1. Background
Headaches, also known as cephalgia, are a common and debilitating condition that can severely impact an individual's ability to perform everyday activities. There are various types of headaches, including migraine, tension-type headache, cluster headache, and frequent headaches. Globally, headaches affect approximately 40% of the population, with migraines alone accounting for 47% of the total burden (1, 2). As a highly prevalent condition, headaches affect over half of the global population, making them an important subject of research and management.
Migraine is a genetically influenced, complex primary headache disorder that typically presents with moderate to severe, often unilateral headaches, accompanied by symptoms such as nausea, vomiting, and sensitivity to light (photophobia) and sound (phonophobia). This condition is commonly underdiagnosed and is a major cause of disability and absenteeism from work (3). It affects around 30% of the global population, making it a significant health concern (4). Research indicates that women are more prone to migraines (20.7%) compared to men (9%). The prevalence of migraine is lower in Asia (10.1%) than in the United States (15.3%). In Iran, 6.9% of the population reported experiencing migraines, while in Pakistan, migraines account for 22.5% of all headaches, making it the second most common after tension headaches. Among the Pakistani population, the prevalence is higher in females (85.7%) than in males (14.3%) (5).
Numerous studies have attempted to identify factors that exacerbate migraines, though no definitive conclusions have been reached (6). Commonly recognized triggers include stress, insufficient sleep, fatigue, and exposure to bright sunlight, with menstruation being an additional trigger for women (7). Other factors, such as poor nutrition, fasting, and dehydration, which are often overlooked by sufferers, may also contribute to the onset of migraines (8). Weather conditions, particularly bright summer sunlight, have also been found to provoke migraines more than softer winter sunlight (9). Migraine patients often manage their symptoms through various remedies, including sleeping, taking hot showers, staying hydrated, consuming fatty foods, or using over-the-counter or prescribed pain medications (10).
Migraine is a prevalent condition that leads to significant morbidity and is linked to various systemic diseases, making it a key public health concern. Early recognition of migraines can facilitate prompt medical treatment and the implementation of personalized therapy, helping to prevent it from becoming a debilitating condition for individuals (11).
2. Objectives
The rationale of this study was to determine the prevalence of migraines among patients presenting with headaches at the neurology department of a tertiary care center. Additionally, identifying triggers will assist in understanding their relationship with migraine attacks and their frequency within the sample. This research is valuable as there is limited data on migraines in Pakistan, and it will help raise awareness and encourage further studies on the topic.
3. Methods
The present observational cross-sectional study was conducted at the Department of Neurology, Bahawal Victoria Hospital, Quaid-e-Azam Medical College, Bahawalpur, Pakistan, from September 2024 to December 2024, with the aim of determining the frequency of migraine among patients presenting with headaches. Migraine was defined according to the International Classification of Headache Disorders (ICHD-3) criteria (11). Patients with an altered state of consciousness, a history of fits or seizures, and diagnosed psychiatric illnesses were excluded from the study. Keeping a confidence interval of 95% and a 5% margin of error, a sample size of 235 was calculated using an expected frequency of migraine as 18.84% among patients presenting with headaches (12). However, the final sample size was 296.
After obtaining ethical approval and detailed informed consent, 296 patients presenting with headaches were included in the study using a non-probability consecutive sampling technique. Demographic information, including age and gender, was noted, and the patients were assessed for migraine. Information regarding its triggering factors and associated features was collected on a self-report basis. All data were recorded and entered into SPSS version 23 for analysis. Mean and standard deviation were calculated for numerical data, whereas percentage and frequency were generated for qualitative variables. The chi-square test was applied post-stratification, using a P-value of less than 0.05 as significant.
4. Results
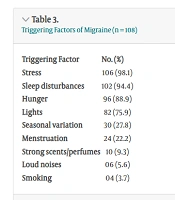
The mean age of the patients was 30.3 ± 13.7 years, with the majority of patients aged 25 years or above, as shown in Table 1. Among the participants, 186 (62.8%) were female. Migraine was present in 108 (36.5%) patients. Stratification of data revealed a statistical association of migraine with female gender (P-value = 0.013) but not with age (P-value = 0.614), as shown in Table 2. The most frequently reported triggering factors were stress (106, 98.1%) and sleep disturbances (102, 94.4%), as demonstrated in Table 3. Photophobia (94, 87.0%) and phonophobia (92, 85.2%) were the most commonly reported associated features of migraine, as depicted in Table 4.
