1. Background
Severe acute respiratory coronavirus-2 (SARS-CoV-2) was first officially reported in Wuhan (China) in December 2019 and in three months turned into a pandemic by the announcement of the general director of the World Health Organization (WHO). While global attention is focused chiefly on its physical health consequences, the impact of COVID-19 on psychological health cannot be overlooked (1). In Nigeria, the first coronavirus case was confirmed on February 27, 2020. Since then, the Nigerian authorities have taken some measures to stop its spread. However, controlling the spread of the dreaded COVID-19 in Nigeria is an arduous task (2). By April 2020, the confirmed active case of COVID-19 in Nigeria was 1,932, with 58 deaths (3). By February 19, 2021, confirmed cases reached 150,246, and 1,803 lives were lost. As of June 6, 2021, 166,767 COVID-19 cases and 2117 deaths were reported (4). The number of confirmed COVID-19 cases was following a steady growing trend. For instance, in June 2020, the WHO noted that about 800 Nigerian Health Care Workers (HCWs) are died due to COVID-19 infection (5). By September 2020, the number of infections among HCWs reached 2,175 (6). When dealing with infectious diseases, fear of getting infected is prevalent, which in turn paves the way for increased rates of transmission, medium, morbidity, and mortality, as is seen with SARS-CoV-2 (4, 5).
High infection rates among HCWs may result in psychosocial consequences such as stigmatization, discrimination, loss, depression, and anxiety (7). In addition, it should be noted that in situations with widespread fear, people may lose their ability to think clearly or rationally (8). In a systematic review on the prevalence of COVID-19 among HCWs and its-related death in 195 countries, Bandyopadhyay et al. (9) found a total of 152,888 infections and 1413 deaths. Regarding the high rates of COVID-19 infection and its high mortality rate among HCWs, it is not surprising for them to worry about vulnerability to the virus. Fear of interacting with suspected COVID-19 infected cases has also been reported (10). The emergence of the COVID-19 has caused a great fear worldwide (11), with pockets of associated stigma and marginalization of confirmed patients, survivors and their families stigmatization, and social exclusion of confirmed patients, survivors, and their families (12, 13).
According to Ahorsu et al. (8), fear of coronavirus disease may result in irrational and unclear thoughts. So that Mamun and Griffiths (14) proposed an urgent need for studies on possible COVID-19 prevention strategies to forestall severe psychopathological symptoms such as suicidal ideation and attempts caused by the fear of COVID-19. Fueling the perceived vulnerability to COVID-19, especially among HCWs in Nigeria, might be due to inadequate funding of the Nigerian healthcare system and associated poor work environment (15). In addition, there are also other important issues such as the attendant lack of material, including personal protective equipment (PPE), low staff strength, and the high infection rates associated with lack of or inappropriate use of equipment (16-18), and the degree to which individuals feel susceptible to infectious diseases. The diagnostic and therapeutic aspects of COVID-19 have been highlighted by researchers all over the world; however, few studies have investigated its psychological consequences (14, 19, 20). As the frontline staff, the mental health of HCWs is germane if humanity is to win the fight against COVID-19. Based on what was mentioned before, the current study aimed to firstly assess the severity of anxiety and depression and perceived vulnerability to diseases and secondly to investigate their association with the fear of COVID-19 among Nigerian HCWs.
2. Methods
This study was carried out on Nigerian HCWs aged 21 to 60 years old working at the Federal Neuropsychiatric Hospital and University of Benin Teaching Hospital (UBTH) in Benin-City, Edo State, South-South of Nigeria. The research purpose and methodology were subjected to scrutiny by the Internal Research Ethics Committee of Redeemer's University, Ede, Osun State, and was given due approval. Also, the ethical guidelines and approval of the Federal Neuropsychiatric Hospital, Benin, and the UBTH were duly obtained before the commencement of the study. Participation in this survey was voluntary, and no incentive was offered to participants. Informed consent was obtained from each participant. Using a purposive random sampling method a total of 550 questionnaires were distributed to HCWs who consented to participate in the study, in which 418 were returned. Five questionnaires were removed due to incomplete responses. Eventually, data of 413 questionnaires were entered the final analysis, given a response rate of 75.1%.
