1. Background
Visual impairment is one of the major health problems. The World Health Organization (WHO) report that there are more than 61 million people in the world with visual impairments, with 24 million having low visibility and 37 million being blind (1). The goal of the epidemiological studies of ocular diseases in different populations is to improve the ocular health for providing normal ocular conditions and prevent the decrease of vision quality due to visual impairments (2).
Some studies stated that refractive errors are a major reason for visual impairments that can occur at any age. It is also mentioned that 42% of people who suffer from visual impairments have uncorrected refractive errors (3-11). Refractive errors mainly myopia is one of the five main reasons for visual impairments in the world (12). It is appraised that myopia can affect one-third of the world's population by 2020 (13). Moreover, some studies explained that a significant percentage of low-vision populations are suffering from uncorrected refractive errors in developing countries (3, 14).
In general, the results of refractive errors evaluation in various populations show a great diversity according to age, gender, the method of measurement, and definition of refractive errors (15-24). For example, Matsumura and Hirai pointed out that myopia, which can affect some ages, is the commonest ocular disorder in Japan (22). In studies at Campo Grande University Hospital, between 1996 and 1998 in Brazil, it is described that hyperopia is the most frequent refractive error in children, varying between 60 and 70% (23). Smith et al. reported that refractive errors impose high costs on societies, and because they affect all age groups, they are the problems of all ages and societies (24). The second most populous country in the Middle East is Iran. According to some studies, the most refractive disorder in Iranian children is hyperopia (25-30).
One of the target populations for refractive errors investigation in previous studies has been the military population. Different evaluations on military individuals and army arrival volunteers have shown that myopia is more frequent than hyperopia in different parts of the world (31-35). The prevalence of hyperopia (19.6%) was less than that of myopia (37.7%) in Swedish military recruits (31). A study in Gilgit showed 43.33% of refractive errors belonged to myopia and 15% to hyperopia in young adults seeking recruitment in the army (32). In Ugandan soldiers, a higher prevalence rate for myopia was reported (33). Collins and Berg found that the prevalence of myopia is three times higher than that of hyperopia among military beneficiaries in the United States (34). Moreover, the prevalence rate of myopia and hyperopia among refractive errors was 75.8% and 11.7%, respectively, in the study of military service in Poland (35).
In Iran, we found no study on refractive errors in military persons. The screening of applicants for military service is not programmed, accurate, and regular in Iran. Since during the military service period, soldiers may carry out sensitive tasks that require the full health of the ocular system, such as shooting, driving, night patrol, working with electronic systems, etc., it seems necessary to perform an epidemiological revision in order to develop screening programs for the recognition and assessment of visual impairments. Therefore, in the current study, the prevalence of refractive errors was evaluated in Army Air Force soldiers of the Islamic Republic of Iran (IRI).
2. Methods
2.1. Study, Target Population, Sample Group, and Examinations
This cross-sectional study was performed between October 2017 and April 2018. The target population was the IRI Army Air Force soldiers who were selected through a convenience sampling.
A total of 500 men aged between 18 and 29 years (mean age 19.9 ± 1.6 years) were examined. The ocular examination included slit-lamp biomicroscopy, auto-refraction, subjective refraction, retinoscopy, uncorrected distance visual acuity (UCDVA), and best-corrected distance visual acuity (BCDVA) assessments. Informed consent was obtained from all individuals. UCDVA and BCDVA were measured with a six-meter logMar chart, refractive errors were determined by using a Topcon autorefractor RM-8900 (Topcon Corporation, Japan) without use of cycloplegics, and retinoscopy (Welch Allyn Elite™ Retinoscope, United States) was done when the subjects were fixed on a VA chart with a distance of six meters to relax accommodation.
The inclusion criteria were the employment at Military Service of the IRI Air Force, the absence of facial-head and ocular trauma, ocular pathology, systemic diseases, and ocular surgery in the case history while the exclusion criteria included the poor cooperation in subjective tests and malingering.
2.2. Data Analysis
Data for the right eye of each subject were used for all data analysis. The data acquired by the dry retinoscopy were used in the analysis and the refractive values were converted into the spherical equivalent (SE = sphere + (cylinder/2)). We categorized the SE values based on dry retinoscopy into four groups of emmetropia, myopia, hyperopia, and astigmatism. The myopic, hyperopic, and astigmatic subjects were further divided into three subgroups based on the magnitude of refractive errors (mild, moderate, and high).
