1. Background
Visible changes in the scapular position and motion patterns are called SD. This condition is associated with pain and pathology which can be characterized by the prominence of the medial border or the inferior angle of the scapula relative to the chest in a static or dynamic state (1). These changes can lead to shoulder dysfunction, increased acromioclavicular compression, subacromial space decrease and alterations in muscle activity. All these actions jump-start the symptoms. In spite of these problems and weaknesses in the scapula, the strength of the rotator cuff muscles decreases and the pressure in the G-H anterior ligaments increases (2). Scapular dyskinesis is seen in 61% of overhead and 33% of non-overhead athletes (3) as well as 67% - 100% of athletes with a shoulder injury or no symptoms (4).
Scapular dyskinesis can be seen in the shoulder of most overhead athletes who have excessive pain syndrome and may be resultant from the inhibition of activating patterns of the scapular stabilizers (4). Throwing overhead or similar activities such as swimming, incur a heavy load to the shoulder joint and tissues. The term “swimmer’s shoulder” is known to many swimmers. It involves a range of sequential or simultaneous injuries (5). Bak divided the swimmer’s shoulders into five main groups and stated that in four types, there is almost always SD (5). The prevalence and related complications to this are a significant issue. During the activity, the involved scapula is in abduction, protrusion, and lateral displacement compared to the uncomplicated scapula (6). In this condition, the probability of external and internal impingement is higher (6).
The swimmers might start their intense training at a young age, which can be very high in volume. A swimmer over the age of 13 typically performs between half to one million hand-cycles per year (7, 8). High-volume exercise during the growth periods may cause changes in the flexibility and stiffness of the tissue surrounding the shoulder and trunk, which makes the swimmer susceptible to shoulder pain. Also, multiple repeats affect the strength and flexibility of the core region (9). High velocities and high range of motion, put a lot of pressure and force onto their articulation, and tissue; therefore, high arthrokinematic accuracy is required for adequate performance and minimizing risk of injury.
One of the critical factors in G-H arthrokinematic is the optimal rotation of G-H (10, 11). The amount of G-H rotation depends on forces and loads applied to the shoulder. Although natural G-H arthrokinematic can change by inappropriate adaptation, it can change rotation and may predispose an athlete to injury (2). The GIR reduction in overhead athletes is a common occurrence due to the G-H arthrokinematics changes. It causes a shift in the humeral head center of rotation to an anterosuperior position on the glenoid during forwarding flexion (11). The GIR deficit can cause changes in the scapular biomechanics or kinematic changes of the G-H joint, which in turn leads to labral injury (2). The superior glenoid labral tear and the G-H joint instability are some of the causes of SD (9). It seems that due to SD, the relationship between a couple of forces is unbalanced. As a result, an excessive internal rotation (IR) exists for the individual so that we see an increase in the upper trapezius activity and also a decrease in the serratus anterior activity. Because of the unstable scapula, the length-tension relationship of the internal rotator muscles is out of balance. Hence, during IR, more force comes from the origin (the site of the scapula), which leads to a decrease in IR.
Soft tissue is thought to interfere with pathophysiology of the GIR disorders; therefore, the intervention can focus on soft tissue including muscle stiffness, non-flexibility, muscle weakness and capsular stiffness (2). As an example, by using active shoulder stretching exercises, the tightness of the posterior capsule can improve. According to some studies, the most common swimmer’s shoulder pain is associated with the rotator cuff muscles (1, 12). Although the study by the Sauers et al. investigated the passive shoulder stretching in baseball players (13). Kuhn confirmed that a shoulder intervention program must focus on strengthening of the rotator cuff and periscapular muscles, joint mobilization, and posterior capsule stretching (14). Moura et al. have indicated that amateur athletes with clinical evidence of subacromial pain syndrome associated with SD, respond well to a rehabilitation program. The program was emphasizing scapular control, upper trapezius relaxation, correction of muscular imbalance, and sensory-motor training (15).
2. Objectives
Most abnormalities in the scapula’s movement or positioning may be corrected with the intervention of the leading cause (14) like in SD. Rarely, surgical treatment is performed on the scapula, and the focus is usually on the source of the problem (9). Scapular dyskinesis is a common problem in elite swimmers, although according to our knowledge, no research has yet shown the effectiveness of corrective exercises on female athletes. Therefore, this study aimed to evaluate the effect of the 6-week selected corrective exercises in a clearly defined population of overhead athletes with SD symptoms. It was hypothesized that after this exercise program, all subjects would experience improved GIR.
3. Methods
3.1. Participants
Thirty-eight female attendees of the National Swimming Champions Competition (11 - 15 years old) were selected through the available sampling method. All participants provided a written consent form before sampling. The demographic information of the individuals was recorded in the individual information form. The test results were published without names and identities, providing the principle of trust in the writing of the article.