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 186 (62.8) |
| Male | 110 (37.2) |
| Age (y) | |
| ≤ 24 | 112 (37.8) |
| ≥ 25 | 184 (62.2) |
| Migraine | |
| Present | 108 (36.5) |
| Absent | 188 (63.5) |
Clinical and Demographic Variables (n = 296)
| Triggering Factor | No. (%) |
|---|---|
| Stress | 106 (98.1) |
| Sleep disturbances | 102 (94.4) |
| Hunger | 96 (88.9) |
| Lights | 82 (75.9) |
| Seasonal variation | 30 (27.8) |
| Menstruation | 24 (22.2) |
| Strong scents/perfumes | 10 (9.3) |
| Loud noises | 6 (5.6) |
| Smoking | 4 (3.7) |
Triggering Factors of Migraine (n = 108)
| Associated Features | No. (%) |
|---|---|
| Photophobia | 94 (87.0) |
| Phono phobia | 92 (85.2) |
| Nausea | 74 (68.5) |
| Vomiting | 46 (42.6) |
| Lightheadedness | 26 (24.1) |
| Vertigo | 18 (16.7) |
Associated Features of Migraine (n = 108)
5. Discussion
In the present study, the prevalence of migraine was 36.5%, which is higher compared to previous studies that reported a prevalence of 9.1% in China, 12% in Australia, and 18.84% in Nepal (3, 12, 13). Recent studies from Pakistan have reported migraine prevalence rates of 28% and 39.8%, which align with the results of our study (8, 14). Our findings are consistent with data from the United States and Iran, which report similar prevalence rates of migraine (15, 16). However, studies from India have shown a higher prevalence of migraine in the general population (17). These variations in migraine prevalence across different regions may be due to factors such as geographic location, altitude, cultural differences, and the use of different assessment methods, which can influence the reported incidence rates globally (7, 18).
The results of this study provide valuable insights into the clinical and demographic characteristics, triggering factors, and associated features of migraines among the patient population. The majority of the patients were female (62.8%), with a significant association found between female gender and the presence of migraine (P-value = 0.013), confirming the well-established gender disparity in migraine prevalence. However, no significant association was found between age and migraine (P-value = 0.614), indicating that migraine occurrence in this sample was not age-dependent. This finding is consistent with other studies that have reported similar results (11, 15, 16).
Migraines are known to occur in about 60% of women during menstruation, primarily due to the drop in estrogen levels before menstrual bleeding, which results in a loss of serotonergic tone in the blood vessels (18). In our study, hormonal fluctuations were identified as a trigger in 22.2% of the migraine cases, which supports the theory that hormonal changes, particularly those related to the menstrual cycle, can trigger migraine attacks. This underscores the need to consider hormonal factors when managing migraines in female patients.
In terms of triggering factors, stress (98.1%) and sleep disturbances (94.4%) were the most commonly reported triggers in our study, highlighting the role of lifestyle factors in exacerbating migraine attacks. Other common triggers included hunger (88.9%) and bright lights (75.9%), while seasonal variation (27.8%) was also identified as a relevant trigger, particularly in females. Regarding associated features, photophobia (87.0%) and phonophobia (85.2%) were the most prevalent, aligning with the typical sensory disturbances observed in migraine sufferers. These findings underline the complex etiology of migraines, with both environmental and physiological factors playing a role in their onset and severity. This study contributes to the limited body of research on migraines in Pakistan, offering a foundation for future studies and raising awareness about the importance of early identification and management of migraine triggers.
The present study has certain limitations that should be considered. Being based in a single hospital, the findings may not be fully representative of the broader population, limiting the broader impact of the results. Therefore, it is important to conduct further studies with a larger and more diverse sample size to better understand the prevalence, triggers, and morbidity of migraines in the Pakistani population, and to assess the broader implications for migraine management and prevention strategies.
5.1. Conclusions
In conclusion, this study highlights a significant association between female gender and the prevalence of migraines, with more than one-third of the patients reporting migraines and a notable gender difference. However, age did not show a significant relationship with migraine occurrence. Stress and sleep disturbances were identified as the most common triggers, reported by nearly all participants, while photophobia and phonophobia were the most frequent associated symptoms. These findings suggest that managing stress and improving sleep quality may help in preventing migraines, and the gender-based differences observed could inform more targeted treatment strategies, particularly for female patients.