1. Background
Malassezia species are the natural flora of the skin in humans and warm-blooded animals (1). They are susceptible to heat, and most of them need long chain fatty acids to grow. This fungus can be seen in two forms of yeast and mycelium (dimorphic) in 90% of adults (2).
These yeasts are mostly seen in regions such as the neck, back, arms, and abdomen due to sebaceous glands accumulation and in individuals aged 10 to 19 years due to increased activity of sebaceous glands that provide the necessary lipids for the development of Malassezia species. Conditions such as AIDS, taking antibiotics, pregnancy, and taking steroids can cause different skin problems, which can be intensified by Malassezia species; however, the role of these yeast species in some skin diseases is ambiguous. For many years, all the damage caused by Malassezia furfur, especially skin disorders such as dandruff, seborrheic dermatitis, and pityriasis versicolor, were attributed to a single species (3).
Seborrheic dermatitis is a chronic dermatitis observed in both infants and adults. In adults, rash tends to appear on the central parts of the face, eyebrows, and head and often causes the skin to scale. Seborrheic dermatitis can also occur under the armpits, on groin, or in middle of the chest. In men, this condition sometimes occurs in the beard area. The cause of seborrheic dermatitis is unclear, but it is sometimes associated with an overgrowth of Malassezia, which naturally exists on the skin surface (4). Although seborrheic dermatitis could be treated with antifungal antibiotics, unfortunately, drug resistance cases are reported frequently. Therefore, the use of different antimicrobial compounds or agents to prevent or control such resistances is recommended. Among these compounds are medicinal herbs that are not only economically justifiable, but their availability, extraction, and application in pharmacy and medicine are confirmable.
Nowadays, scientists pay particular attention to using herbal and traditional medicine. In countries like Iran, there is a long history of applying herbal medicine for treating diseases. For instance, the great Iranian scientist Abu Ali Sina (Avicenna) had considered using herbs. Aloe vera belongs to the Asphodelaceae family. This plant is similar to broad-leaved cactus and is a permanent, meaty, and juicy plant, which reaches a maximum height of two meters. Surprisingly, water constitutes 96% of Aloe vera gel. The compounds found in Aloe vera gel contain polysaccharides that are capable of reducing and restoring inflammation. It also has antimicrobial properties. This plant contains hydroxyl anthracene derivatives and aloe resin A, B and C. Also, glucose, mannose, and cellulose sugars, oxidase, amidases, and catalase enzymes, vitamins B1, B2, B6, C, and E, folic acid, and minerals such as calcium, sodium, magnesium, zinc, copper and chromium form its other nutrients (in low quantities) (5).
2. Objectives
In this study, considering the community approach to traditional medicine and treatment with natural substances and with respect to the fewer side effects of herbal remedies, we determined the effect of Aloe vera extract on the growth of clotrimazole-resistant Malassezia furfur species isolated from patients with seborrheic dermatitis in vitro.
3. Methods
3.1. Sample Collection and Mycologic Identification
Sampling was performed on 102 suspected cases of seborrheic dermatitis (with symptoms such as scaling and some itching) from three specialized skin clinics in the city of Sari, Mazandaran province, north of Iran. After completeing a written informed consent, the participants filled a checklist that contained items on age, gender, occupation, and nightly sleep time. The participnts were selected using the randomized smpling method. Those who had taken steroids or antibiotics were excluded from the study. The specimens were collected from the skin of the neck, face, arm, abdomen, shoulder, and scapula using a sterile surgical knife. The scales were stained with methylene blue and 10% KOH and were then cultured on dixon agar (Merck, Germany), which was modified with cyclohexamide and chloramphenicol in the form of transplantation. The samples were incubated for 7 to 10 days at 32°C.
The yeast cells were first examined directly by microscopy based on their colony forms and then adjacent to Calcofluor-white. In the present study, 1 - 2 single spores were identified as positive 1 (+1) and 2 - 6 integrated spores or 3 - 12 single spores were considered as positive 2 (+2) (6).
Finally, Malassezia species were identified by catalase and esculin hydrolysis tests after growing on sabouraud dextrose agar (Merck, Germany).