A spherical equivalent of -0.50 diopter (D) or worse was construed as myopia and a spherical equivalent equal to + 0.50 D or worse was construed as hyperopia. The set cutoff values for myopia (-0.50 D or worse) and hyperopia (+ 0.50 D or worse) are common in the literature, especially in adults (31, 36-40). The spherical equivalent between -0.50 and + 0.50 was defined as emmetropia (absence of any refractive error). We classified myopia as mild (-0.50 D to -3.00 D), moderate (-3.10 D to -6.00 D), and high (worse than -6.00 D). Hyperopia was classified as mild (+ 0.50 D to + 2.00), moderate (+ 2.1 D to + 4.00 D), and high (worse than + 4.00 D).
The cylinder error ≥ 0.75 D was considered as astigmatism. Moreover, astigmatism was classified as mild (-0.75 D to -2.00 D), moderate (-2.10 D to -4.00 D), and high (worse than -4.00 D). If the axis of astigmatism was between 150° and 180° or between 0° and 30°, it was defined as with-the-rule (WTR) astigmatism, against-the-rule (ATR) astigmatism was defined when the axis of astigmatism was between 60° and 120°, and other was considered oblique astigmatism (36).
The normality of data distribution was tested by the Kolmogorov-Smirnov test. We used the Pearson coefficient of correlation to compare the right and left eye refractions. Proportion differences between two groups of education level were analyzed by the chi-square test. The prevalence of refractive errors was reported in percentages with 95% confidence intervals (CI). A P value of < 0.05 was contemplated as statistically significant.
3. Results
A total of 500 men, aged 18 - 29 years, were examined and included in the study. The mean age of the study subjects was 19.9 ± 1.6 years.
3.1. Distribution of Refractive Errors
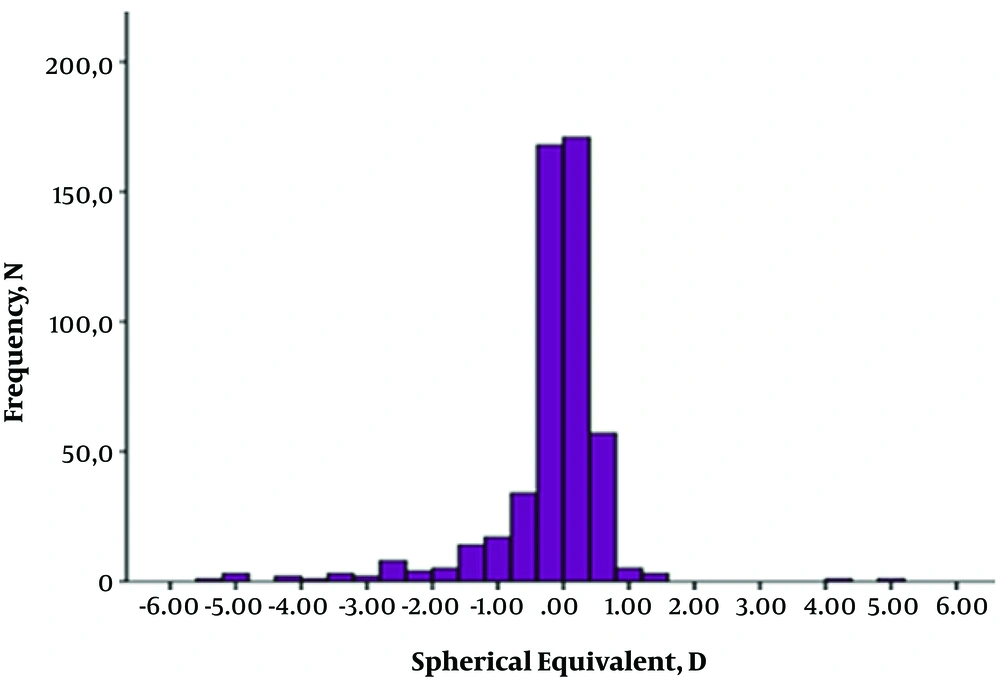
Myopia was found in 18.8% [95% confidence interval (CI): 15.5 - 22.5] and the distribution of hyperopia and astigmatism was 13.4% (95% CI: 10.5 - 16.7) and 20.8% (95% CI: 17.3 - 24.6), respectively. Emmetropia was seen in 67.8% (95% CI: 63.5 - 71.9) of the subjects. The mean SE refraction of myopia, hyperopia, and cylinder error for astigmatism was -1.5 ± 1.2, + 0.8 ± 0.7, and -1.2 ± 0.9, respectively. The characteristics of different types of refractive errors obtained with dry retinoscopy are presented in Table 1 and Figure 1.
