1. Background
Effective cardiopulmonary resuscitation (CPR) is a cornerstone of cardiac arrest intervention (1). Traditional central pulse assessment has limitations, particularly in the early stages (2). Pulseless electrical activity can render continued conventional CPR futile, requiring more accurate assessment methods (3). While end-tidal CO₂ monitoring is available, its use is inconsistent. Echocardiography and Doppler ultrasound provide enhanced, real-time cardiac function assessment during CPR, facilitating better decisions on resuscitation termination (4). Nonetheless, accurate identification of successful resuscitation and optimal termination time remains a challenge. Be'sat Nahaja Hospital, the site of this study, frequently encounters a surge of critically ill patients requiring CPR within its emergency department. The inherent constraints of time, limited medication availability, and facility resources can impede efficient patient prioritization. Therefore, this study endeavors to develop a scientifically rigorous methodology for CPR assessment utilizing femoral artery color Doppler ultrasound and echocardiography. The data derived from these techniques are intended to provide objective, quantifiable measures of hemodynamic response, potentially serving as a valuable legal record of CPR procedures conducted.
1.2. Literature Review
Cardiac arrest severely reduces cardiac output, depriving vital organs of oxygen (5). The brain is highly vulnerable; loss of cerebral blood flow depletes ATP, and anaerobic metabolism leads to neuronal death (6). Other organs, including the heart, kidneys, and lungs, are also affected. Electrical disturbances, such as ventricular fibrillation, disrupt cardiac output (7, 8). The CPR aims to sustain blood flow and oxygen delivery until interventions like defibrillation can restore return of spontaneous circulation (ROSC) (9). Hemodynamic assessment is crucial for optimizing blood flow during resuscitation (10).
Traditional methods like pulse checks are unreliable early in CPR. Arterial blood pressure and central venous pressure monitoring also have limitations (11, 12). Perfusion indices offer insights into tissue oxygenation (13), but pulse oximetry can be affected by lung disease. These limitations necessitate comprehensive, real-time assessment tools like Doppler ultrasound and echocardiography. Effective CPR requires a balance between chest compressions and organ perfusion. Manual pulse palpation is unreliable and interrupts compressions (14, 15).
Doppler ultrasound offers non-invasive blood flow measurement, and educational interventions can improve pulse check efficiency (16, 17). Doppler ultrasound is more accurate than palpation and enables dynamic evaluation of CPR effectiveness. Integrating Doppler ultrasound requires careful evaluation to minimize compression disruptions. Research should aim to balance accurate pulse assessment with uninterrupted compressions (18).
2. Methods
This one-year descriptive study evaluated CPR effectiveness in adult patients requiring CPR in the emergency department. The study population comprised adults experiencing cardiac arrest, clinically presenting as pulselessness and apnea, and requiring CPR. All adults admitted to the Be'sat Nahaja Hospital Emergency Department requiring CPR constituted the sampling frame. Participants were selected using random sampling. The study was conducted in the Be'sat Nahaja Hospital Emergency Department, chosen for its high volume of cardiac arrest cases and standardized CPR protocols. This study was approved under the ethical approval code IR.AJAUMS.REC.1403.028.
Data collection during resuscitation included continuous physiological monitoring of vital signs, color Doppler ultrasound of femoral artery blood flow, and electronic medical record review. Specialists were available for each step. Color Doppler sonography and echocardiography were positioned to avoid interference with CPR. Statistical analysis, using repeated measures two-way ANOVA, assessed the effectiveness of color Doppler ultrasound and its association with outcomes.
The results indicated a statistically significant difference (P < 0.05), confirming the validity and meaningfulness of the collected data. Physiological variables included heart rate (bpm), vascular blood flow (Doppler ultrasound), peak systolic velocity (PSV, cm/s), and ejection fraction (EF, %).
3. Results
3.1. Patient Demographics
The demographics of the 100 patients showed a mean age of 63.46 years (range: 2 - 95 years), with 68% being male. Most arrests were out-of-hospital (70%), while 30% occurred in-hospital. Triage level 1 comprised 52% of patients. The ROSC rate was 22%, and survival to hospital admission was 17%. These findings highlight the challenges of out-of-hospital cardiac arrest.
3.2. Research Findings
3.2.1. Vital Signs
Vital signs (blood pressure, heart rate, respiratory rate, body temperature, and oxygen saturation) were examined to assess patient status during and after cardiac arrest and CPR. The measurements showed wide ranges: Blood pressure (including substantial hypotension), heart rate (including bradycardia and tachycardia), and respiratory rate (including tachypnea and bradypnea) all varied considerably. Body temperature was mostly between 36 - 37°C, with some instances of hypothermia and hyperthermia. Oxygen saturation also varied, with some patients exhibiting low values.
