1. Context
Shoulder pain is the third leading cause of musculoskeletal pain, following back and neck pain (1), with a prevalence of 16% (range 0.67% to 55.2%) in the adult population (2). Common causes of shoulder pain include rotator cuff (RC) injuries, adhesive capsulitis, and hemiplegic shoulder pain (HSP) (3). Shoulder pain can significantly reduce the range of motion (ROM) of the shoulder, limit daily activities, and negatively impact overall quality of life (QOL) (4).
Rotator cuff injuries account for over 70% of shoulder pain cases. The pain and disability resulting from RC disease can severely limit individuals' ability to engage in daily activities and may even lead to work absenteeism (5). Frozen shoulder, also known as adhesive capsulitis, is another underlying cause of shoulder pain (6, 7). The condition involves inflammation within the rotator interval, leading to subsequent capsular fibrosis and stiffness. As a result, there is a progressive loss of glenohumeral motion, particularly in external rotation, accompanied by persistent shoulder pain (6).
Hemiplegic shoulder pain is a common occurrence following a stroke (8). Around 75% of hemiplegia patients report shoulder pain 12 months post-stroke (9). Improper positioning of the affected upper limb, laxity of the RC muscles, soft tissue damage, brachial neuropathy, and spasticity are all common causes of HSP (8, 10).
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive, safe, and cost-effective method commonly used in rehabilitation to manage musculoskeletal pain. Previous review studies have assessed the impact of TENS on conditions like RC injuries (11), adhesive capsulitis (6), and HSP (12, 13). However, the limited number of studies available prevented definitive conclusions regarding the efficacy of TENS.
2. Objectives
The objective of this systematic review and meta-analysis is to ascertain the efficacy of TENS in reducing shoulder pain and improving ROM among individuals suffering from shoulder pain.
3. Methods
This systematic review and meta-analysis followed the Cochrane Handbook guidelines and adhered to the PRISMA-P checklist for reporting systematic reviews and meta-analyses protocols (14). The study was also registered on PROSPERO with the registration ID CRD42021251600.
3.1. Search Strategy and Study Selection
We conducted an advanced search utilizing the population, intervention, comparison, outcome, and study design (PICOs) strategy (Appendix 1 in Supplementary File). Two independent researchers (M.B. and N.A.) performed searches in PubMed, Embase, Scopus, Web of Knowledge, Cochrane, and Google Scholar from their inception until March 2022. Additionally, we updated the search in PubMed on May 31, 2023. Following the removal of duplicate articles, two researchers (N.A. and S.H.) independently assessed the titles and abstracts of the studies based on the predetermined inclusion and exclusion criteria.
3.2. Eligibility Criteria
3.2.1. Participant
Studies whose participants were adults (18 years or older) with shoulder pain were included. Shoulder pain was categorized into RC injuries, adhesive capsulitis, and HSP. Studies that did not specify the cause of shoulder pain were included in the mixed diagnoses group (population not clearly defined) (3).
3.2.2. Intervention
All studies utilizing TENS, irrespective of the type (conventional, acupuncture-like, or burst mode), were included.
3.2.3. Comparison
The control group was divided into four categories: Sham TENS, no treatment, routine care, and active interventions (15). Routine care consisted of heat pack and exercise therapy. Active interventions were categorized into other electrical stimulation, injections, and other modalities such as extracorporeal shockwave therapy and Kinesio taping.
3.2.4. Outcomes
The outcomes assessed in this study were pain levels and ROM of the shoulder.
3.2.5. Studies
To ensure the validity of the findings, only randomized controlled trials (RCTs) with either a parallel design or a cross-over study design (with sufficient washout time) were included in this analysis.
3.3. Exclusion Criteria
Studies in which TENS was not the primary intervention, those that used TENS combined with other electrical therapy, and those where data were collected during TENS application (TENS on) were excluded from the analysis. Furthermore, case reports and case series, retrospective studies, review articles, summaries of studies presented at conferences, studies without accessible full texts, and unpublished or duplicate articles were also excluded.
3.4. Data Extraction
The data extraction process involved creating an MS Excel file using version 2010. Two independent authors (S.H. and T.A.) performed the data extraction. Articles for which the full text was not obtained were not included in the meta-analysis.