| Refractive Status | N, Prevalence (%) (95% CI) |
|---|---|
| Emmetropia (-0.50 D < SE < 0.50 D) | 339, 67.8 (63.5 - 71.9) |
| Myopia (SE ≤ -0.50 D) | 94, 18.8 (15.5 - 22.5) |
| Hyperopia (SE ≥ + 0.50 D) | 67, 13.4 (10.5 - 16.7) |
| Astigmatism (cylinder ≤ -0.75 D) | 104, 20.8 (17.3 - 24.6) |
| Total | 500 / 100 |
a CI, confidence interval; D, diopter; N, number; SE, spherical equivalent.
The refractive status distribution in the study sample is shown in Figure 1, which shows the peak point of refractive status distribution for emmetropia.
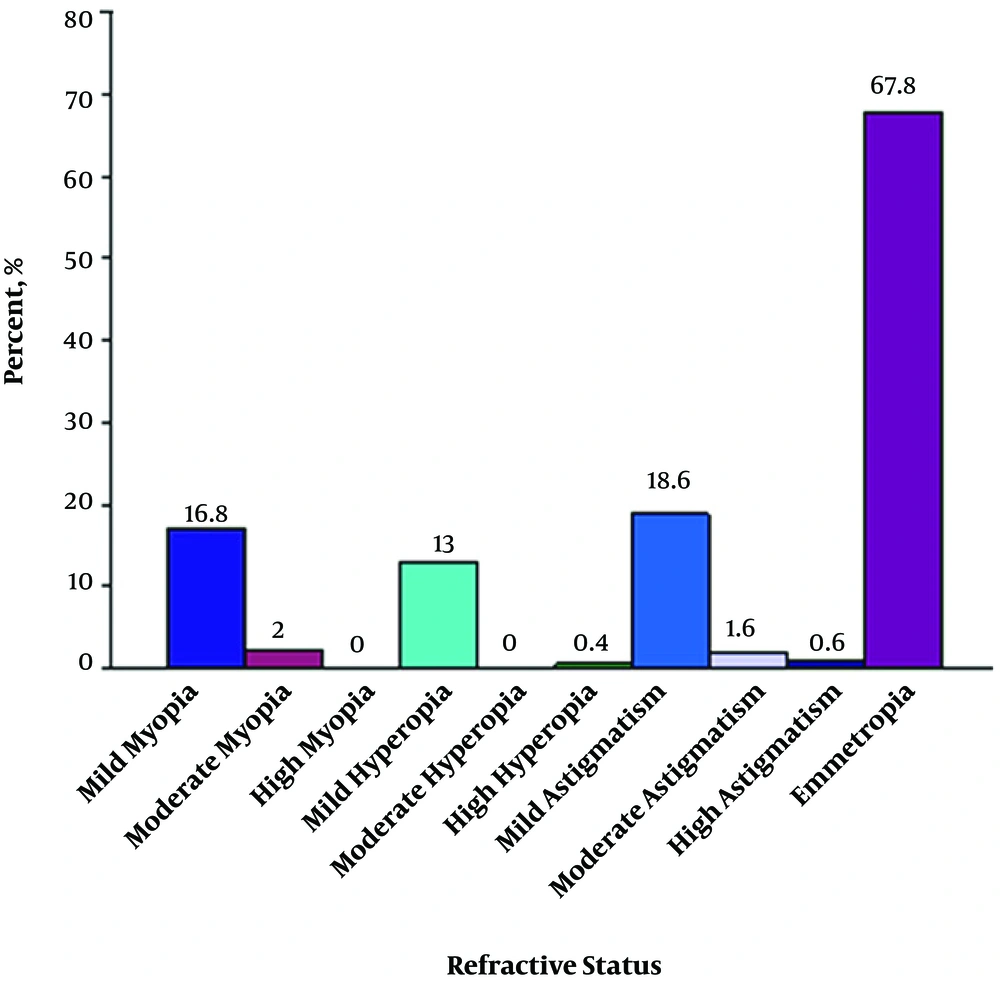
The prevalence of mild and moderate myopia was 16.8% (95% CI: 13.6 - 20.4) and 2% (95% CI: 1 - 3.6), respectively, and no eye with high myopia was found in our study group. Among 13.4% of hyperopic eyes, 13% (95% CI: 10.2 - 16.3) were related to mild and 0.4% (95% CI: 0 - 1.4) to high hyperopia and no eye with moderate hyperopia was found. The prevalence of mild, moderate, and high astigmatism was 18.6% (95% CI: 15.3 - 22.3), 1.6% (95% CI: 0.7 - 3.1), and 0.6% (95% CI: 0.1 - 1.7), respectively (Table 2).