All HCWs at the Federal Neuropsychiatric Hospital, Benin, and the mental health, and obstetrics, and gynecology departments of the UBTH who consented to participate in this study were recruited. All those who declined to participate and were on leave at the time of data collection, were excluded from the study.
The Fear of COVID-19 Scale, the Hospital Anxiety and Depression Scale (HADS), and the Perceived Vulnerability to Disease Scale (PVDS) were used for data collection. The unidimensional Fear of COVID-19 Scale contains seven items scored on a 5-point Likert scale (8). The scale has an acceptable internal consistency (α = 0.82 and ICC = 0.72). The Fear of COVID-19 Scale has a significant validity coefficient when correlated with PVDS and HADS (8). The test-retest analysis of the Fear of COVID-19 scale on the Nigerian sample showed a good internal consistency (r = 0.76, P = 0.000) and a Cronbach's alpha of 0.85. The Hospital Anxiety and Depression Scale (HADS) (21) is developed to measure anxiety and depression in hospital settings and on medical outpatients. The 14-item HADS is scored on a 4-point Likert scale. The higher the score, the more severe the anxiety or depression. The scale has Cronbach's α of 0.78 and 0.86 for the dimensions of anxiety and depression, respectively, and it has been validated with Nigerian samples (22).
The PVDS (23) is a 15-item instrument with two dimensions of perceived infectability and germ aversion that is widely used to evaluate participants' perceived infectious disease vulnerability. Its items are scored on a 7-point Likert scale. Half of the items are reverse-scored (23, 24). PVDS has a Cronbach's α of 0.70, 0.72, and 0.70 for perceived infectability, germ aversion, and total PVDS score, respectively (24), and has been used on a Nigerian sample (25).
3. Results
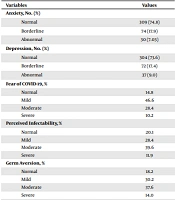
Most of the participants were female (n = 215; 52.1%) with a mean age (± SD) of 38.70 ± 8.60 years. The youngest and oldest participants aged 21 and 60 years. The majority were married (n = 290; 70.2%), with an education level of tertiary (n = 348; 84.3%). In addition, concerning the job position, most of the participants were nurse (n = 87; 21.1%), followed by other clinical positions (10 clinical psychologists, 16 social workers, 21 pharmacists, and 7 occupational therapists), and physician (n = 36; 8.7%). Also, 236 (57.1%) were non-clinical staff (health attendants (n = 89), ambulance drivers (n = 11), statisticians (n = 23), accountants (n = 16), administrative officers (n = 75), and clerical staff (n = 22). Anxiety was present in 104 participants, among which 74 had the borderline level of anxiety, while 30 had an abnormal level of anxiety. Depression was present in 109 participants, of which 72 were borderline, and 37 were abnormal (See Table 1).
