of pleural effusions. This study aims to enhance diagnostic accuracy and guide appropriate clinical management for patients with pleural effusion.
2. Objectives
This study aimed to evaluate the effectiveness of ultrasonography and CT scans in differentiating between exudative and transudative pleural effusions.
3. Methods
3.1. Study Design
The study protocol was approved under the supervision of the Iran University of Medical Sciences Research and Ethics Committee (code: IR.IUMS.FMD.REC.1402.176), and informed written consent was obtained from all subjects. In this cross-sectional study, 72 patients with pleural effusion were included and assessed. Data from patients with pleural effusion at Hazrat-e-Rasool General Hospital (Iran University of Medical Sciences, Tehran, Iran) between January 2021 and January 2022 were obtained. Demographic and clinical information was collected using a designated questionnaire, which included gender and age. Patients diagnosed with pleural effusion by an expert radiologist were deemed eligible for this study, regardless of their current disease status, whether inactive or active at the time of enrollment. Patients with malignancies, current infections, other autoimmune diseases, and endocrine diseases were excluded from the study.
For each patient, the levels of pleural fluid protein and serum were measured simultaneously based on Light's criteria to classify the type of pleural effusion as exudative or transudative. Based on these classifications, the predictive accuracy of CT scan and ultrasound in determining the nature of the pleural effusion relative to the final clinical diagnosis was evaluated.
3.2. Statistical Methods
For statistical analysis, chi-square and Kendall's coefficient of concordance (KCC) tests were utilized using SPSS version 24. A P-value of less than 0.05 was considered statistically significant.
4. Results
4.1. Participants and Descriptive Data
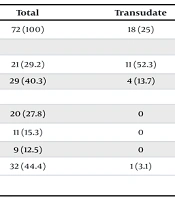
Seventy-two patients with a mean age of 56.1 ± 19.7 years (range: 17 - 93 years) were included in this study. Among these patients, 33 (45.8%) were female, and 39 (54.2%) were male. Eighteen patients (25%) had transudative pleural effusion, while 54 patients (75%) had exudative pleural effusion. Pulmonary edema was observed in 21 patients (29.2%). Additionally, evidence of parenchymal lung infection was present in 29 patients (40.3%). Pleural nodules were identified in 11 patients (15.3%), and pleural effusion loculation was noted in 20 patients (27.8%). Furthermore, 9 patients (12.5%) exhibited echogenic pleural fluid, and pleural thickening greater than one centimeter was observed in 32 patients (44.4%) (Table 1).
| Variables | Total | Transudate | Exudate | P-Value |
|---|---|---|---|---|
| Pleural fluid type | 72 (100) | 18 (25) | 54 (75) | 0.001 b |
| Pulmonary disorders | ||||
| Pulmonary edema | 21 (29.2) | 11 (52.3) | 10 (47.6) | 0.001 b |
| Lung parenchymal infection | 29 (40.3) | 4 (13.7) | 25 (86.2) | 0.071 |
| Pleural disorders | ||||
| Pleural effusion loculation | 20 (27.8) | 0 | 20 (100) | 0.002 b |
| Pleural nodules | 11 (15.3) | 0 | 11 (100) | 0.037 b |
| Echogenic pleural fluid | 9 (12.5) | 0 | 9 (100) | 0.64 |
| Pleural thickening > 1 cm | 32 (44.4) | 1 (3.1) | 31 (96.8) | 0.001 b |
Frequency of Pleural and Pulmonary Disorders by Pleural Fluid Type Among Study Participants a
4.2. Correlation Between Pleural Fluid Type and Pulmonary/Pleural Abnormalities
Significant correlations were found between the type of pleural fluid (transudate vs. exudate) and various pulmonary and pleural abnormalities, such as pulmonary edema, pleural nodules, pleural effusion loculation, and pleural thickening greater than one centimeter (P < 0.05). Transudative fluid was more commonly associated with pulmonary abnormalities, while exudative fluid was predominantly linked to pleural abnormalities (Table 1).
4.3. Computed Tomography Scan Findings
According to CT scan results, the most frequently observed abnormality was pleural thickening greater than one centimeter, present in 32 patients (44.4%). Statistical analysis revealed that all these abnormalities exhibited a non-normal distribution within the study population (P < 0.05) (Table 2).
| Pleural and Pulmonary Disorders | No. (%) | P-Value a |
|---|---|---|
| CT scan findings | ||
| Pulmonary edema | 21 (29.2) | 0.002 |
| Lung parenchymal infection | 29 (40.3) | 0.001 |
| Pleural nodules | 11 (15.3) | 0.003 |
| Pleural thickening > 1 cm | 32 (44.4) | 0.001 |
| Ultrasound findings | ||
| Pleural effusion loculation | 20 (27.8) | 0.001 |
| Echogenic pleural fluid | 9 (12.5) | 0.002 |
Computed Tomography Scan and Ultrasound Findings of Pleural and Pulmonary Disorders Among the Study Participants
4.4. Ultrasound Findings
Ultrasound revealed that pleural effusion loculation was the most common abnormality, observed in 20 patients (27.8%). Similar to the CT findings, all abnormalities detected via ultrasound exhibited a non-normal distribution in the study population (P < 0.05) (Table 2).
