1. Background
One of the major health problems around the world is suicide (1). Suicide is currently considered as a major threat to public health around the world, and its major burden is imposed on countries with low and middle income levels. Death rate from suicide around the world in 2012 was estimated as 11.4% per 100 000 people (15% men and 8% women) and 2.5% in Iran (6.2% in men and 6.6% in women) (2, 3). In the recent years, suicide-related deaths have been on the rise. Suicide death rate is predicted to increase from 1.8% in 1998 to 2.4% in 2020 (4). It is one of the three main causes of death in the most active group and the second cause of death in the group of 15- to 19-year-olds (5, 6). Researches have shown that long-term emotional, physical, and sexual abuse during childhood leads to complications, such as personality disorders (7, 8), substance abuse (9), major depression (10), and suicide (11). Maltreatment of children is a widespread international problem and its consequences are different (12). Maltreatment of children is a general term used to describe all forms of child abuse, neglect, physical abuse, sexual abuse, and emotional abuse (13). One of the consequences of childhood trauma is the increased risk of committing suicide in adulthood (14). The relationship between childhood trauma and increased risk of suicidal behavior has been seen in both general and clinical populations. For example, a study (15) showed a strong association between sexual abuse during childhood and suicidal behavior in adulthood. Childhood traumas are associated with early suicidal actions (16). The first suicidal behavior at young age is seen to be accompanied by psychiatric illnesses, aggression, and violent behavior. The young age, at which suicide is attempted, is accompanied by repeated suicidal attempts (16). On the other hand, repeated suicidal attempts are associated with other self-harms. Swogger et al. (17) have shown that childhood trauma is not only a risk factor for suicidal behavior, yet also a risk factor for early suicide, psychiatric disorders, and aggressive traits. Although researches have shown a relationship between childhood trauma and suicide, there is still no specific mechanism to explain the relationship between childhood abuse and mental health problems during adulthood (18). Meanwhile, it seems that this relationship is mediated by psychological variables. One of these important variables is mental pain.
Mental pain is an unpleasant feeling (suffering) with a psychological or non-physical origin. Shneidman defined it as “how much you as a human being suffer pain”, which refers to mental suffering (19). Mental pain is an inevitable aspect of human being (20). An intolerable mental pain is a common cause of suicide (21). The causal relationship between mental pain and suicide has been raised by several researchers (19, 21). According to Shneidman’s theory, suicide does not only come about by exogenous factors, such as trauma, yet by intrinsic components, especially mental pain. More importantly, when a person’s risk of suicide is evaluated, one should consider the individual’s capacity for suffering pain. He suggested that suicidal behavior is better managed when mental pain is treated. Therefore, it seems that the mechanism of the effect of childhood abuses on suicide ideation is mental pain (19).
2. Objectives
Accordingly, the purpose of this research was to investigate the mediating role of mental pain in the relationship between trauma and suicide through the structural equation modeling approach (Figure 1).
3. Methods
The present research was fundamental in terms of purpose and descriptive-correlative in terms of data collection method. The statistical population of the research consisted of 196100 university students studying at different branches (Science and Researches campus, North, South, East, West and Center) of Islamic Azad University of Tehran in the academic year of 2017 - 2018. Using multistage cluster sampling, the participants were selected randomly from branches of Islamic Azad University of Tehran: Science and Researches Campus and Center Branch. Two or three classes of general education were selected randomly based on the number of each class from the faculties of humanities, basic sciences, and engineering of each branch. Given the large population size and that the number of acceptable samples for correlation research was 15 to 20 people for each sub-scale, and considering the structural equations and modeling that follow the rules of multiple regression analysis, 15 cases for each variable was a good rule (22); according to the number of variables under study, 14 variables (five types of trauma, eight subscales of mental pain, and one suicidal ideation), and considering 25 subjects for each variable, the number of sample was 371 individuals. The research was conducted on the sample group in accordance with the rules of the ethical committee of Islamic Azad University, Karaj Branch.