Having at least two years of regular swimming activity was the inclusion criteria. Considered exclusion criteria were: pain or history of injury in each shoulder bone and/or complete rupture of shoulder muscles during the last two years; the frequent practice of physical activity in any other sport; and the negative result of the SD diagnosis test (16). The subjects were divided into two experimental (n = 19) and control (n = 19) groups according to demographic characteristics and their first swimming stroke. The sampling method was calculated using the formula shown below:
Three individuals were excluded from the study due to the lack of cooperation in doing exercises from the program. Overall, 35 swimmers participated in this study.
3.2. Testing Procedure
3.2.1. Diagnosis of Scapular Dyskinesia
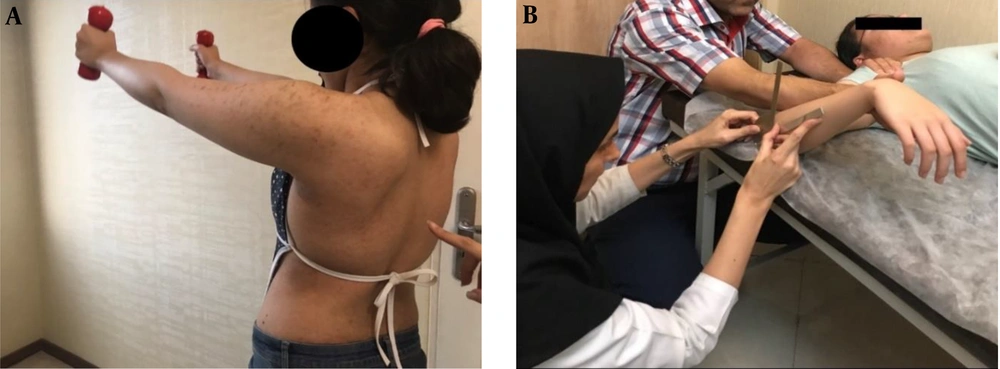
To diagnose the three-dimensional scapular movement, the subjects performed the dynamic tasks of the upper limb in both the elevation (concentric) and depression (eccentric) levels. When observing the winging or altered rhythm of the scapula unilaterally or bilaterally, the test results were “positive” in the sense that there are signs of scapular dyskinesis (16). This observational method has good validity and inter-rater reliability, as shown in previous studies (16, 17) (Figure 1).
3.2.2. GIR Measurement
The athlete was asked to lie supine and the examiner positioned the shoulder into 90° of abduction and 90° of elbow flexion with the arm in neutral rotation. Palpation of the coracoid process was used to judge the scapular movement. The examiner moved the arm into IR until the capsular end feel was achieved, scapular movement occurred, or the participant complained of pain (2, 18) (Figure 1). Test-retest reliability of this method is reported to be 0.92 (2).
GIR pre-test was measured one day before the first training session, and post-test one day after the last training session.
3.3. Exercise Program
The protocol was Moura et al.’s moderated training program (2016) (19) (Table 1), comprised of six weeks and three sessions a week, with moderate intensity. These exercises emphasized on improving the imbalance between upper trapezius and serratus anterior, lower and middle trapezius muscles. Activity intensity was monitored using the Borg scale and OMNI-resistance exercise scale (20, 21). The Borg scale is a numerical scale that ranges from 6 to 20, where 6 means “no exertion at all” and 20 means “maximal exertion”. When measured, a number is chosen from the following scale by an individual that best describes their level of exertion during physical activity; and according to OMNI-resistance exercise scale, by increasing the separation between the hands gripping the elastic band, the intensity decreases. The training program included three parts: scapular stability, stability-strengthening, and strengthening.
| Phase 1 (week 1 & 2) | Phase 2 (week 3 & 4) | Phase 3 (week 5 & 6) |
|---|---|---|
| Sleeper stretch (60°, 90°, 120°) | Sleeper stretch (60°, 90°, 120°) | |
| Sitting, arms in neutral position, pull their shoulder blades back and down | Punch with dumbbells | Standard push-up plus with the Swiss ball |
| Punch exercise | One-hand push-up plus exercise | Modified prone Cobra on Swiss ball with dumbbells |
| Wall push-up plus exercise | Modified prone Cobra with dumbbells | Prone horizontal abduction exercise on the Swiss ball with dumbbells |
| Modified prone Cobra | Prone horizontal abduction exercise | Prone V-raise exercise on the Swiss ball with dumbbells |
| Prone V-raise exercise | Low row exercise with TheraBand | |
| Prone row | Rotator cuff exercise with TheraBand | |
| Rotator cuff exercise |
3.4. Statistical Analysis
After ensuring the assumption of the normality, the data distribution and the equality of variance with two tests; Paired-sample t-test (IR) and co-variance (between groups) were used to compare within and between groups. Analysis was performed with IBM SPSS statistics version 19.0. Significance level was considered less than 0.05.