3.5. Quality and Risk of Bias Assessment
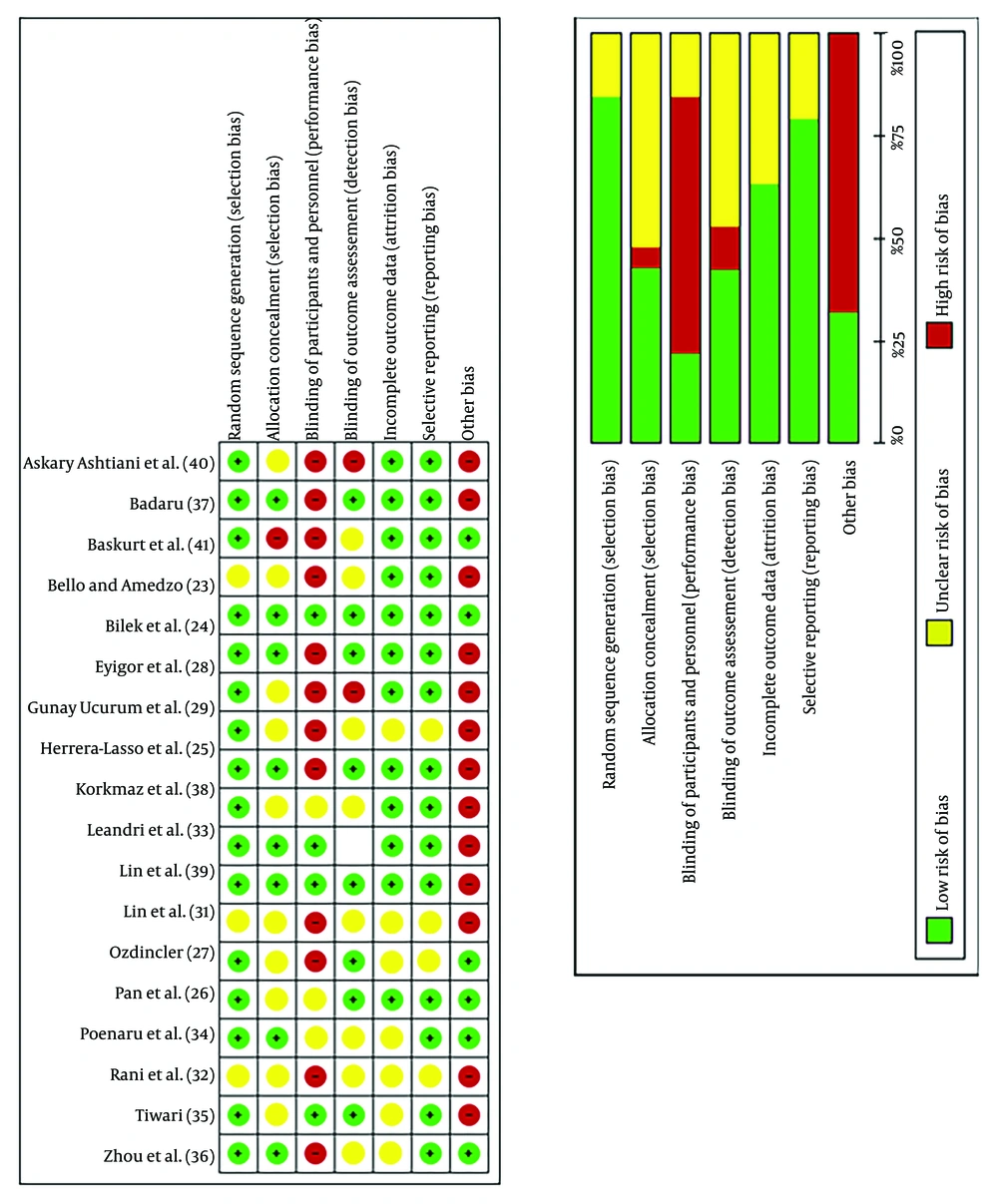
Risk of bias (ROB) was assessed using the Cochrane ROB tool (16). Two independent authors (L.J. and B.F.) evaluated the ROB for each included study. The items assessed included random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other sources of bias (e.g., sample size less than 30). Each item was categorized as low risk, high risk, or unclear. The overall certainty of the evidence was evaluated by two independent authors using the grades of recommendation, assessment, development, and evaluation (GRADE) tool (17) (https://gdt.gradepro.org) (Appendix 2 in Supplementary File).