| Variables | Values |
|---|---|
| Anxiety, No. (%) | |
| Normal | 309 (74.8) |
| Borderline | 74 (17.9) |
| Abnormal | 30 (7.03) |
| Depression, No. (%) | |
| Normal | 304 (73.6) |
| Borderline | 72 (17.4) |
| Abnormal | 37 (9.0) |
| Fear of COVID-19, % | |
| Normal | 14.8 |
| Mild | 46.6 |
| Moderate | 28.4 |
| Severe | 10.2 |
| Perceived infectability, % | |
| Normal | 20.1 |
| Mild | 28.4 |
| Moderate | 39.6 |
| Severe | 11.9 |
| Germ aversion, % | |
| Normal | 18.2 |
| Mild | 30.2 |
| Moderate | 37.6 |
| Severe | 14.0 |
| PVD, % | |
| Normal | 15.5 |
| Mild | 35.0 |
| Moderate | 36.4 |
| Severe | 13.1 |
It was hypothesized that PVD can significantly predict levels of fear of COVID-19 among HCW in Benin City Edo State, Nigeria. Linear regression analyses were used to test the extent to which the factors and composite score of PVD can independently and significantly predict the severity of Fear of COVID-19 among the participants. As summarized in Table 2, Perceived infectability was found to predict Fear of COVID-19 independently and significantly (β = 0.244, P = 0.000), reporting an R2 of 0.075. Germ aversion also could independently and significantly predict fear of COVID-19 (β = 0.166, P = 0.000) reporting an R2 of 0.033. Finally, the composite score of PVD also significantly predicted Fear of COVID-19 (β = 0.96, P = 0.000), reporting an R2 of 0.099. Also, according to the findings, perceived infectability, germ aversion, and a composite score of PVD could explain about 7.5, 3.3, and 9.9% of the variance of fear of COVID-19, separated by the severity, respectively. Furthermore, it was hypothesized that anxiety and depression can jointly and independently predict the severity of fear of COVID-19 among the HCW. Multiple regression analysis was used to test this hypothesis. Also, a significant joint prediction of the fear of COVID-19, separated by anxiety and depression, is provided in Table 2. The analysis showed that anxiety and depression can jointly explain 4.0% of the variance in fear of COVID-19 among the participants. This result further revealed that only depression (β = 0.196, t = 4.049, p = 0.000) had a significant independent predictive influence on the severities of the fear of COVID-19 among the participants.
| Variables | B | β | t | Sig. | R2 | F | P |
|---|---|---|---|---|---|---|---|
| Perceived infectability | 0.244 | 0.274 | 5.775 | 0.000 | 0.075 | 33.35 | 0.000 |
| Germ aversion | 0.166 | 0.182 | 3.755 | 0.000 | 0.033 | 14.101 | 0.000 |
| Perceived vulnerability to diseases | 0.196 | 0.315 | 6.730 | 0.000 | 0.099 | 45.291 | 0.000 |
| (Constant) | 13.596 | 7.915 | 0.000 | ||||
| Depression | 0.314 | 0.196 | 4.049 | 0.000 | 0.040 | 8.598 | 0.000 |
| Anxiety | 0.053 | 0.052 | 1.071 | 0.285 |
a N = 413.
We hypothesized a significant gender difference concerning the fear of COVID-19 among the participants. An independent sample t-test was carried out to determine the influence of gender on the fear of COVID-19, on 198 males and 215 female participants. The mean (± standard deviation) score of male and female HCWs is provided in Table 3.
| Variables | Frequency | Mean | SD | t | P |
|---|---|---|---|---|---|
| Gender | 0.87 | 0.39 | |||
| Male | 198 | 17.17 | 6.25 | ||
| Female | 215 | 16.66 | 5.69 |
a N = 413.
As observed in Table 3, there was no significant difference in the occurrence of fear of COVID-19 across gender, though males obtained higher mean scores than females.
Finally, we hypothesized that Job type would significantly influence the fear of COVID-19 among HCWs. One-way analysis of variance was used to compare fear of COVID-19 among HCWs based on their Job types. The job type was classified into four groups: physicians, nurses, other clinical staff, and non-clinical staff. The independent variable represented the four different Job types, while the dependent variable was the fear of COVID-19 scores. The analysis is shown in Table 4.
| Variables | N | Mean | SD | F | Sig. |
|---|---|---|---|---|---|
| Physicians | 36 | 15.94 | 5.242 | ||
| Nurses | 87 | 16.92 | 6.219 | ||
| Other clinical staff | 54 | 16.93 | 6.331 | 0.840 | 0.472 |
| Non-clinical staff | 236 | 17.22 | 5.891 | ||
| Total | 413 | 16.91 | 5.965 |
a N = 413.