The participants with health problems that may interact with the results (having medical issues, such as depression, hyperthyroidism or taking any medication for sleep) were excluded from this study. The participating students were informed about the aim of the study and the methods that were to be used (ethical considerations). The research tools were as follows:
3.1. Childhood Trauma Questionnaire
The childhood trauma questionnaire (CTQ) was used to measure childhood traumas. This questionnaire was designed by Bernstein et al. (23) with 70 items in 1994, and in 1995, the second version was presented with 53 items. In 1998, further scale development led to the current 28-item version of the CTQ, which is sometimes referred to as the CTQ-SF. After reading each question, the subject chooses the number that best describes him. Each of the questions were classified in five levels (never, rarely, sometimes, often, and always). The questionnaire measures abusive behavior in five subscales, including physical abuse, emotional abuse, physical neglect, emotional neglect, and sexual abuse, and it ultimately gives an overall abuse score. This questionnaire has a relatively high validity and reliability. Bernstein et al. (23) reported the reliability of different factors of CTQ by two methods of re-testing and Cronbach’s alpha to be between 0.79 and 0.94. In the current research, Cronbach’s alpha coefficient was used to estimate the coefficient of reliability of CTQ. The results showed that the coefficient of reliability of the entire test was 0.85 and the reliability coefficient of the subscales was between 0.80 and 0.94. These coefficients reflect the high reliability of the CTQ.
3.2. The Orbach and Mikulincer Mental Pain Scale
The mental pain scale of Orbach et al. (24) has 40 items, which measure both the current mental pain and the worst mental pain ever experienced by an individual. Subjects respond to a five-point Likert scale from one (I completely disagree) to five (I completely agree); high scores highlight more painful experiences. This scale has eight factors, including: (1) irreversibility, (2) loss of control, (3) narcissist wounds, (4) emotional flooding, (5) freezing, (6) self-estrangement, (7) confusion, and (8) emptiness. Orbach et al. (24) initially constructed a nine-factor scale of 44 items, which, in addition to the eight factors mentioned, included a social distance factor with four items. In the initial study, the Cronbach’s alpha coefficient for the nine factors was between 0.78 and 0.94. Nine factors of mental pain scale were related to depression and anxiety scales in the expected direction. The correlation coefficient between the factors of mental pain and depression scale was between 0.26 and 0.64, and between its factors and anxiety, it was between 0.27 and 0.50. This moderate and meaningful relationship with the scales of depression and anxiety showed a distinctive validity for this scale. The social distance factor was omitted from the scale due to contradictory validity and eight factors remained (25). In another study, Orbach et al. (26) presented an alpha coefficient of 0.82 to 0.94 for mental pain subscales. In the current research, Cronbach’s alpha coefficient was used to measure the reliability of the Orbach and Mikulincer mental pain questionnaire (OMMP). The results showed that the coefficient of reliability of the entire test was 0.98 and the reliability of the subscales was between 0.78 and 0.95, indicating the high reliability of the questionnaire.
3.3. Beck Suicide Scale of Ideation
Beck suicide scale of ideation (BSSI) was developed by Beck (1979) to measure the individual’s aptitude for suicide. This scale provides a numerical estimate of the intensity of ideation and suicidal inclinations and consists of 19 items that are graded on a three-point scale from zero (lowest severity) to two (highest intensity). Validity and reliability of this scale have been confirmed in various researches. In Danitz’s research (27), the Cronbach alpha of this scale was 0.89. Also, the simultaneous validity of the test was reported with the suicide risk measurement scale to be 0.69 (28). In Iran, Anisi et al. (29) reported the reliability of the test using Cronbach’s alpha to be equal to 0.95 and 0.75 with the splitting method. In this research, the simultaneous validity of this scale was reported to be 0.76 with the depression scale of the general health questionnaire (GHQ).
4. Results
The sample consisted of 73 men (19.7%) and 298 women (80.3%). The average age of participants was 23.26 years with a standard deviation of 3.19 years. In Table 1, the correlation matrix between the hidden variables, and mean and standard deviation of the research variables has been shown. As the contents of this table indicate, all correlations included a considerable value (0.637 ≤ r ≤ 0.83).