3.6. Statistical Analysis
We utilized RevMan software version 5.4.1 (RevMan 2020) and STATA software version 17 for our analysis. To assess heterogeneity between studies, we employed the I² statistic with a cutoff point of ≥ 50%. Significant heterogeneity was defined as a P-value < 0.10 on the χ² test (18). The standardized mean difference (SMD) with a 95% confidence interval was used to analyze continuous outcomes when studies employed the same variables but with different scales. Standardized mean difference values between 0.2 and 0.5 are considered small, between 0.5 and 0.8 are medium, and greater than 0.8 are large (19). Additional meta-analysis information is provided in Appendix 3 in Supplementary File.
3.6.1. Subgroup Analysis
Subgroup analysis was conducted based on the duration of follow-up, categorized as immediate (less than a week) and long-term (more than eight weeks).
3.6.2. Sensitivity Analysis
Sensitivity analyses were conducted to assess the impact of excluding studies with a high ROB, including performance bias, detection bias, allocation concealment bias, and other biases (e.g., sample size < 30). Additionally, a leave-one-out analysis, known as jackknife analysis, was performed to evaluate its influence on the summary estimate (20).
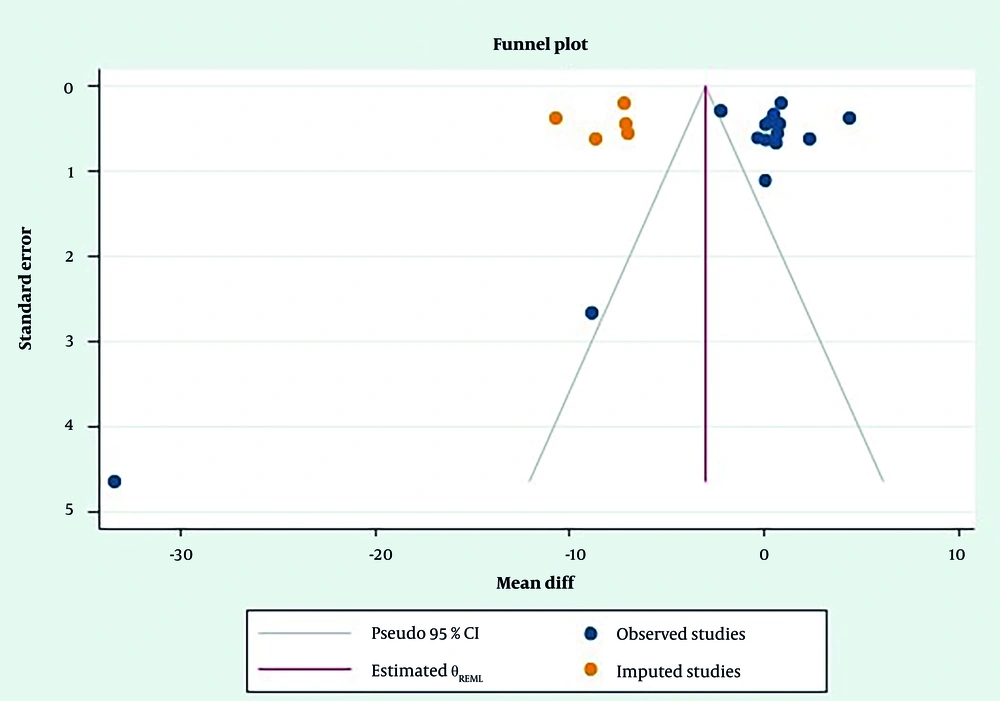
3.6.3. Assessment of Publication Bias
If the meta-analysis included more than 10 studies, a funnel plot was utilized to assess the presence of publication bias. In cases where asymmetry was detected, the "Trim-and-Fill" method was employed to adjust for any missing studies (21). To identify small study bias for continuous outcomes, Egger's test was conducted (22).
