1. Background
Hyperbaric oxygen therapy (HBOT) means breathing 100% oxygen in a pressure more than environment in a chamber or tube. HBOT is an excellent treatment for decompression injury, which is a risk of scuba immersion (1). Other abnormalities treated with HBOT include serious infections, air bubbles in blood vessels, chronic diabetic foot ulcers, and radiation injury (2). Some clinical trials proved that HBOT are useful in the treatment of severe common ischemic diabetic foot ulcer (3). It increases long-term health related pleasure of life (QOL) in these patients, which is possibly attributable to better ulcer healing (3). HBOT has an effective impact on post-concussion syndrome (PCS) even years after mild traumatic brain injury (4). Different studies defined that HBO significantly improves hidradenitis suppurativa (HS) (2). QOL is an important health outcome, and it represents the final goal of all health interventions. QOL is measured as physical, mental, social functioning, and perceived physical and mental well-being (5). A large number of articles have shown the relevance of assessment of health-related quality of life (HR-QOL) and functional position as important findings in standard clinical outcomes (6). Radiotherapy is used in the setting of beneficial treatment for head and neck malignancies. Xerostomia and its related problems manifest when major salivary glands are included in the irradiation zone. This complication decreases QOL in patients. HBO is a unique therapy and a prevention choice for radio necrosis of the jaw bones and soft tissue. We do not know to what extent HBOT improves xerostomia and xerostomia-related health (7).
HBO therapy leads to significant neurological improvement in post stroke patients in acute and late phases (8, 9). Hyperbaric oxygen therapy is safe for kids with radiation-induced bone and soft tissue necrosis; it does not cause any complication in them. HBOT is a potential option for prevention and treatment of radiation-related adverse events (10).
HBOT is a healthy treatment modality suggesting rapid cure in the healing radiation-induced osteoradionecrosis either alone or as a combination therapy. Hyperbaric oxygen therapy cures radiation soft tissue necrosis, cystitis, and proctitis (11). There are various troublesome diseases that affect QOL in patients. Traditional and convenient medical treatments cannot change QOL in these patients. HBO significantly improves QOL in patients. A systematic review cumulates robust evidence to prove the clinical effect of a treatment. This systematic review aimed at assessing the researches that focused on change in quality of life of patients with different diseases after HBO treatments.
2. Methods
2.1. Data Source, Search Strategy, and Eligible Studies
We conducted a systematic search to find English articles (RCTs) that were published before April 2017. We searched PubMed, institute of scientific information (ISI), SCOPUS, Web of science, Ovid, Science direct, ProQuest, Wiley, Cochrane, Ebsco host, and Google Scholar as the main international electronic data sources. The reference lists of all the papers and electronic journals were searched for further researches. The medical subject headings (MESH), entry terms of PubMed, and entree of Scopus were used for most comprehensive and efficient searches. We used MESH keywords to search PICO Abbreviations, which were as follow: P: “Patients” [Mesh]; I: “Hyperbaric Oxygenation” [Mesh]; C: comparison group treated with no drug or routine treatment; and O: “Quality of Life” [Mesh]. Two independent authors (A.N and M.D) conducted data extraction using inclusion and exclusion criteria and excluded studies that did not use HBOT in a clinical trial (with follow-up). Quality assessment of clinical trial studies were performed by other authors (A.M & S.A.M) based on the consolidated standards of reporting trials (CONSORT) checklists.
2.2. Data Extraction
2.2.1. Quality Appraisal of Articles
Two independent researchers extracted data using specific inclusion and exclusion criteria. The JAMA user’s guideline quality assessment scales for clinical trials was used to assess quality of included articles (complementary note). This user guideline includes 3 key questions about internal and external validity. We used internal validity items to evaluate the articles. Internal validity had 6 main questions about the following items:
1) Randomization
2) Allocation treatment
3) Patient and physician blinding
4) Placebo and intervention groups similarity
5) Follow-up time
6) Type of result analysis
The item got a score of 1 if the answer to the item was “yes”. Then, we collected the score of all 6 items. We considered a study eligible in this systematic review, if it gained 3 of all 6 scores. Discrepancies were resolved through discussions between reviewers and reaching consensus.