3.2. Antifungal Susceptibility Test
Drug susceptibility test to clotrimazole was performed using the broth microdilution method according to CLSI-M27-A3 instruction (7). After preparing the stock from clotrimazole powder (Gibco, Germany) in 25% ethanol and diluting it at the range of 16 - 0.03 µg/mL, dilutions were poured in 96-well ELISA microplates containing dixon broth (Merck, Germany) adjacent to yeast suspension (1 × 103 cells per mL) counted by neubauer chamber. Then, they were placed in a shaking incubator at 32°C for 72 hours. In reporting the minimum inhibitory concentration (MIC), ELISA Reader was used in addition to determination of turbidity. To determine the minimum fungicidal concentration (MFC), 100 μL of the wells’ content with a concentration higher than the MIC, together with 100 μL of the positive control were separately transferred to dixon agar medium and were incubated for 3 - 5 days at 32°C. The concentration of the well with no growth on the mentioned medium was reported as MFC. In this study, Candida krusei ATCC6258 and Candida parapsilosis ATCC 22019 were used as controls.
3.3. Preparation of Aloe vera Extract
To prepare the plant extract, Aloe vera was procured freshly from a greenhouse. After extraction of gel from the Aloe vera leaf, it was mixed and soaked with 70% ethanol at a ratio of 1 to 10 (each 100 cc of gel was soaked with 1000 cc of ethanol), and then the mixture was placed in a shaker for 24 hours. After 24 hours, the mixture was filtered and placed in a rotary container to evaporate the solvent (ethanol). Afterwards, the extract was placed in a water bath for 24 hours to form a honey-like liquid.
3.4. Evaluating the Inhibitory Effect of Aloe vera Extract
The antifungal effect of different concentrations of Aloe vera extract on all the clotrimazole-resistant isolates was investigated using the agar well diffusion method. In this method, first a microbial suspension of 0.5 McFarland was prepared and cultured in the form of spreadsheet on a dixon agar medium. Wells with a diameter of 7 mm were created on the medium and filled with 100 μL of the extract at the concentrations of 250, 125, 62.5, 31.25, and 15.6 mg/mL. One well containing distilled water was considered as the negative control. After adding dilutions to wells, the plates were incubated at 32°C for 5 days. After that, the mean diameter of the inhibition zones was reported in milimeters, and inhibition zones with a diameter of more than 12 mm were considered as sensitive and the ones with a diameter of less than 10 mm were considered as resistant to the extract.
The MIC of the honey-like Aloe vera extract, which had shown a good antifungal effect in the well diffusion method, was determined by the broth microdilution method at a dilution of 1024 - 2 μL/mL.
3.5. Statistical Analysis
Comparison of mean treatments was performed using Duncan’s multiple range test and one-way analysis of variance (ANOVA) at a confidence level of 0.001. All statistical analyses were performed using SPSS, and all figures were drawn with MS excel (all measurements were repeated three times).
4. Results
After conducting biochemical tests to identify Malassezia species from the 102 collected samples, 72 samples were reported to be positive. In investigating the frequency of Malassezia strains among patients suspected of seborrheic dermatitis, Malassezia furfur showed the highest frequency of 77.8% (56 cases), which was more frequently seen in female patients (86%), followed by Malassezia globosa and Malassezia restricta with 12 (16.7%) and 4 (5.5%) cases, respectively.