| Chi-Square | TLI | RFI | RMSEA | SRMR | IFI | CFI | NFI | |
|---|---|---|---|---|---|---|---|---|
| Measurement model | 1093.62 | 0.94 | 1.698 | 0.13 | 0.072 | 0.95 | 0.95 | 0.95 |
| Structural model | 651.51 | 0.95 | 0.94 | 0.132 | 0.062 | 0.96 | 0.96 | 0.95 |
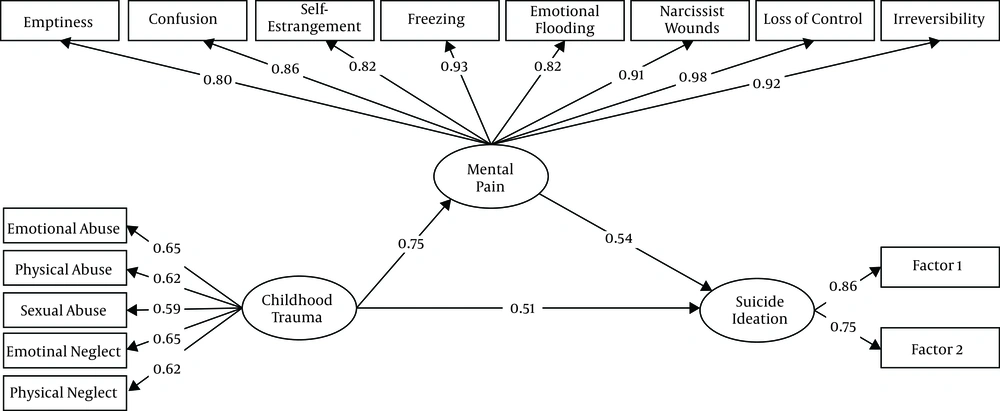
The structural model evaluation by using the structural equation modeling method showed that all the fit indices of this hypothetical model, other than RMSEA, were in the desired fit range. The fitness indices for this model are shown in Table 2. Figure 2 depicts the conceptual structural model along with the standard coefficients. Trauma as an exogenous variable, with the coefficients of 0.75 (t values = 14.31) and 0.51 (t values = 7.89) influences mental pain and suicide ideation. Mental pain also influences suicide ideation with a standard coefficient of 0.54 (t values = 8.94). In the structural model the significance of the path coefficient was determined using the t value. If the value of t is more than 1.96, the relationship between the two structures is significant, thus all the paths are significant.
In this study, the researchers used Bootstrap test to evaluate the mediating relationships.
| Values | |
|---|---|
| Independent variable | Childhood trauma |
| Mediating variable | Mental pain |
| Dependent variable | Suicide ideation |
| Bootstrap limits | |
| High | 0.506 |
| Low | 0.305 |
| Estimation error | 0.051 |
| Effect size | 0.407 |
| Significance level | 0.001 |
5. Discussion
The purpose of this study was to investigate the mediating role of mental pain in the relationship between childhood trauma and suicide ideation. Before evaluating the model of measurement and structural model, important assumptions about the structural equation modeling, including univariate and multivariate normality, and lack of multiple co-linearity were investigated. Calculation of the kurtosis of each of the evident variables is a common method for evaluating univariate normality. In this study, the skewness of the observed variables were in the range of 0.214 to 2.572 and their kurtosis was in the range of -0.889 to 7.531. Chou and Bentler (30) considered the cutting point of ± 3 for the proper skewness value. Although there is little agreement on the cutting point of kurtosis, however, in general, values greater than ± 10 are problematic for this index and values greater than ± 20 invalidate the obtained results (31). The values obtained for skewness and kurtosis of variables indicate the default fulfilment of univariate normality.
In this study, the assumption of multivariate normality was investigated by calculating the relative multivariate kurtosis index, whose value is equal to 1.291. Bentler (32) believes that if the value of this index is not more than three, then multivariate normality has been achieved. Therefore, the distribution of all combinations of variables is normal. The default study of the absence of multicollinearity was performed by checking the correlation matrix between the evident variables. An examination of this matrix indicates that there is no multicollinearity between them. Correlation coefficients are in the range of 0.637 ≤ r ≤ 0.803. Correlation coefficients above 0.85 make difficulty in the correct estimate of the model (31). In such situation, one of two variables should be left out of the analysis. Therefore, the assumption of the absence of a multicollinearity has also been realized. Structural equation modeling by using the maximum likelihood estimation method was used to evaluate the model of measurement and structural model. The model for measuring determines the relationship between evident variables and hidden variables. The evaluation of this model is done using the confirmatory factor analysis method. The fit indices of the measurement model given in Table 2 show the desired fit of this model. Therefore, the evident variables are capable of making operational the hidden variables. When the number of samples is not very high, Bootstrap provides the most powerful and logical way for achieving indirect effects (33). In this method, if the upper and lower limit of this test is either positive or negative, and zero is not placed between these two limits, then the indirect causal path will be significant. Table 3 represents the results of this test. In the hypothetical model, indirect effects have been considered for the trauma variable, and the direct effects for mental pain. As Table 3 indicates the trauma path to suicide ideation has become significant by mediation of mental pain with the standard coefficient of 0.407 at the level of P < 0.001. In other words, a unit of change in its standard deviation will make the standard deviation of suicide change by about 0.407 unit. Structural relationships between the variables of the study show a good fit of the hypothetic model. The findings of this research are in line with previous researches (11, 15-17). In explaining this finding, it can be said that since emotional abuse leads to depression and depression disorder have a high correlation with suicide, it can be argued that those, who are