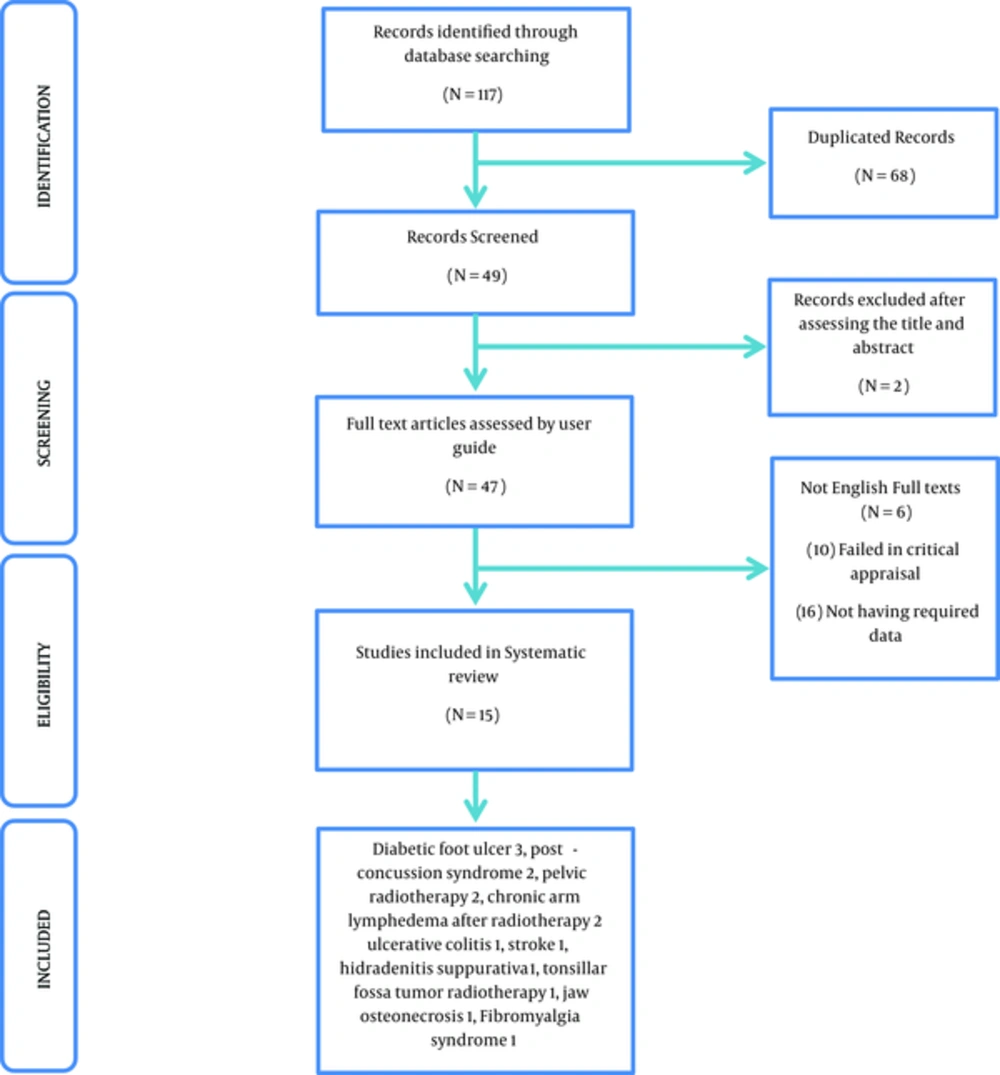
Quality assessment based on JAMA user guide was conducted on all 15 RCTs included in this research (Figure 1).
2.2.2. The Following Characteristics Were Extracted
Disease name, first author, country name, years of publication, sample size in intervention and control groups (male/female ratio in each group), QOL questionnaire name, complications, inclusion and exclusion criteria of each study, the mean age of patients in each intervention, control, follow-up time, type of convention treatment, and HBOT schedule in each disease. We resolved discrepancies through discussion among 3 reviewers and reaching a consensus.
Inclusion criteria were as follow: HBO therapy, physical and mental health for HBOT, patients access to follow- up, and informed consent, age 18 years or older.
Exclusion criteria were as follow: Having chest disease or abnormality, inner ear abnormality or disease, claustrophobia, no informed consent, pregnancy, pneumothorax, severe chronic obstructive pulmonary disease, recent chest surgery, upper or lower airway infection, mental problems (especially claustrophobia), head trauma, seizure, epilepsy, and heart failure (ejection fraction < 35%). Smoking was not allowed during the research.