4.5. Concordance Between Ultrasound and Computed Tomography Scan
The concordance between ultrasound and CT scan findings was evaluated using KCC. The KCC values were interpreted as follows: Less than 0 indicating no concordance, 0 - 0.2 indicating slight concordance, 0.21 - 0.4 indicating fair concordance, 0.41 - 0.60 indicating moderate concordance, 0.61 - 0.80 indicating substantial concordance, and greater than 0.81 indicating almost perfect concordance. As presented in Table 3, ultrasound demonstrated fair concordance with CT scan in detecting pleural nodules (KCC = 0.33). However, for detecting pulmonary edema, parenchymal lung infection, pleural effusion location, and pleural thickening greater than one centimeter, ultrasound showed slight concordance with CT scan (KCC < 0.2). No concordance was found between ultrasound and CT scan findings in identifying echogenic pleural fluid (KCC < 0) (Table 3).
| Pleural and Pulmonary Disorders | Kendall's W (Concordance Coefficient) a | Level of Concordance |
|---|---|---|
| Pulmonary edema | 0.084 | Slight concordance |
| Lung parenchymal infection | 0.051 | Slight concordance |
| Pleural effusion loculation | 0.068 | Slight concordance |
| Pleural nodules | 0.333 | Fair concordance (slight to moderate) |
| Echogenic pleural fluid | 0.000 | No concordance |
| Pleural thickening > 1 cm | 0.103 | Slight concordance |
Concordance Between Ultrasound and Computed Tomography Scan Findings Using Kendall's Coefficient of Concordance
5. Discussion
Pleural effusions can develop under various pathological conditions. It is crucial to characterize the pleural effusion and identify its etiology. Light’s criteria are used as a first step to differentiate between EPE and TPE (6). Among the 72 patients studied, the majority (75%) had EPE, indicating a high prevalence of this type in our sample. This can be attributed to the high incidence of pulmonary infections and inflammatory-related diseases within the study population. The mean age of the patients was 56.1 ± 19.7 years, with a wide age range from 17 to 93 years, indicating a broad occurrence of pleural effusion across all age groups. The nearly equal gender distribution (45.8% women and 54.2% men) suggests that pleural effusion occurs similarly in men and women, consistent with the study by Mortazavi-Moghaddam et al. There appears to be no difference between age and gender in the incidence of pleural effusion (12).
The CT findings showed that the most common abnormality was pleural thickening greater than 1 cm, observed in 44.4% of patients. Similarly, ultrasonographic findings showed that pleural fluid loculation was the most common abnormality, present in 44.4% of patients. Imaging features such as pleural nodules (15.3%), localization of pleural fluid (27.8%), and pleural thickening (44.4%) suggest that these criteria can help accurately differentiate the types of effusion. There was mild to moderate agreement between ultrasound and CT in the detection of pleural nodules (KCC = 0.33), whereas agreement was poor for the detection of pulmonary edema, pulmonary parenchymal infection, localization of pleural fluid, and pleural thickening greater than 1 cm (KCC < 0). No significant agreement was observed between CT and ultrasonography in determining the echogenicity of pleural fluid (KCC < 0).
The results of this study are consistent with previous research. Bandaru and Rachegowda examined ultrasonography appearances and CT attenuation values in patients with pleural effusion and evaluated additional findings such as pleural thickening, pleural nodules, and localization. They reported that pleural thickening, nodules, and loculations were more common in exudates compared with transudates, with high specificity (91.6%, 95.8%, and 100%, respectively). It seems that changes such as increased pleural thickness, nodules, and loculations occur due to exudative pleural inflammation (13).
Recent studies have further validated the role of imaging techniques such as CT scans and ultrasonography in differentiating between exudative and transudative pleural effusions, aligning with the findings of our study. One study explored the diagnostic value of CT attenuation values to differentiate pleural effusion types, finding that exudative effusions typically show higher CT values compared to transudative ones. The study reported a median CT value of approximately 13.01 HU for exudates versus 4.89 HU for transudates, with a high correlation between CT values and protein levels in pleural fluid. This reinforces our observation that CT features like pleural thickening are associated with exudative effusions (14).
Additionally, a systematic review and meta-analysis compared ultrasonography to CT scans for pleural effusion quantification. The study concluded that while both modalities are effective, ultrasonography excels in bedside settings and provides specific patterns, such as septations or echogenicity, that strongly correlate with exudative effusions. This supports our finding of loculated pleural fluid being a common feature detected by ultrasound in exudative cases (15). Our findings for concordance in the detection of features such as pleural nodules are consistent with these studies, suggesting that while both imaging modalities are useful, their combined use may provide more comprehensive diagnostic insights. Overall, these recent studies confirm that the imaging criteria identified in our study are indeed valuable for the detection of pleural effusions. The high specificity of some of the features observed on CT and ultrasound emphasizes their complementary role in clinical practice (13-15).
Another study used radiological imaging techniques to assess pleural fluid and classified patients into two groups based on Light's criteria: TPF and EPF. They found that pleural thickening was more common in exudative than transudative fluid, which is consistent with our study (16). In addition, Yang et al. investigated the utility of ultrasound in determining the type of pleural effusion in 320 patients and differentiated transudate and exudate based on ultrasound findings. They found that some ultrasound patterns, such as complex or homogeneous isolated echogenic patterns, were always associated with exudate and that pleural nodules were a specific finding in malignant effusions (17).
Further research should focus on identifying specific imaging features on CT and ultrasound that allow better differentiation between exudative and transudative effusions. Additionally, standard protocols for image interpretation should be developed based on the unique characteristics of each type of effusion. These suggestions could lead to more accurate and efficient methods for the diagnosis and treatment of pleural effusion, ultimately improving patient outcomes.