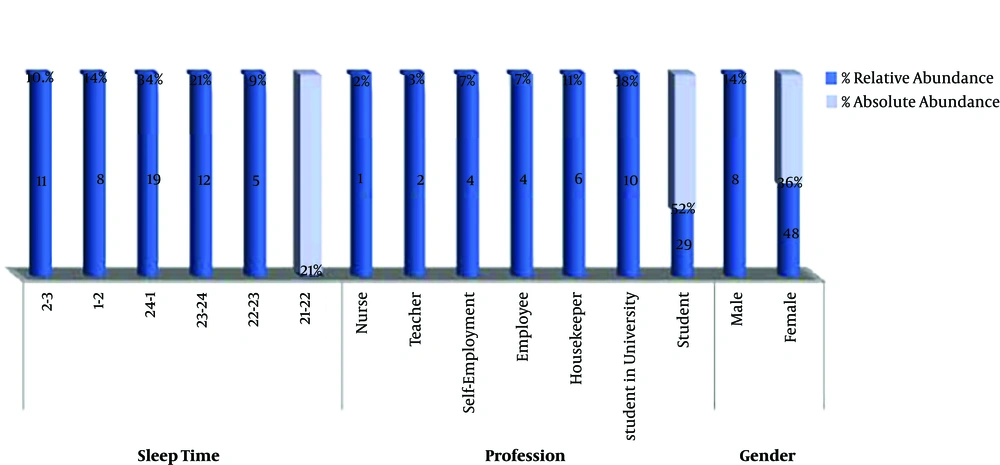
The highest and lowest frequencies of Malassezia furfur isolates were observed in students (52%) and nurses (2%), respectively, which means that students are more exposed to this yeast, thus, they are suggested as a high-risk group in this study. When investigating the relationship between sleep time and the prevalence of the disease, it was found that the highest frequency of Malassezia furfur was observed in people who went to sleep between 12 and 1 AM and the lowest frequency was found in the ones who slept between 9 and 10 PM (Figure 1). This indictes that the number of patients with Malassezia furfur is higher among people who go to sleep at midnight. In determining the drug sensitivity test by broth microdilution test, the MIC was measured in the range of 4 - 16 μg/mL and the MFC level was also in the range of 8 - 16 μg/mL. This means that 50% of Malassezia furfur isolates were resistant to clotrimazole, 32% were susceptible and 18% were semisusceptible (Table 1).
| Characteristics | Resistant | Semi-Sensetive | Sensetive | Total |
|---|---|---|---|---|
| Gender | 56 (100) | |||
| Female | 23 (41.07) | 9 (16.07) | 16 (28.57) | |
| Male | 5 (8.93) | 1 (1.79) | 2 (3.57) | |
| Profession | 56 (100) | |||
| Student | 14 (25) | 6 (10.71) | 9 (16.07) | |
| Non-student | 14 (25) | 4 (7.15) | 9 (16.07) | |
| Sleep time | 56 (100) | |||
| Late time | 19 (33.93) | 7 (12.5) | 12 (21.4) | |
| On time | 9 (16.07) | 3 (5.4) | 6 (10.7) |
The Frequency of Clotrimazole Resistance in Malassezia Isolates From Patients
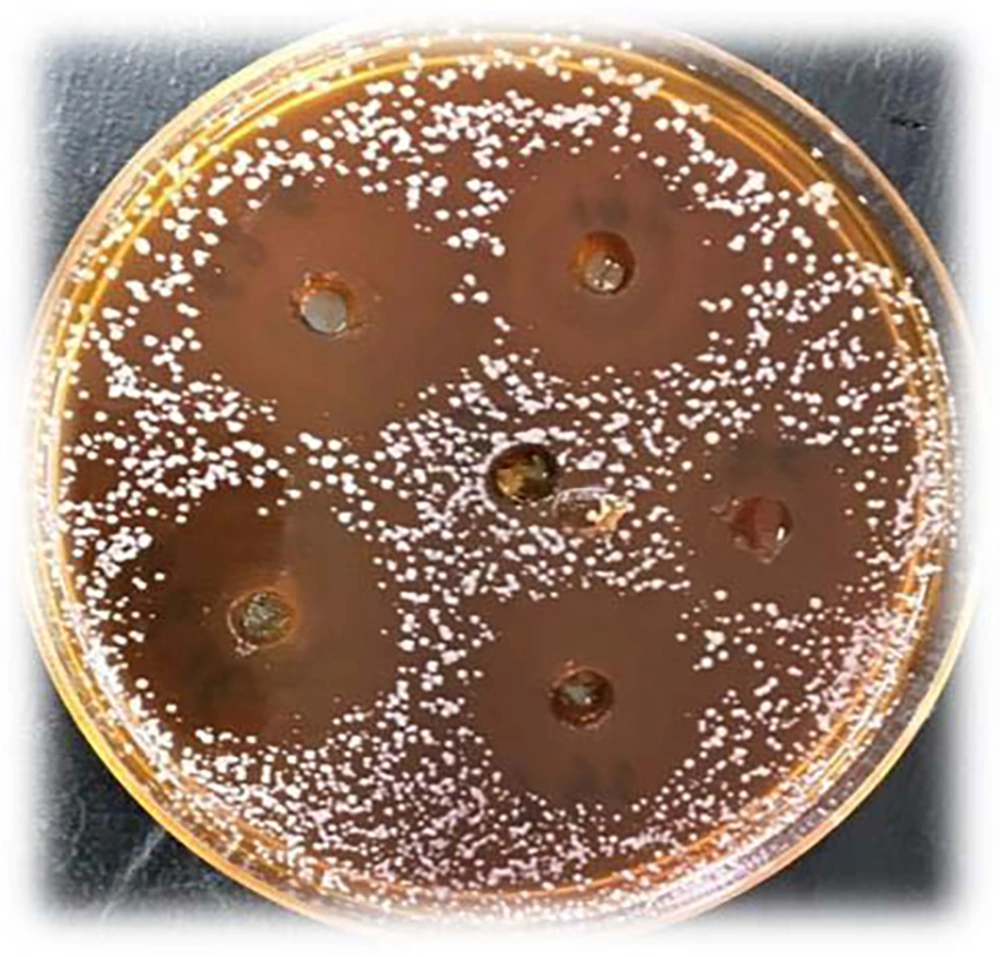
The results of the well diffusion method showed that the highest and lowest mean diameters of the inhibition zone were observed in the concentrations of 250 mg/mL (average = 25.35 mm) and 15.6 mg/mL (average = 11.52 mm), respectively (Table 2). In fact, all the concentrations of the extract showed good antimicrobial effect (Figure 2), but with an increase in the concentration of the extract, the diameter of the inhibition zone also increased.
| Aloe vera Extrac Concentrations (mg/mL) | Inhibition Zone Diameter(mm)b |
|---|---|
| 250 | 25.4 ± 0.3 |
| 125 | 22.5 ± 00.01 |
| 62.5 | 14.65 ± 00.02 |
| 31.25 | 13.59 ± 00.00 |
| 15.6 | 11.52 ± 00.00 |