4. Results
4.1. Identification of Studies
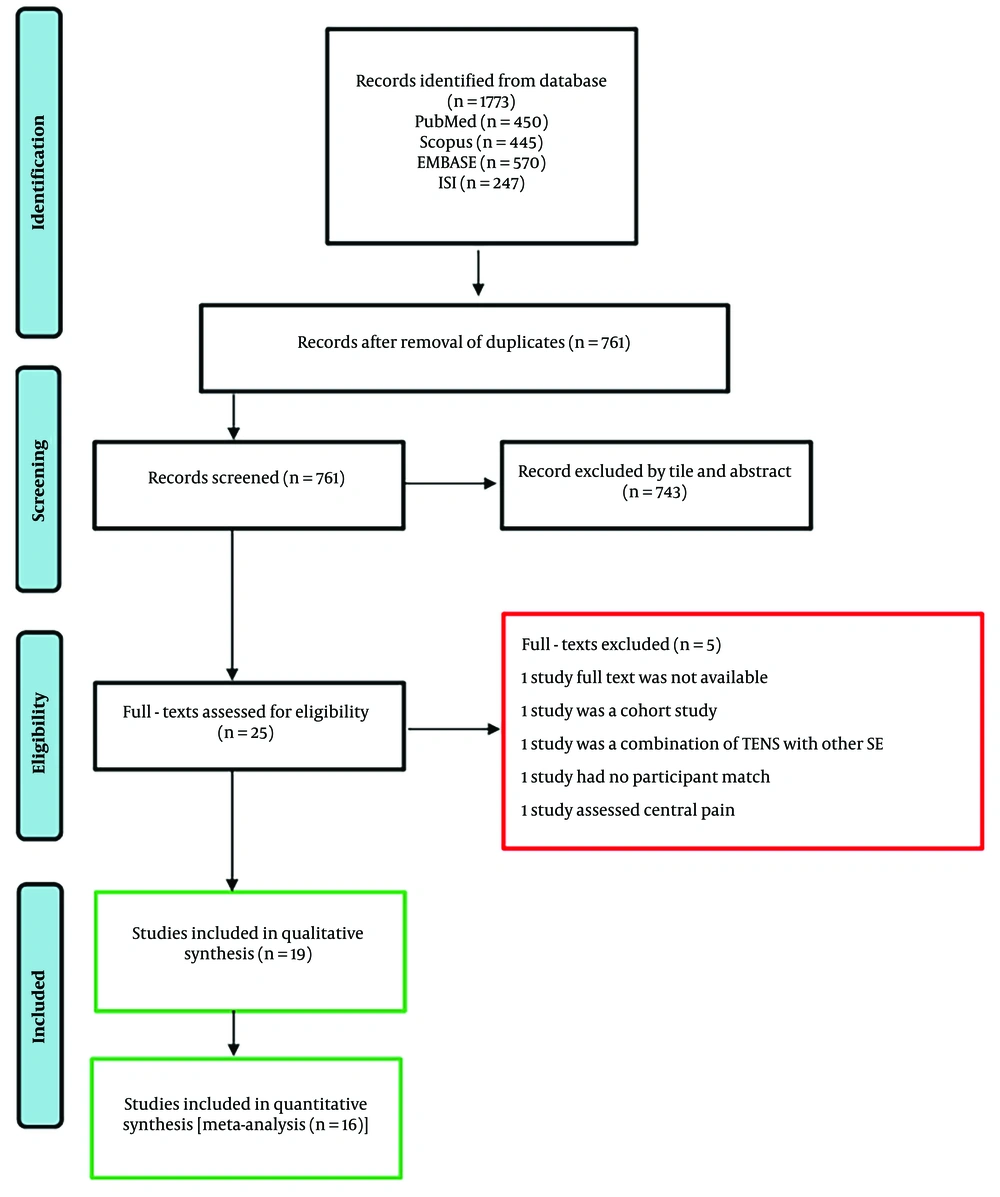
Figure 1 depicts the procedure for research selection. A total of 761 articles were identified from the initial search. After evaluating 25 articles for full-text eligibility, 19 articles were included in the qualitative review, and ultimately, 16 of these were included in the meta-analysis.