3. Results
3.1. Characteristics of the Included Studies Are as Follow
The initial search included 117 citations, of them 68 were duplicates, and 49 were examined in more details, 2 of which were excluded after reading the title and abstract. Then, 47 full texts were assessed by user guides, of them 16 studies were excluded because they lacked the required data, 10 studies failed in critical evaluation, and 6 did not have English full texts. Finally, 15 articles related to the study domain were found (Figure 1 and Table 1). Final studies included 14 prospective randomized and 1 non-randomized clinical trials.
| N | First Author | Country | Y.P | Disease | QOL Questionnaire | Intervention / Number | Control / Number | Total Mean Age (Years) of Patients | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Hamza Yildiz (2) | Turkey | 2015 | Hidradenitis suppurativa | DLQ1, HSS1, SS, VAS | HBO + antibiotic | Antibiotic | 35.7 | 10 weeks |
| 2 | M. Londahl (3) | Sweden | 2006 | Chronic diabetics food ulcers | SF36, three minute walk test | HBOT | Air | Not mentioned | 48 weeks |
| 3 | Suyanto Sidik (12) | Indonesia | 2007 | Pelvic radiation | Karnofsky scale | HBOT | Routine care | 47 | 24 weeks |
| 4 | David N. Teguh (13) | Netherlands | 2009 | Oropharyngeal and nasopharyngeal cancer (radiotherapy) | (QLQ)-C30, QLQ-H and N35, (PSS) VAS | HBOT | Routine care | Not mentioned | 72 weeks |
| 5 | R. Scott Miller (14) | USA | 2015 | Post-concussion symptoms (pcs) | RPQ-3 subscale, | HBO sessions | Routine care | 31 | 48 weeks |
| 6 | Shai Efrati (15) | Israel | 2015 | Fibromyalgia syndrome | SF-36 questionnaire | HBOT | No treatment | 49 | 8 weeks |
| 7 | Shai Efrati (16) | Israel | 2013 | Post stroke | NIHSS, ADL, EQ-5D, EQ-VAS | HBOT | No | 62 | 16 weeks |
| 8 | Rahav Boussi-Gross (4) | Israel | 2013 | Post-concussion Syndrome | EQ-5D, EQ-VAS | HBOT | Routine care | 43 | 16 weeks |
| 9 | Maria Pagoldh (17) | Sweden | 2013 | Severe attack of ulcerative colitis | (SF-36), (IBDQ) | HBOT + conventional medical treatment | Conventional medical treatment | 32 | 6 weeks |
| 10 | Richard E. Clarke (18) | Columbia | 2008 | Chronic refractory radiation proctitis | bowel-specific QOL assessment | HBOT | Air | Not mentioned | 3 and 6 months and Years 1 - 5 |
| 11 | M. Lo ndahl, M (3) | Sweden | 2010 | Diabetes and chronic foot ulcer | SF-36 | HBOT | Air | 69 | 12 months |
| 12 | Lone Gothard (19) | UK | 2010 | Chronic arm lymphedema after radiotherapy for early breast cancer | UK SF-36 health survey questionnaire | HBOT | No control group | 62.5 | 12 months |
| 13 | Lone Gothard (20) | UK | 2004 | Chronic arm lymphedema after radiotherapy for cancer | QLQ-C30 and breast module BR23 | HBOT | Air | 64 | 12 months |
| 14 | A. Abidia (21) | UK | 2003 | Ischemic diabetic lower extremity ulcers | SF-36, HAD scale | HBOT | Air | 71 | 6 months |
| 15 | John J. Freiberger (22) | UK | 2012 | Bisphosphonate-related osteonecrosis of the Jaw | Duke health profile | conventional therapy + HBO | Conventional therapy | 66 | 24 months |
The Main Characteristics of Eligible Studies on the HBO and QOL in Patients with Different Types of Diseasea
The countries for HBO therapy in these RCTs were UK (26.7%), Israel (20%), Sweden (20%), Indonesia (6.66%), Colombia (6.66%), USA (6.66%), Netherland (6.66%), and Turkey (6.66%).
3.2. Demographic Characteristics of the Patients
We had 415 patients in the intervention group (HBOT), with a mean age of 41.88 years and a male to female ratio of 164/108 (1.52).