Table 1 shows averages for successful and unsuccessful cases using the two-way repeated measures ANOVA method. Diastolic blood pressure was the only parameter with a statistically significant difference between successful and unsuccessful resuscitation attempts.
| Vital Signs | Unsuccessful | Successful | P-Value |
|---|---|---|---|
| Systolic blood pressure (mmHg) | 73.9 ± 2.4 | 58.8 ± 0.8 | 0.005 b |
| Diastolic blood pressure (mmHg) | 109.7 ± 3.1 | 98.4 ± 8.5 | 0.225 |
| Heart rate (n) | 80.4 ± 2.7 | 79.1 ± 4.1 | 0629 |
| Breathing rate (n) | 16.3 ± 0.6 | 15.5 ± 1.7 | 0.629 |
| Body temperature (°C) | 36.2 ± 0.1 | 36.1 ± 0.2 | 0.900 |
| Oxygen saturation (%) | 83.8 ± 1.4 | 83.5 ± 3 | 0.937 |
Average Vital Signs for Successful and Unsuccessful Cases a
3.2.2. Patient Complaint Data
Patient complaint data showed that cardiorespiratory arrest and heart problems were the most frequent (37%), followed by decreased level of consciousness. Other common complaints included weakness, lethargy, chest pain, and multiple traumas; some patients presented without vital signs. These findings can help healthcare providers identify at-risk individuals and initiate timely interventions.
Triage level analysis revealed variations: Level 1 complaints were mainly cardiorespiratory arrest and decreased level of consciousness; Level 2 complaints commonly included decreased level of consciousness, weakness, lethargy, chest pain, and multiple traumas; Level 3 complaints frequently included weakness, lethargy, chest pain, and shortness of breath, in addition to decreased level of consciousness and heart-related issues.
3.2.3 Patient Medical History
Patient medical history data indicated that a substantial portion of the study population (56%) had no documented pre-existing medical history. Heart problems were the most prevalent condition (18%) among those with known medical conditions. Triage level analysis revealed that a significant proportion of patients in Level 1 and Level 2 triage had no known medical history, with heart problems being the most common pre-existing condition. While conclusions for Level 3 are limited by the small sample size, a considerable proportion also had no known medical history.
3.3. Data from Color Doppler Ultrasound and Echocardiography
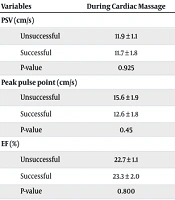
Color Doppler ultrasound and echocardiography data, including PSV, pulse peak point, and EF, were analyzed across three CPR phases: During cardiac massage, the transition phase, and the cardiac massage stop phase. Table 2 presents the average values for these parameters along with the corresponding P-values.
| Variables | During Cardiac Massage | The Transition Phase of Heart Massage to the Stop of Heart Massage | Cardiac Massage Stop Phase | P-Value |
|---|---|---|---|---|
| PSV (cm/s) | ||||
| Unsuccessful | 11.9 ± 1.1 | 30.9 ± 1.7 b | 11.8 ± 0.7 b | 0.000 |
| Successful | 11.7 ± 1.8 | 51.4 ± 1.8 b | 75.3 ± 7.3 b | 0.000 |
| P-value | 0.925 | 0.000 | 0.000 | |
| Peak pulse point (cm/s) | ||||
| Unsuccessful | 15.6 ± 1.9 | 34.5 ± 1.2 b | 16.2 ± 0.1 b | 0.000 |
| Successful | 12.6 ± 1.8 | 56.5 ± 1.6 b | 98.5 ± 6.3 b | 0.000 |
| P-value | 0.45 | 0.001 | 0.000 | |
| EF (%) | ||||
| Unsuccessful | 22.7 ± 1.1 | 33.6 ± 0.9 b | 16.5 ± 0.5 b | 0.000 |
| Successful | 23.3 ± 2.0 | 44.6 ± 1.6 b | 48.1 ± 3.5 b | 0.000 |
| P-value | 0.800 | 0.000 | 0.000 |
Data Averages from Color Doppler Ultrasound and Echocardiography a
A repeated measures two-way ANOVA was used to analyze the Table 2 data. This method examines changes in hemodynamic parameters (PSV, pulse peak point, and EF) across CPR phases and compares successful and unsuccessful resuscitation outcomes. P-values indicate statistical significance.
During active cardiac massage, successful cases had significantly higher PSV (75.3 ± 7.3 cm/s vs. 11.8 ± 0.7 cm/s), pulse peak point (98.5 ± 6.3 cm/s vs. 16.2 ± 0.1 cm/s), and EF (48.1 ± 3.5% vs. 16.5 ± 0.5%) (P < 0.001), indicating better blood flow and cardiac function.
The transition phase, from active cardiac massage to cessation of compressions, also showed significant differences in PSV and pulse peak point between successful and unsuccessful cases. Successful cases had higher PSV (51.4 ± 1.8 cm/s vs. 30.9 ± 1.7 cm/s) and pulse peak point (56.5 ± 1.6 cm/s vs. 34.5 ± 1.2 cm/s) (P = 0.001 for PSV, P = 0.001 for pulse peak point), indicating a more pronounced surge in blood flow. The EF differences were not significant (P > 0.05).