4.2. Overview of the Included Studies
The sample sizes ranged from nine (23) to 106 individuals (24), with a total of 1,220 people with shoulder pain examined, of which 519 were in the TENS group and 701 were in the control group. In eight studies, participants suffered from shoulder pain due to RC injuries (25-32); in six studies, they had shoulder pain after a stroke (23, 33-37); and in five studies, the cause of shoulder pain was unknown (24, 27, 38-40). The follow-up duration for patients varied from one day (24, 25, 41) to three months (29, 30) (Table 1).
| Number | Study (Year) | Study Type | TENS Group (N/F%) | Control Group (N/F%) | Disease | Combination Therapy | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | Leandri et al., 1990 (33) | RCT | High-Intensity Conventional TENS (20/75%), low-intensity conventional TENS (20/70%) | Placebo (20/75%) | Stroke | Exercise | Passive ROM |
| 2 | Herrera-Lasso et al., 1993 (25) | RCT | TENS (15/93%) | Ultrasound (14/64%) | RC disease | Infra-red heat, Codman exercise | VAS; ROM |
| 3 | Pan et al., 2003 (26) | RCT | Conventional TENS (28/68%) | Extracorporeal shock wave therapy (32/62.5%) | Calcific of RC tendinitis | - | Constant score; VAS; manual muscle test; changes of sonographic size and shape of calcium deposits |
| 4 | Ozdincler, 2005 (27) | RCT | Conventional TENS (15) | Low energy laser therapy (LEL) (15) LEL+TENS (15) | Shoulder pain | Therapeutic exercise | VAS; ROM; Constant Shoulder Index |
| 5 | Baskurt et al., 2006 (41) | RCT | Conventional TENS (30/66%) | Heat (31/70%) heat + TENS (31/58%) | RC disease | - | VAS; PPT |
| 6 | Poenaru et al., 2008 (34) | RCT | Conventional TENS (31/36%) | Galvanic application (33/42%) | Stroke | Physiotherapy | Barthel Index Activities of Daily Living Scale (ADL); VAS; action research arm test; Motricity Index; Constant Murley Scale |
| 7 | Bello and Amedzo, 2010 (23) | RCT | Conventional TENS (10/70%) | Hot pack (9/66.7%) | Stroke | Massage, passive and active mobilization of the shoulder joint | Brief Pain Inventory Short Form Question -12 (BPI SF-12) ARAT |
| 8 | Eyigor et al., 2010 (28) | RCT | Conventional TENS (20/70%) | Injection (20/75%) | RC disease | Exercise | VAS; active/passive ROM; SF36; Shoulder Pain and Shoulder Disability Questionnaire; BDI consumption |
| 9 | Korkmaz et al., 2010 (38) | RCT | Conventional TENS (20/70%) | Pulse radiofrequency (20/70%) | Shoulder pain | Exercise | VAS; active/passive ROM; SF36 Shoulder Pain and Shoulder Disability Questionnaire |
| 10 | Lin et al., 2015 (39) | RCT | Acupuncture; like TENS (50/65%) | Transcutaneous pulse radiofrequency (50/87.5%) | Shoulder pain | - | VAS; blood test |
| 11 | Askary Ashtiani et al., 2016 (40) | RCT | Burst mode TENS; (16) | Active potential stimulation (16) | Shoulder pain | - | America surgeons standardize shoulder; assessment form western ontario RC Index shoulder dyskinesia |