Also, the sample size in the control group was 391 patients (routine care), with a mean age of 38.29 years and a male to female ratio of 178/83 (2.14).
3.3. Type of Disease in RCTs
The most frequent clinical trials that evaluated HBO therapy was in the treatment of diabetic foot ulcer (20%), post-concussion syndrome (13.3%), pelvic radiotherapy (13.3%), chronic arm lymphedema after radiotherapy (13.3%), ulcerative colitis (6.67%), stroke (6.67%), hidradenitis suppurativa (6.67%), tonsillar fossa tumor radiotherapy (6.67%), jaw osteonecrosis (6.67%), and fibromyalgia syndrome (6.67%).
3.4. Types of QOL Questionnaires
The researchers evaluated health-related quality of life with different questionnaires related to patients’ disease. They assessed multidimensional concept of QOL that included domains related to physical, mental, emotional, and social aspects related to a disease or its specific therapeutic approaches (Table 1).
The most frequent questionnaire was SF-36 (36-item short form survey (21.4%) (23), EORTC QLQ-C30 (European organization for research and treatment of cancer), and QLQ, a questionnaire developed to assess the quality of life in cancer patients (24), H&N35 (Head and Neck) (25), and cancer module performance status scale (PSS) (26).
3.5. HBO Therapy
All HBO therapy interventions were performed at multi- place hyperbaric chambers, and ideally, for 5 days a week according to schedule (eg, 8 weeks, 40 treatment sessions) (15). HBOT schedules for treating troublesome diseases that improved QOL of patients are presented in Table 2; we have several protocols for HBOT in various diseases. Nearly 100% of eligible studies used HBOT at 2.5 - 3 ATA/ 90 minutes daily 5 days a week for 8 weeks, extending over 10 weeks, but the sessions should have not exceeded 40. We did not find any side effects (inner and middle air barotrauma, sinus barotrauma, oxygen toxicity, and confinement anxiety) relevant to HBOT in this systematic review.
| N | Disease Name | HBOTa Schedule | Control | HBOT Number | Control Number | Male/Female Ratio HBOT, Mean Age ± SD (Years) | Male/Female Ratio, Control Group, Mean Age ± SD (Years) |
|---|---|---|---|---|---|---|---|
| 1 | Hidradenitis suppurativa (2) | HBOT sessions 120 minutes, a period of compression in air for 20 minutes, followed by treatment at 2.4 atmospheres absolute (ATA) for 3 periods of 25 minutes separated by two 5-minute air breaks (mask off), followed by a decompression period of 15 minutes. 5 days/week for 4 weeks (20 treatment sessions, once per day except at weekends. | Combination of clindamycin (300 mg orally, twice per day, taken with food) and rifampicin (300 mg orally, twice per day, taken on an empty stomach) were included in the study. All patients received this therapy for 10 weeks. | 22 | 21 | M/F:7/15, mean age: 33 | M/F:11/10, mean age: 37.5 |
| 2 | Chronic diabetic food ulcers (27) | HBOT at 2.5ATA/ 90 minutes daily 5 days a week /8 weeks, extended over 10 weeks, but sessions must not exceed 40 | Primary healing and maintain ambulation by optimization of circulation, ulcer off loading and treatment of infection. | 38 | 37 | Not mentioned | Not mentioned |
| 3 | Pelvic radiation (12) | HBOT 100% oxygen with pressure 2 - 3 (ATA) in high pressure chamber for more than 18 times, during 6 months follow up | Routine care after radiotherapy | 32 | 33 | M/F: Not mentioned, mean age: 47 ± 5.5 | M/F: Not mentioned, mean age: 44.7 ± 6.2 |
| 4 | Oropharyngeal and nasopharyngeal cancer (radiotherapy) (13) | HBOT consisted of 30 sessions at 2.5 ATA with oxygen breathing for 90 minutes daily, 5 days per week, applied shortly after the RT treatment was completed. | Brachytherapy boost dose to the primary tumor ranged from 11 to 22 Gy, and prescribed Cyberknife boost dose ranged from 11.2 to 16.5 Gy. The parotids received a mean dose of 6 - 67 Gy (median dose, 37 Gy) | 8 | 11 | Not mentioned | Not mentioned |