In the cardiac massage stop phase, no significant differences were observed in PSV, pulse peak point, or EF values between successful and unsuccessful cases. The values for PSV (P = 0.92), pulse peak point (P = 0.45), and EF (P = 0.800) were not statistically significant, suggesting these parameters may not reliably indicate resuscitation outcome at this point. This implies that while the initial hemodynamic response and the transition phase are critical, values at cessation of compressions might reflect hemodynamic equilibrium regardless of outcome.
4. Discussion
This study correlated patient triage level with resuscitation outcomes. Level 1 patients (most critical, 52%) had lower ROSC (22%) and survival to admission (17%) rates than Level 2 patients (30% for both outcomes), reinforcing the importance of timely intervention. Successful CPR patients were younger (mean age: 52.58 years). The fact that 70% of successful resuscitations occurred out-of-hospital emphasizes the need for bystander CPR training. These demographics align with existing research (19, 20).
Vital sign analysis showed wide ranges, reflecting physiological instability. Blood pressure, heart rate, respiratory rate, and oxygen saturation varied. A two-way repeated measures ANOVA was used to analyze the data. Diastolic blood pressure was the only parameter with a statistically significant difference between successful and unsuccessful resuscitation attempts. Cardiorespiratory arrest and heart problems were the most common presenting symptoms (37%), emphasizing the need for rapid CPR. Level 1 patients frequently presented with these symptoms and decreased levels of consciousness. Level 2 patients presented with a wider range of complaints. Level 3 patients often presented with less critical symptoms. A substantial proportion of patients, particularly in Levels 1 and 2, had no known pre-existing medical conditions.
This study highlights color Doppler ultrasound and echocardiography as valuable tools for real-time hemodynamic assessment during CPR, providing objective measures of cardiac function and blood flow (21). During active cardiac massage, successful cases had significantly higher PSV, pulse peak point, and EF, indicating more effective blood flow and cardiac function. These higher values align with CPR goals, while lower values may reflect event severity or limitations in compression quality. The transition phase also revealed significant differences in PSV and pulse peak point between successful and unsuccessful cases, with successful cases showing higher values. The EF differences were not significant, which likely reflects an increased likelihood of ROSC as compressions are paused (22).
However, in the cardiac massage stop phase, no significant differences were observed in PSV, pulse peak point, or EF values between successful and unsuccessful cases, suggesting a potential hemodynamic equilibrium (23-25). The four-phase classification system proposed in this study, integrating PSV, pulse peak point, and EF data, offers a framework for evaluating cardiac activity during CPR: Phase 1 (no effective cardiac activity), phase 2 (ineffective cardiac activity), phase 3 (improved cardiac activity), and phase 4 (effective cardiac activity). This approach can aid clinicians in guiding interventions and optimizing resuscitation efforts (26).
Lower values, especially when resuscitation is unsuccessful, are related to damaged heart muscle and the reduction of adenosine triphosphate (ATP) (27, 28). Adenosine triphosphate is the primary energy carrier in cells, essential for myocardial contraction and cellular function. Formed from glucose in the mitochondria, ATP typically converts to ADP (adenosine diphosphate) when energy is used. In oxygen-deprived cells, ADP further breaks down into AMP (adenosine monophosphate). If oxygen deficiency persists, AMP can degrade into adenosine, which rapidly exits the cell. This adenosine loss can prevent cell recovery because energy production becomes impossible. However, if circulation is restored before adenosine escapes, the reverse process can occur: Adenosine converts back to AMP, then to ADP, and finally to ATP, allowing the cell to survive. In cardiac arrest, the heart muscle is often compromised, leading to ATP depletion. Without sufficient ATP (due to ischemia and hypoxia), effective contraction is impaired, and blood flow and cardiac function (PSV, pulse peak point, EF) may be minimal, particularly in unsuccessful resuscitations.
This study demonstrates the value of color Doppler ultrasound and echocardiography as tools for assessing cardiac and circulatory status during and after CPR. These tools can aid in evaluating CPR effectiveness, diagnosing unsuccessful CPR, and potentially determining the time of death. These methods can serve as evidence, particularly in cases where CPR effectiveness is unclear. Based on the findings, recommendations are proposed to advance cardiac arrest management, including: Integrating hemodynamic monitoring; identifying predictors of CPR success; conducting larger studies; investigating predictive factors; developing predictive models; prioritizing quality of life for survivors; exploring cost-effective strategies; identifying risk factors; refining resuscitation techniques; personalizing treatment; and focusing on long-term outcomes (29-31).
Additionally, this study’s findings help explain why some patients do not recover from cardiac arrest. Delays in reaching the hospital for CPR are critical. If the time is prolonged, adenosine exits the cells, making cell recovery irreversible. Similarly, underlying conditions that cause heart or lung damage can lead to cellular oxygen deprivation. If adenosine leaves the cells as a result, the damage will also be irreversible.
4.1. Conclusions
In conclusion, this study demonstrates the potential of color Doppler ultrasound and echocardiography to enhance CPR assessment by providing real-time hemodynamic information. The findings suggest that these technologies can offer valuable insights into cardiac function and blood flow during resuscitation, potentially aiding in clinical decision-making and improving patient outcomes. Further research is warranted to validate these findings and explore the integration of these technologies into routine CPR protocols.