| Refractive Errors | N, Prevalence (%) (95% CI) |
|---|---|
| Myopia | |
| Mild | 84, 16.8 (13.6 - 20.4) |
| Moderate | 10, 2 (1 - 3.6) |
| High | 0, 0 |
| Hyperopia | |
| Mild | 65,13 (10.2 - 16.3) |
| Moderate | 0, 0 |
| High | 2, 0.4 (0 - 1.4) |
| Astigmatism | |
| Mild | 93, 18.6 (15.3 - 22.3) |
| Moderate | 8, 1.6 (0.7 - 3.1) |
| High | 3, 0.6 (0.1 - 1.7) |
a CI, confidence interval; N, number.
The distribution of myopia, hyperopia, and astigmatism subgroups in our study is shown in Table 2. Mild astigmatism was the most prevalent refractive errors (18.6%) (95% CI: 15.3 - 22.3).
Table 3 shows a dominant trend for WTR astigmatism in astigmatic subjects (43.3%) (95% CI: 33.6 - 53.3), followed by oblique (29.8%) (95% CI: 21.2 - 39.6) and ATR astigmatism (26.9%) (95% CI: 18.7 - 36.5).
| Astigmatism/Type | N, Prevalence (%) (95% CI) |
|---|---|
| Based on axis | |
| WTR | 45, 43.3 (33.6 - 53.3) |
| ATR | 28, 26.9 (18.7 - 36.5) |
| Oblique | 31, 29.8 (21.2 - 39.6) |
| According to the focal point | |
| Simple | 51, 49 (39.1 - 59) |
| With myopia | 31, 29.8 (21.2 - 39.6) |
| With hyperopia | 22, 21.2 (13.8 - 30.3) |
a ATR, against-the-rule; CI, confidence interval; N, number; WTR, with-the-rule.
According to the focal point with reference to the retina, astigmatism was divided into three subgroups, simple astigmatism, with myopia, and with hyperopia. Simple astigmatism was more frequent (n = 51, 49%) (95% CI: 39.1 - 59) compared to the other groups of astigmatism (Table 3).
In addition, the study sample was divided into two groups, based on the education level. The group with a higher education level consisted of persons with bachelor degrees or higher and the other group consisted of persons with under-bachelor degrees. 116 out of 250 participants with bachelor degrees or higher and 108 out of 250 participants with under-bachelor degrees had refractive errors in their right eyes. There was no significant difference in the prevalence of all types of refractive errors between the two groups of education level (P = 0.472).
4. Discussion
As mentioned previously, some important tasks assigned to soldiers during military service require the complete health of the visual system. Therefore, the evaluation of visual impairments, especially refractive errors, in them can help better planning for maintaining their visual health and reduce injuries caused by these disorders. In this study, we evaluated the prevalence of refractive errors in Iranian Army Air Force soldiers among those who presented to Isfahan Shahid Babaee Hospital. The prevalence rate of myopia (SE ≤ -0.50 D) was 18.8%, hyperopia (SE ≥ + 0.50 D) was 13.4%, and astigmatism (cylinder power ≤ -0.75 D) was 20.8%. 67.8% of the participants were emmetrope.
However, the prevalence of refractive errors, especially myopia, in our study was lower than those reported in some previous studies (31, 36-40). One important explanation for these differences is our selected sample. It is difficult to compare our results with other population-based studies because subjects enrolled in the study were IRI Army Air Force soldiers that had been screened before dispatching to military service regarding their refractive status and they would be exempted if they had had refractive errors higher than a specified level.