| 12 | Tiwari, 2018 (35) | RCT | Acupuncture; like TENS (15) | Tapping (15) | Stroke | Therapeutic exercises | VAS |
| 13 | Gunay Ucurum et al., 2018 (29) | RCT | Conventional TENS (20/75%) | Hot pack+ exercise (20/90%) interferential current (22/70%) ultrasound (21/89.5%) | RC disease | Hot pack + exercise | VAS; DASH SF36 |
| 14 | Zhou et al., 2018 (36) | RCT | Conventional TENS (32/19%) | Neuromuscular electrical stimulation (31/33%) Conventional rehabilitation program (18/16%) | Stroke | Routine rehabilitation | NRS active/passive ROM; fugl-meyer Assessment; modified Ashworth Scale; Barthel Index; Stroke-Specific Quality of Life Scale |
| 15 | Vrouva et al., 2019 (30) | RCT | Conventional TENS (21/62%) | MENS (21/42%) | RC disease | Kinesio-therapy | Shoulder Pain and Disability Index; NRS EuroQoL-5 Questionnaire Ultrasonography |
| 16 | Lin et al., 2019 (31) | RCT | Conventional TENS (25/40%) | TENS + RF (20/24%) | RC disease | Exercise | Comfortable level; adverse event; constant-murley shoulder scores; pain, enjoyment of life, and general activity scores |
| 17 | Badaru et al., 2020 (37) | RCT | TENS (25/44%) | Massage (25/40%) | Stroke | - | VAS |
| 18 | Rani et al., 2020 (32) | RCT | Conventional TENS (35/54%) | Standard treatment (35/54%) | RC disease | ROM exercises | Shoulder Pain and Disability Index |
| 19 | Bilek et al., 2021 (24) | Cross-over RCT | Conventional TENS (106) | HVPS (106); Placebo (106) | Sub acromial pain syndrome | - | VAS; Active ROM |
Abbreviations: PPT, pressure pain threshold; ARAT, action research arm test; BDI, Beck Depression Inventory; MENS, micro-current electrical nerve stimulation; HVPS, high voltage pulsed currents; RCT, randomized controlled trial; TENS, transcutaneous electrical nerve stimulation; RC, rotator cuff.
In two studies, acupuncture-like TENS was used (35, 39); in one study, burst mode TENS was used (40); and in the other studies, conventional TENS was used (23-38, 41). Six trials utilized only TENS (24, 26, 37, 39-41), while others combined it with other therapies such as exercise, hot packs, and massage (23, 25, 27-36, 38). The duration of TENS usage varied from 15 minutes (31, 39, 42) to 60 minutes (36) per day, with the number of treatment sessions ranging from one (24, 25, 41) to 30 (35) (Appendix 4 in Supplementary File).
4.3. Quality Assessment
Figure 2 displays the results of the quality assessment. Only Bilek et al. demonstrated no ROB, with a low risk in all items of the Cochrane Collaboration tool (24).
4.4. Outcomes
4.4.1. Immediate Effect of Transcutaneous Electrical Nerve Stimulation on Pain
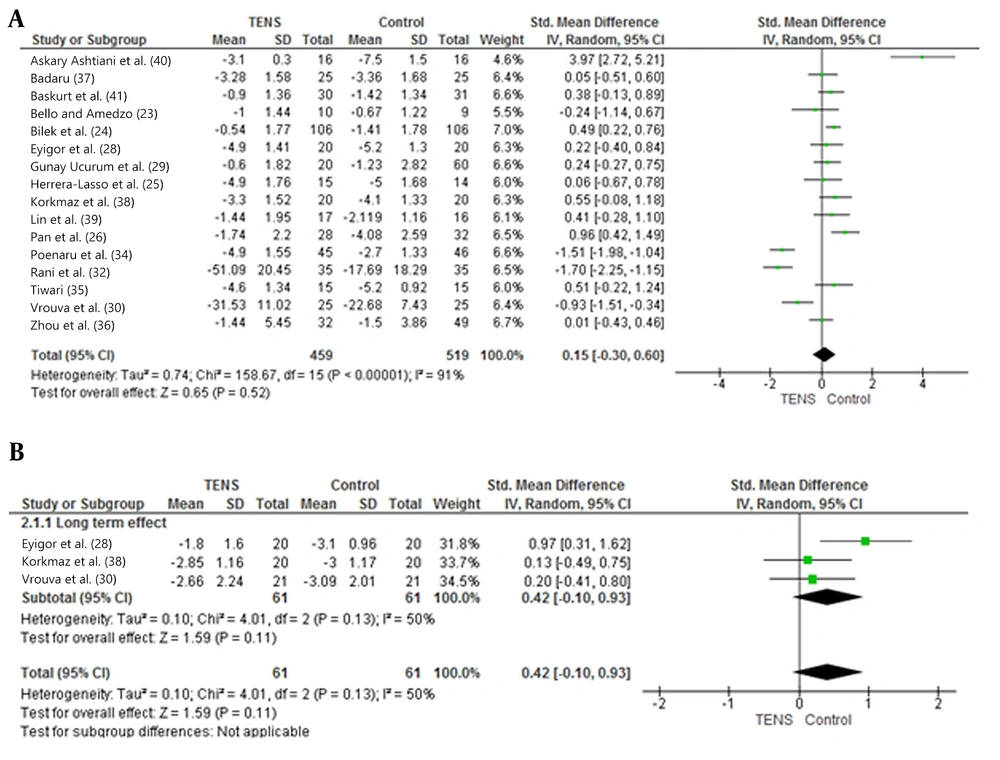
There was no significant difference in pain relief between the TENS group and the control group (SMD: 0.15; 95% CI: -0.30 to 0.59; I2: 91%; P = 0.52) (Figure 3A). It is crucial to emphasize that the certainty of the evidence was evaluated as very low. We downgraded the quality of evidence by one level due to inconsistency and evidence of publication bias. Furthermore, we downgraded the quality by two levels because of the ROB and indirectness (Appendix 5 in Supplementary File).