Diameter of Inhibition Zone Due to the Effect of Aloe vera Extrac on Growth of Malassezia Isolatesa
In this study, the MIC of Aloe vera extract gainst clotrimazole-resistant Malassezia furfur isolates was determined in the range of 1024 - 2 μL/mL by the broth microdilution method. The MIC of Aloe vera extract was obtained in 89% of clotrimazole-resistant Malassezia isolates at a concentration of 512 μL/mL and higher. In fact, only 11% of clotrimazole-resistant strains showed resistance to the extract, which indicates the satisfactory antimicrobial effect of Aloe vera extract. MFC values of Aloe vera extract for 86% of clotrimazole-resistant Malassezia isolates was determined at the concentration of 512 μg/mL and for 3% of clotrimazole-resistant isolates at the concentration of 1024 μL/mL, indicating the fungicidal properties of this extract at concentrations of 512 to 1024 μL/mL.
5. Discussion
One of the most important diseases associated with Malassezia is seborrheic dermatitis, which is of paramount importance in terms of appearance. The causative agents of these diseases do not involve the host’s immune system but the superficial skin areas, and are thus seen as a chronic problem in most cases (8).
In this study, 70.6% of the total samples collected from suspected cases of seborrheic dermatitis were reported to be positive for Malassezia species. This is while in a study, the frequency of yeast cells in all samples of patients with seborrheic dermatitis was reported to be 54% (9), which is less than the results of our study in this regard.
The results of this study showed that the frequency of Malassezia strains isolated from suspected cases of seborrheic dermatitis was higher in women (86%) than in men (14%), which could be due to differences in the secretion of sebum, and the type and amount of sex hormones. In a study, the highest frequency of Malassezia was observed in women (60%) (10), which is similar to the result of our study in this regard. However, the results of some reports indicated the higher risk of diseases associated with Malassezia in men than women (11).
The highest frequency of Malassezia was observed between the ages of 12 and 16 years old (41%). Also, the number of patients was higher among the ones who went to sleep between 12 and 1 AM (34%) than those who went to sleep between 9 and 10 PM (2%).