The other possible cause of these differences is the emmetrope group in our study sample. We described refractive errors in four groups of emmetropia, myopia, hyperopia, and astigmatism while a few previous studies reported the prevalence rate among subjects with refractive errors (41-43). Regardless of emmetropia, 35.47% of the refractive errors were myopia (SE ≤ -0.50 D), 25.28% hyperopia (SE ≥ + 0.50 D), and 39.25% astigmatism in our investigation. These prevalence rates are comparable with the results of studies that did not consider emmetropia (41-43).
It is worth noting that in this study, it was not feasible to obtain cycloplegic refraction; therefore, accommodation might affect the measurements of refractive errors, particularly in this age group, despite the fixation to far target and fogging used to minimize and control the accommodation. It is clear that myopia is more prevalent than hyperopia in this study. This is in agreement with some other studies with the same age group, as mentioned in Table 4.
a Refractive errors considered as spherical equivalent (SE) < -0.50 diopter (D) for myopia and SE > + 0.50 D for hyperopia.
b Refractive errors considered as SE ≤ -0.50 D for myopia and SE ≥ + 0.50 D for hyperopia.
c Refractive errors considered as SE ≤ -0.50 D for myopia and SE > + 0.50 D for hyperopia.
Myopia had lower prevalence in our evaluation than in others mentioned in Table 4. On the contrary, except for the Sweden study, the prevalence of hyperopia was higher in our investigation. The non-cycloplegic method was used for the determination of refractive errors in all of these studies. We believe that using the fogging method to control accommodation is one important reason for the lower prevalence of myopia in our study. Another possible reason is that our sample population had been examined before dispatching to military service with the methods that focused on UCDVA/BCDVA, and it is likely that because of the greater impact of myopia than hyperopia on far VA, some myopic persons had been exempted from military service.
Moreover, it should be said that many studies have shown a relationship between age and increasing myopia (44-46). Optically, myopia and hyperopia are opposite to each other; thus, it is expected that hyperopia decreases with increasing myopia. The literature explains that one of the most important reasons for that is the growth-related increase of axial length. An increase in near activities including the use of computerized devices, high accommodative convergence/accommodation ratio, environmental factors, and high lag of accommodation are other reasons that have been considered in previous studies (47-49).
Hashemi et al. found that the prevalence of myopia increases to 30-years-old in adult rural populations in Iran (39). In another study, Hashemi et al. proved that the prevalence of hyperopia was higher in females, which is in line with most studies that have shown the higher prevalence of myopia in males (36). We expected that myopia would be more prevalent than hyperopia in our study.
Our assessments showed no significant difference in the prevalence of myopia between our two education groups. We think increasing endlessly in near work activities among all people in the community is the most important reason for this finding.
Regarding astigmatism, we should say that the most common refractive error in our study was astigmatism (Figure 2).
According to what has already been proven in some studies (50-52), the prevalence of astigmatism increases significantly with age, so it was expected that the astigmatism prevalence would be high in our study.
The prevalence of type and axis of astigmatism was also evaluated in our study group. WTR and simple astigmatism were found to be more frequent, which are in agreement with the findings of other studies (36, 53, 54). There are numerous reports that the prevalence of WTR astigmatism significantly decreases with age while ATR astigmatism significantly increases with aging. Fan et al. (55) and Gudmundsdottir et al. (56) in their studies explained that the reduction of eyelid tension with age causes the vertical corneal meridian to flatten, leading to increasing ATR astigmatism and decreasing WTR astigmatism. Nonetheless, ATR astigmatism was less prevalent in this study, in accordance with some study outcomes that pointed to the higher prevalence of ATR astigmatism after the fourth decade of the life (50, 51, 57, 58).
The limitations of the present study included the lack of cycloplegic refraction, limited range of age in the study group, and lack of history taking of near work activities that make it difficult to generalize the results.
4.1. Conclusions
In conclusion, the prevalence of refractive errors in Iranian Army Air Force soldiers is significantly high despite screening programs before military dispatch. Therefore, programmed, accurate, and regular screenings should be designed and executed for the detection of refractive errors among soldiers. Due to their visual activities during the military period, accurate optometric and ophthalmic examinations would be beneficial and useful.
However, the authors think that the large sample size selection from more barracks, sample selection of a wider range of age, reporting corrected and uncorrected refractive errors, investigation of binocular vision anomalies associated with refractive errors, and the use of cycloplegic refraction can be useful in future studies.