4.4.2. Long-term Effect of Transcutaneous Electrical Nerve Stimulation on Pain
Only three studies with 122 participants had a follow-up period of more than eight weeks (28, 30, 38). There was no significant difference in pain relief between the TENS group and the control group (SMD: 0.15; 95% CI: -0.30 to 0.59; I2: 91%; P = 0.52) (Figure 3B). The certainty of the evidence for these findings was assessed as very low. We downgraded the quality of evidence by one level due to the ROB, imprecision, and indirectness (Appendix 5 in Supplementary File).
4.4.3. Effect of Transcutaneous Electrical Nerve Stimulation on Active and Passive Range of Motion
Based on the results of five trials (24, 25, 28, 36, 38), it was found that the use of TENS did not result in a significant improvement in active abduction compared to control groups (SMD: -3.72; 95% CI: -8.78 to 1.34; I²: 0%; P = 0.15). Similarly, there was no significant difference in active flexion (SMD: -0.05; 95% CI: -0.23 to 0.13; I2: 0%; P = 0.61), external rotation (SMD: -0.03; 95% CI: -0.18 to 0.13; I2: 0%; P = 0.75), and internal rotation improvement between the TENS and the control group (SMD: -0.26; 95% CI: -0.05 to 0.58; I²: 0%; P = 0.10) (Appendix 6 in Supplementary File). The certainty of the evidence was assessed as very low, as the evidence was downgraded for ROB, indirectness, and imprecision (Appendix 7 in Supplementary File).
Passive abduction (SMD: -0.11; 95% CI: -0.45 to 0.24; I2: 47%; P = 0.54), flexion (SMD: -0.05; 95% CI: -0.29 to 0.18; I2: 0%; P = 0.67), external rotation (SMD: -0.09; 95% CI: -0.42 to 0.24; I2: 46%; P = 0.60), and internal rotation (SMD: -0.04; 95% CI: -0.27 to 0.35; I2: 0%; P = 0.79) improvement from TENS was non-significant compared to the control group (Appendix 8 in Supplementary File). The certainty of the evidence was assessed as very low, as the evidence was downgraded for ROB, indirectness, and imprecision (Appendix 7 in Supplementary File).
4.5. Sensitivity Analysis
We conducted a leave-one-out sensitivity analysis to assess the influence of individual studies on the overall result of TENS versus the control group on shoulder pain immediately (Appendix 9 in Supplementary File). The analysis revealed that none of the included studies significantly impacted the SMD value for this outcome. However, a sensitivity analysis was conducted based on the ROB (Appendix 10 in Supplementary File).
4.6. Assessment of Publication Bias
Egger's test showed no small study effect in the meta-analysis (P = 0.89). Funnel plot asymmetry was observed, and Trim-and-Fill analysis indicated that five studies were missing on the left side (Figure 4).