In another study, Malassezia species isolated from patients with seborrhoic dermatitis were more common in the age group of 20 - 29 years old (10), while in our study, Malassezia had the lowest frequency in the age group of 20 - 24 years old.
In the present study, Malassezia furfur was found to be the most prevalent in Malassezia strains by species, compared to Malassezia globosa and Malassezia restricta. However, in a study by Hedayati et al. (10), Malassezia globosa was found as the dominant species of Malassezia, followed by Malassezia furfur and Malassezia restricta. Nakabayashi et al. (11) reported that in patients with seborrheic dermatitis, Malassezia globosa and Malassezia furfur were the most frequent ones. In the present study, Malassezia furfur had the highest frequency in seborrheic dermatitis patients.
In a study by Klarostaghi et al. (12) that was conducted to see if Malassezia was present in acne lesions, only Malassezia furfur was found (2.5%). The geographical and climatic conditions of the area, the low prevalence of other species in the geographic region under study, and even the type of sampling technique could be the reasons for this finding.
In numerous studies, an increase in the number of Malassezia yeasts in dandruff and the association between the number of Malassezia yeasts and the severity of seborrheic dermatitis have been reported (4). In addition, it has been shown that treatment with antifungal agents such as clotrimazole heals lesions and reduces the number of Malassezia yeasts on the skin of patients with seborrheic dermatitis (13).
In a study by Yurayart et al. (14) more than 95% of Malassezia strains isolated from dogs with seborrhoic dermatitis were reported to be susceptible to clotrimazole. In another study by Khazaiyan et al. (15), 12.5% of Malassezia isolates were resistant to clotrimazole. This resistance was less than the one reported in our study. Resistance to antibiotics in different regions of Iran and the world can be as a result of genetic changes in the causative strains, differences in the amount of antibiotics used, and changes in the availability of new antibiotics.
Resistance to conventional antibiotics by bacteria is a global phenomenon that is encompassing all human pathogens and all antibiotic groups (16). Therefore, it is essential to carry out further studies to obtain antimicrobial agents from other sources such as plants. One of these plants is Aloe vera, whose extract is well known to have beneficial effects, but limited research has so far been conducted on its microbial effects. In this study, the antimicrobial effects of Aloe vera extract were shown to be more optimal than those of clotrimazole.
The results of the present study revealed a direct relationship between the diameter of the inhibition zone and Aloe vera extract concentration. This means that in all cases the diameter of the inhibition zone grows upon the increase in concentration, which is consistent with the study conducted by Mohebi et al. (17).
In the study of Sadrnia et al. (5) no inhibition zone was observed in all studied concentrations. However, in the present study, Aloe vera extract had inhibitory effect in all the studied concentrations. The difference in reported concentrations can be due to the difference in the applied extraction methods and the strains used in experiments.
In this study, the MIC and MFC values of the Aloe vera extract against the clotrimazole-resistant Malassezia isolates were determined in the ranges of 256 - 1024 μL/mL and 512 - 1024 μL/mL, respectively. The results indicated that 89% of clotrimazole-resistant strains showed susceptibility to the extract, which proves adequate antimicrobial effect of Aloe vera extract.
In a study by Kasim et al. (18), the results showed that 70% of Acalypha fimbriata aqueous and ethanolic extracts had the highest activity against pathogenic fungi, including Malassezia furfur. They also reported the MIC levels to be 50 mg/mL (18). Other studies carried out in Iran and other parts of the world also show that Aloe vera extract has antimicrobial activity (19).
4.1. Conclusions
The results of the present study showed that Aloe vera had satisfactory antimicrobial activity against clotrimazole-resistant Malassezia furfur isolates in vitro and that its antimicrobial activity increased upon increasing its concentration. Nevertheless, further studies seem to be needed in vivo to determine the effective dosage on fungi and ultimately to use Aloe vera to control chronic and inflammatory diseases. These results, along with further research in this field, can lead to the emergence of proper antifungal herbal remedies and reduce the use of synthetic antifungal drugs due to their toxicity and the side effects of these drugs.