| 5 | Post-concussion symptoms (PCS) (14) | 40 HBOT sessions administered at 1.5 (ATA), 40 sham sessions consisting of room air at 1.2 ATA, or no supplemental chamber procedures. | Routine PCS care | 24 | 23 | M/F: 24/0, mean age:32.5 | M/F: 23/0, mean age:30.3 |
| 6 | Fibromyalgia syndrome (15) | 40 sessions, 5 days/week, 90 minutes, 100% oxygen at 2ATA. | No treatment | 24 | 26 | M/F: 0/24, mean age: 50.4 ± 10.9 | M/F:0/26, mean age: 48.1 ± 11.1 |
| 7 | Post stroke (16) | Two months of 40 sessions (5 days/week), 90 minutes each, 100% oxygen at 2 ATA. | Routine stroke care | 37 | 37 | M/F: 22/8, mean age: 61 ± 12 | M/F:17/12, mean age: 63±6.3 |
| 8 | Post-concussion syndrome (4) | 40 treatment sessions (5 days/week), 60 minutes each, with 100% oxygen at 1.5 ATA | Routine PCS care | 45 | 45 | M/F: 16/0, mean age: 42.5 ± 12.6 | M/F: 24/0, mean age: 45.7±10.9 |
| 9 | Severe attack of ulcerative colitis (17) | 2.4 ATM for 90 minutes/session, 5 days/week, for 6 consecutive weeks (30 sessions) + Conventional therapy | initial intravenous GCS treatment betamethasone 4 + 0 + 4 mg (prednisolone equivalence 67 mg), oral mesalazine (1 200 mg twice daily on days 1 - 5 and thereafter 2400 mg twice daily), suppository prednisolone (20 mg once daily) and enema prednisolone (37.5 mg once daily | 10 | 8 | M/F: 7/3, mean age: 29.5 | M/F: 4/4, mean age: 34.8 |
| 10 | Chronic refractory radiation proctitis (18) | 100% oxygen at 2.0 ATA for 90 minutes, once daily, five times weekly. 10 additional sessions were provided to selected patients, depending on the individualized responses | 21% oxygen (normal air) at 1.1 ATA, once daily, five times weekly. | 64 | 56 | M/F: not mentioned, mean age: not mentioned | M/F: Not mentioned, mean age: not mentioned |
| 11 | Diabetes and chronic foot ulcer (3) | 5 days a week for 8 weeks (40 treatment session extended to 10 weeks, but the number of treatments was not allowed to exceed 40 | Routine diabetic care | 38 | 37 | M/F: 76/24, mean age: 67 | M/F: 86/14, mean age:71 |
| 12 | chronic arm lymphedema after radiotherapy for early breast cancer (20) | 100% oxygen at 2.4 ATA for 100 min in a multiplace hyperbaric chamber on 30 occasions over a period of 6 weeks | No control group | 21 | - | M/F: 1/20, median age: 64, (range 53 - 76). | - |
| 13 | chronic arm lymphedema after radiotherapy for cancer (19) | 2.4 (ATA) in a hyperbaric chamber, the total time at 2.4 ATA was 100 minutes, including two 5- minutes air breaks. Each participant received a total of 30 pressure exposures, treating 5 days a week for 6 weeks | best standard care for lymphedema | 21 | 21 | M/F: not mentioned, mean age: 63.2 | M/F: not mentioned, Mean Age: 62.1 |
| 14 | Ischemic diabetic lower extremity ulcers (21) | 100% oxygen at 2.4 atmospheres of absolute pressure for 90 minutes daily (total of 30 treatments) | air | 9 | 9 | M/F: 2/1, mean age: 72 ± 12.6 | M/F: 1/2, mean age: 70 ± 6.6 |
| 15 | Bisphosphonate-related osteonecrosis of the Jaw (22) | HBO administered at 2 ATA twice a day for 40 treatments as an adjunct | surgery and antibiotics | 22 | 27 | M/F: 9/3 mean age: 66.1 | M/F: 12/15, mean age: 66.3 |
Effective Schedule of HBO Therapy and Type of Treatment in Control Group in RCTs
3.6. Routine Care
Of the patients, 46.7% used conventional treatment for their disease in the control group, 33.3% used air as placebo, 6.7% received no treatment in the control group, and 6.7% of the studies had no control group.