5. Discussion
The findings of this systematic review and meta-analysis revealed that TENS therapy did not significantly reduce shoulder pain when compared to control groups, both immediately and for more than eight weeks after the last treatment session. However, high statistical heterogeneity was observed based on the I² test. The effect of TENS on the active and passive shoulder range of motion was not greater than that of the control group. The certainty of evidence was low and very low due to the high ROB and high heterogeneity of studies.
Limited review studies have examined the effects of TENS on reducing shoulder pain (11-13, 42). Lee et al.'s study in 2017 (12) showed that electrical stimulation had no significant effect on the function and reduction of shoulder pain in people with stroke. In Desmeules et al.'s (11) review study that examined the effect of TENS on RC disease, only six studies were included. These studies were not meta-analyzed due to the high ROB, and the effect of TENS on pain reduction was not proven. A review of studies that examined the effect of TENS on reducing musculoskeletal pain reached similar results (43-45). The study by Martimbianco et al. (44), which examined the effect of TENS on chronic neck pain, and the study by Wu et al. (45), which examined the effect of TENS on reducing chronic back pain, showed that TENS does not significantly reduce pain compared to the control group.
Johnson et al.'s study in 2022 (15) showed that TENS significantly reduced acute and chronic pain when compared to sham. In the current review, only one study compared TENS with sham (24), whereas one study compared TENS with a group that did not receive any intervention (29). Four studies compared TENS with routine treatments (23, 32, 36, 41), and among those that compared TENS with active interventions, one study showed that TENS was more effective than injections in reducing pain (28). Eight studies compared TENS with other electrical stimulation and found no significant difference between the two groups (24, 29, 30, 34, 36, 38-40). However, five studies that compared TENS with other interventions such as ESWT (26), ultrasound (25, 29), massage (37), or taping (35) showed significant differences in pain reduction in the control group compared to TENS.
A network meta-analysis study conducted in 2021 revealed that ultrasound, laser, and acupuncture were more effective than TENS in reducing subacromial pain in short-term follow-ups (2 - 6 weeks) (42).
It is important to consider the results of studies that have used TENS in combination with exercises. According to the 2018 clinical practice guidelines (CPG) of the American College of Occupational and Environmental Medicine, adding TENS as an adjunctive intervention to an exercise program is recommended (46). Steuri et al. (47) demonstrated that combining therapeutic interventions with conservative exercises enhances their efficacy in reducing pain caused by shoulder impingement. Similarly, Wu et al. (48) found that TENS, when used in combination with other interventions, significantly reduces pain in knee osteoarthritis compared to the control group.
Two studies have examined the impact of single-session TENS on pain reduction (24, 41), and they found that the control group had a moderate effect in reducing pain compared to TENS. However, as the number of sessions increases, the effectiveness of TENS also increases, and there is no significant difference between the two groups. A systematic review and meta-analysis conducted by Amer-Cuenca et al. in 2023 (49) revealed that using TENS repeatedly (ten sessions or more) resulted in significant pain reduction in fibromyalgia.
Studies examining the effect of TENS on increasing joint range of motion are limited. In this review study, only five studies (24, 28, 33, 36, 38) evaluated the effect of TENS on shoulder joint ROM and revealed that TENS did not show any significant improvement in the active and passive range of motion compared to the control group. Wolf et al. (50) conducted a review study to investigate the effect of TENS on trunk range of motion in patients with chronic back pain. The study revealed that trunk flexion and extension increased in the exercise group compared to the TENS group, and this improvement remained for more than a month. However, in studies that compared TENS with exercises to exercises alone, the range of motion of flexion increased in the TENS group.
5.1. Conclusions
This systematic review and meta-analysis showed that the use of TENS reduces shoulder pain and increases the range of motion of the shoulder joint immediately and at least eight weeks after use, comparable to the control group. This review provides only low-quality evidence; we suggest that at least 15 sessions of TENS combined with exercise can effectively reduce chronic shoulder pain. To obtain more reliable and conclusive results, high-quality RCTs with larger sample sizes and longer follow-ups should be conducted to investigate the effectiveness of TENS on pain and ROM in individuals with shoulder pain of different etiologies.