exposed to emotional abuse in childhood suffer from emotional disorders, such as depression and depression can lead to suicide (34). Evidence suggests that childhood traumas have a devastating effect on the growing brain of children and adolescents. One of these effects is emotional disorders. Abuse and neglect during childhood may lead to chronic disability in confronting the fluctuation of emotions and thereby increased emotional disorders, including depression (11). Emotional abuse can affect people’s cognition, in the form of distortions and cognitive errors, and these cognitive distortions ultimately lead to depression, whose greatest consequence is suicide. A research has shown that the intensity of emotional and physical abuse during childhood is related to the number of suicide attempts (34). Another research by studying 281 suicidal attempts showed that those, who have a history of suicide attempt have a higher CTQ score than those, who did not have suicide attempts. Therefore, in both groups of males and females, childhood trauma has a risk factor for suicidal aptitude (16).
In explaining this finding, it could be said that people with a history of stress experience a lot of negative emotions that prevent thinking and decision-making to solve their problems. The lack of practical and constructive measures will make the reminding stimuli of stressful events be continued, or exacerbate it in various factors (such as blaming and blaming oneself); it ultimately makes the individual feel helpless and imagine that he/she has no control over the situation, their life becomes absurd and irrelevant, and these intensify their thoughts on suicide. In one study, it has been emphasized that exposure to violence or trauma may increase depression and also affect the ability to deal with stress, thus resulting in suicidal thoughts and suicide attempts (35); as a result, the use of maladaptive strategies causes the individual to be anxious and, consequently, respond to stressful events anxiously instead of responding appropriately, thus, making individuals susceptible to suicide ideation (36).
Shneidman suggested that mental pain is placed at the heart of suicidal processes from suicide ideation to suicide. Intolerable mental pain has been reported to be the most common cause of suicide (21). The meta-analysis conducted by Ducasse et al. (37) showed that the level of mental pain in those, who commit suicide is greater than those, who do not; also, it is higher in those, who have suicide ideation than those, who have no idea about suicide. Interestingly, these results were meaningful even when subgroups had the same level of depression. This conclusion is consistent with the finding that the risk of suicide apart from depression is positively correlated with mental pain level (38). Mental pain also interacts with environmental factors in suicidal excitement. For example, the level of suicidal action and mental pain is higher in those, who were at risk of suicide by their family members than those, who did not have such an experience. These results suggest that mental pain increases the risk of suicide in dealing with stressful events in suicidal individuals. Therefore, in general, it can be said that life-threatening events increase the risk of suicide through psychological and emotional pain they cause (39).
5.1. Conclusions
Generally speaking, the findings of this research indicate that life-threatening events, although they have a central structure and a major role in committing suicide, the mechanism of this effect is mental pain.
5.2. Limitations and Suggestions
Although the findings support the hypothetical model of research, the results of this research should be interpreted with regards to its constraints. First, the current study was conducted on students with a fairly homogeneous population; therefore, in generalizing the results to other populations, caution must be taken. On the other hand, although many researchers support the conceptualization of mental disorders in a dimensional structure and believe that the results of clinical and non-clinical environments are greatly of coherence; caution should be taken in generalizing the results of this study to the clinical environment. Another limitation is that the cross-sectional nature of the present study prevents causal inferences and accurate knowledge of the true nature of the relationships between research variables. It is very probable that the order of the formation of variables is based on the hypothetical model; however, it is certainly not possible to reject other alternative states based on this study. Finally, in order to evaluate each of the variables, only one tool of self-measurement was used. Using a variety of measurement methods can help better conceptualize the variable.
Given the research constraints, it is recommended that the present study should be conducted on a clinical population or non-undergraduate population in order to enhance the generalizability of its findings. Longitudinal studies are also suggested to infer causal relationships and to clarify the sequence of time between research variables.