4. Discussion
This systematic review aimed at evaluating data from clinical trials with follow-up to find success, failures, and complications of HBOT in improving QOL in patients. The results confirmed that HBOT is safe to be used in the treatment of patients with disabling and troublesome diseases and improves QOL. The number of clinical trials on HBO therapy is dramatically increasing because HBOT success is more than conventional therapy success in many diseases. HBOT is mostly performed in developed countries, such as USA and UK. According to SF-36 instrument, HBOT improves vitality, physical function, body pain, total health perceptions, mental health and physical, emotional, and social role functioning in patients with troublesome diseases (15, 17, 19, 21, 27).
The main worldwide diseases for HBO therapy were chronic diabetic foot ulcers, post-concussion syndrome after brain injury, and chronic arm lymphedema after radiotherapy, or pelvic radiotherapy. The least clinical trials were on HBO therapy in acute attack of ulcerative colitis, stroke, hidradenitis suppurativa, tonsillar fossa tumor radiotherapy, jaw osteonecrosis, and fibromyalgia syndrome. The results presented here confirmed that HBOT caused no serious complications in patients. Moreover, the relative risks of death and morbidity (incidence of disease) and complication (hospital readmission, seizures, infection, and limb amputation) were not significantly improved in patients who received hyperbaric oxygen therapy compared with the control group. However, we could not use meta-analysis because of using different QOL questionnaires in different studies and because of the low number of some clinical trials.
An excellent improvement was observed in QOL of patients who had received HBOT combined convention therapy compared with controls. Thus, future RCTs with more sample size would be required to incorporate more robust outcome measures. This review article was based on a comprehensive search strategy.
4.1. Diabetic Foot Ulcer
We found an excellent effect of HBOT on promoting QOL of diabetic patients by healing their foot ulcers. AJ Bishop et al. conducted a literature review and concluded that HBOT reduces amputation rates and improves healing wounds in diabetic patients (28). Kessler L et al. indicated that HBOT accelerates the cure rate of no ischemic chronic diabetic foot ulcers (29). Kalani M et al. found that adjunctive HBOT is excellent for healing specific patients with diabetic foot ulcers. It accelerates the rate of cure, decreases the need for foot amputation, and increases the pleasure in life in long-term follow-ups (30). Adjunctive HBOT is the best choice for improving mental, physical, and social aspects of QOL in these patients.
4.2. Post-Concussion Syndrome
HBOT is a non-invasive and no-drug way to repair damaged tissue; its positive effect is the result of 2 oxygen-dependent processes. Researchers ascertained a large and multicenter cohort for evaluating HBOT in chronic traumatic brain injury and post-concussion syndrome. They found that multiple doses of hyperbaric therapy are effective in the treatment of PCS, while others are not (31). Paul G. Harch et al. mentioned that the biological effects from 1 minute exposure to 1.09 ATA or 3 minutes at 1.04 ATA promote the symptomatic improvements in central nervous system (32). HBOT is the best choice for these patients to improve their health state, usual activities, anxiety, and depression (4).
4.3. Pelvic Radiotherapy
Radiation therapy is used successfully to cure pelvic malignancies, but morbidity from hemorrhagic cystitis is a major long-term complication in 1% to 2% of patients. Obliterative endarteritis secondary to ionizing radiation leads to cells hypoxia and poor tissue improvement (33). HBOT can improve healing these lesions. Ranjiv Mathews et al. concluded that HBOT improved angiogenesis and increased cure in radiation injured tissue, such as bladder (34). Romana Mayer et al. demonstrated that HBOT was an effective treatment to heal patients with late gastrointestinal and genitourinary morbidity, when conventional drug was not effective. HBOT should be prescribed as soon as possible in patients with radiation cystitis (33).
In this review, we found that HBOT improves patients’ functional impairment and subjective well-being by tonsillar fossa tumor radiotherapy (13) and pelvic radiotherapy (18) by oxygenation and lesion repair.
4.4. Chronic Arm Lymphedema After Radiotherapy
Lymphedema due to radiation is a common and major side effect of breast cancer curative therapy in early stages. HBOT improves cure in bone ischemic due to radiotherapy and improves soft tissue injuries too, but it is untested in arm lymphedema (20). In this review, we did not find QOL improvements in these patients. Perhaps, the type of questionnaires (EORTC QLQ-C30) was inappropriate or sample size was small, according to authors’ description (20). Lone Gothard in 2010 did not find good evidence for HBOT in the treatment of arm lymphedema following breast cancer surgery and its adjuvant radiotherapy in early stages (19). HBOT cannot improve QOL in these patients.