4. Results
The participants’ demographic details are presented in Table 2. The assumption of normality was determined using the Shapiro-Wilk test. In terms of age, height, weight, BMI, and the first swimming stroke, Independent t-tests revealed no significant differences between the control and experimental groups. It suggested that the two groups had similar demographic backgrounds.
| Variable | Experimental Group | Control Group | P Value |
|---|---|---|---|
| Age (y) | 12.8 ± 1.06 | 13.37 ± 1.14 | 0.67 |
| Height (cm) | 159.05 ± 6.32 | 161.25 ± 6.23 | 0.92 |
| Weight (kg) | 53.05 ± 6.31 | 54.62 ± 4.88 | 0.10 |
| BMI (kg/m2) | 20.92 ± 1.70 | 20.99 ± 1.26 | 0.15 |
Abbreviation: BMI, body mass index.
aValues are expressed as mean ± SD and analyzed by the Shapiro-Wilk test.
Chi-squared test was used for comparing the first swimming stroke between two groups. Assumption of homogeneity of variance was tested using the Mauchly sphericity test. The results show that there were no significant differences between the swimmers of the two groups (Table 3).
| Swimming | Experimental Group | Control Group | P Value |
|---|---|---|---|
| Crawl | 5 (26.3) | 5 (31.25) | 0.95 |
| Breaststroke | 5 (26.3) | 4 (25.0) | |
| Backstroke | 4 (21.1) | 4 (25.0) | |
| Butterfly | 5 (26.3) | 3 (18.75) |
aData are expressed as number (%) and analyzed by χ2 test.
Table 4 presents the pre- and post-mean, SEM and the changes values of the GIR between the two groups. The GIR diminished significantly after six weeks of selected corrective exercises in the experimental group (P = 0.001), whereas there was no significant increase in the control group (P = 0.722). The changes are in the exercise group (8.37 ± 0.76) and control group (-0.19 ± 0.44) and the test shows significant differences between the two groups (P < 0.001).
| GIR | Experimental Group | Control Group | P Value |
|---|---|---|---|
| Pre-test | 38.05 ± 1.38 | 38.75 ± 1.33 | 0.722 |
| Post-test | 46.42 ± 1.59 | 38.56 ± 1.42 | 0.001* |
| Changes | 8.37 ± 0.76 | -0.19 ± 0.44 | < 0.001* |
aValues are expressed as mean ± SEM and analyzed by swimmer’s GIR t-test.
5. Discussion
The present study aims to investigate the effects of a six-week stretch and stability-strength training program on GIR of swimmers with SD. The findings indicated that these exercises would improve and increase the shoulder IR by reduction of posterior capsule stiffness and amending muscle imbalance in the shoulders of these competitive swimmers.
As mentioned earlier, an abnormal scapular motion was commonly observed in competitive overhead athletes. This finding is associated with excessive joint distraction force that may contribute to the posterior structural change, and induce adverse effects on GIR (6). Conservative interventions, including the use of exercise, can be effective at different shoulder positions, symptoms of pain, range of motion and functional disability (22). However, SD occurs when the coordination of the scapular movement over the chest changes; it leads to overload on the G-H joint and muscles, which can cause pain and movement limitation (23). Kibler has described the intervention should focus on removing the muscle imbalance, especially the periscapular muscles. Besides, developing muscle balance, elongation of the posteroinferior capsule and the pectoralis minor muscle are needed (1). Furthermore, the study by the Sauers et al. suggested the dominant shoulder display significantly increases in G-H and shoulder complex IR and ER ROM and significantly decreases posterior shoulder tightness followed by stretching (13). Smith et al. affirmed that retracted scapula is a base of support for rotator cuff muscles (24). For such reasoning, scapular protraction must control or correct with reduced force-generating capabilities for the IR and external rotation (ER) (25).
Together with our results, Batalha et al. reported that the horizontal adduction stretch reduced posterior shoulder tightness on post-surgical subjects (26).
Brownstein reported that both stretching methods (dynamic mobility and passive stretching) increase the total range of motion (TROM) by an average of about 20 degrees. However, the dynamic mobility group had a more significant increase in ER than IR, and the passive stretching group had a more substantial increase in IR than ER (27). Moseley et al. (28) and Townsend et al. (29) used selected rehabilitation exercises such as the prone horizontal abduction with ER exercise as a strengthening exercise for G-H and scapulothoracic. These results agree with the findings of Cools et al., who suggested that these exercises can improve low UT/SA and UT/MT ratios (30).
Higson et al. showed that high-level swimming exercises had no effect on GIR ROM but could reduce ER in elite swimmers (19); Therefore, improving the GIR followed by the exercise protocol of this study can improve the SD in adolescent swimmers. These findings corroborated our study policy, which agrees with using dry land exercises along with swimmers training.
Although, when comparing our results with others, it must be taken into account that various studies investigated the effect of different exercises, in a distinct study population, under different training modalities, and with varying measures of outcome, making it difficult to interpret the results of our study in relation to previous research on this topic.
Finally, it seems that a 6-week selected corrective exercise program can cause a significant improvement in reduced GIR in young competitive female swimmers; however, our results suggest that further studies are required to evaluate the effects of this training on male swimmers.
5.1. Conclusions
According to the findings of the present study, it seems that the targeted corrective exercises can enhance decreased GIR in female adolescent swimmers with SD by stabilizing the scapula and improving muscle imbalance. Therefore, it is suggested that overhead athletes such as swimmers, use this protocol in their dryland exercise program.