4.5. Stroke
Stroke recovery correlates with non-active brain lesions, which may persist for a long time. We found significant improvements in patients with stroke following HBOT, and it can lead to neurological improvements even at late chronic stages (11). Gennady G. Rogatsky et al. demonstrated the efficacy of HBOT in neurologic status of acute ischemic stroke (35). HBOT improves consciousness level, sensory and motor function, and daily living activity in patients after acute or chronic stroke (16).
Hidradenitis suppurativa (HS) is a chronic suppurativa and scarring inflammatory disease with predilection in the apocrine gland-bearing fields (36). We found that adjunctive HBOT is effective in improving antibiotic treatment of HS. HBOT has good tolerance, with no unexpected complications. Ozdemir et al. found that HBOT is an effective therapy in problem wounds and can be used in managing HS lesions (37). HBOT decreases skin problem (painful lesions, daily living activity, social activities, and relationships) and has a positive effect on patients’ life (2).
4.6. Tonsillar Fossa Tumor Radiotherapy
Radiotherapy of this area causes severe pain in swallowing, sticky saliva, xerostomia, and pain in mouth. Teguh et al. found that Patients, who receive HBOT after tumor radiotherapy in mouth and fossa, have better QOL scores (13). CHU H et al. concluded that HBOT is a good adjuvant in radiotherapy for advanced oropharyngeal cancer (38). These results are relevant to our systematic review. HBOT can decrease pain in mouth and jaw, soreness in mouth, painful throat, and dry mouth (13).
4.7. Jaw Osteonecrosis
Bisphosphonates prevent bone turnover by suppressing osteoclast signal transduction, maturation, and longevity. In these patients, suppressed turnover can impair oral wound healing, leading to a painful mouth, and osteoporosis-like jaw necrosis called bisphosphonate-related osteonecrosis of the jaws. Freiberger et al. found that hyperbaric oxygen therapy has the potential effect to improve bone turnover by signaling the impact on osteoclasts (39). Marx et al. indicated that HBOT can prevent osteoradionecrosis (40). Their results are similar to our findings. HBOT improves sleeping, nervousness, feeling, and social activities in patients (22).
4.8. Fibromyalgia
Fibromyalgia is a chronic pain in multiple areas of the body (41). Chronic pain is one of the most clinical problems, which is difficult to treat. HBOT treatment has been done for patients with chronic pain syndromes with excellent effectiveness (42). Sutherland et al. indicated that HBOT is useful in modulating animal and human pain (43). In our systematic review, the efficacy of HBOT in healing and improving general health, daily activity, emotional problems, and body pain in patients was confirmed (15).
4.9. Ulcerative Colitis
HBOT has a very good effect on colonic damaged tissues (44). Buchman AL et al. found that HBOT is the first successful treatment in ulcerative colitis, refractory to conventional therapies (45). Gulec et al. concluded that HBOT has beneficial effects on the course of distal colitis and that antioxidant systems may be involved in its mode of action (46). In our study, we did not find detectable differences in QOL of patients. According to authors’ comments, perhaps the reason for lack of evidence on HBOT as a treatment option in a severe attack of UC was the small number of patients (17).
5. Conclusions
HBOT is a safe procedure for disease treatment and improves different aspects of QOL in patients with diabetic foot ulcer, post-concussion syndrome, pelvic radiotherapy, stroke, hidradenitis suppurativa, tonsillar fossa tumor radiotherapy, jaw osteonecrosis, and fibromyalgia syndrome. HBOT is not done in Iran as well as other countries. Policymakers should support hyperbaric medical doctors (M.D.) to establish HBOT chambers for more research and treatment and increase QOL in patients all over the world, especially in Iran. We suggest that HBOT be added to conventional treatment of these patients as an adjuvant.
The main limitation of our systematic review was the lack of numerous RCTs for treatment of different types of diseases. Most articles were prospective studies without clinical trials. The best suggestion is designing appropriate RCTs with large sample size to gain robust evidence about HBOT benefits, failures, and complications in treatment of different types of diseases in the world.