As summarized in Table 4, there was no significant influence of the fear of COVID-19 among the participants based on their job types [F (3, 413) = 0.840, P = 0.472]. According to this finding, it can be concluded that Job type does not have a significant influence on the fear of COVID-19 among the health staff in Benin, Edo State, Nigeria.
4. Discussion
COVID-19 is a major global public health concern with a significant burden on HCWs. This study assessed the PVD, anxiety, depression, and fear of COVID-19 among HCWs in Edo state, South-South geopolitical zone of Nigeria.
According to the findings, the incidence of anxiety, depression, and PVD was 24.9, 26.4, and 53.4%, respectively, which is consistent with the literature on the incidence of anxiety and depression. For instance, in a meta-analysis on HCWs caring for COVID-19 patients, Salari, Khazaie, and Hosseinian-Far (26) reported an incidence of 25.8 for anxiety. In a research study on how COVID-19 lockdown impacted HCWs' mental health, Kazmi et al. (27) reported a level of 57% for anxiety. In a study on Chinees HCWs, Liu et al. (28) reported a prevalence of 16% for anxiety. In another study, Fawzy and Hamed (29) found a 73% prevalence of anxiety among Egyptian medical students, while Cheung et al. (30) reported a 50.1% incidence among Hong Kong nurses. In comparison, Kisely et al. (31) reported an incidence of 10.5% for anxiety in a sample of Americans. The high incidence of depression in the present study is similar to previous studies (26, 27). Liu et al. (28) reported an incidence of 34.6% for depression among hospital staff caring for COVID-19 patients. An incidence of 23% is reported among Iranian medical students (32), and a 20.9% incidence is reported for depression among Iranian physicians (33).
We also found a 44.8% incidence for fear of COVID-19 among Nigerian HCWs, which is consistent with other studies carried out on either HCWs or the general population in various countries. For instance, in an Ethiopian survey, Kibret et al. (34) reported an incidence of 63% for fear of coronavirus disease among HCWs. Similarly, in a study on Inaidna general population, Roy et al. (35) reported an incidence of 40% for fear of COVID-19. Abuhammad et al. (36) found a 52.7% incidence among the Jordanian sample. In addition, an incidence of 53.8% has been reported by a Chinese study (37). Our finding also supports prior research on fears, risks, and PVD as they relate to epidemics (38-41). PVD could significantly predict the severity of fear of COVID-19 among HCWs. This is in keeping with previous studies and is a reflection of the heightened state of arousal and individual constitutional factors. Factors related to PVD (i.e., germ aversion and perceived infectability) and pathogen disgust are reported as factors that contribute to concern about COVID-19 (42). This assertion is linked to the behavioral immune system (BIS) theory (42-44). According to Schaller and Park (44), the BIS is evolved by organisms to identify and mobilize defense against pathogens (43) and to avoid disease infection. BIS includes germ aversion (a factor of PVD). The roles of germ aversion include identifying disease sources, encouraging disease avoidance, and lowering the risk of infection (44).
HCWs experience high levels of stress during outbreaks. For instance, during the Ebola virus outbreak, Chinese HCWs reported severe depression, somatization, obsession-compulsion, and anxiety (45). Or during the Middle East Respiratory Syndrome coronavirus (MERS CoV) epidemic, a Saudi study found that nearly two-thirds of hospital staff believed being exposed to increased risk of MERS CoV infection and expressed the feeling of working at an unsafe workplace (46). Factors such as overwhelming circumstances, social disturbance of everyday life, feeling helpless, increased risk of infection, and fear of transmitting the disease to family and loved ones are associated with poor mental health status (47). As experienced during previous outbreaks, HCWs experience high levels of stress during health emergencies, of which COVID-19 is not an exception.
We also found that anxiety and depression jointly predicted the severity of the fear of COVID-19 among Nigerian HCWs. This result supports Zhang et al. (13) and Ahorsu et al. (8). In addition, most recent literature has reported a direct association between anxiety (39), depression (8), and fear of COVID-19 (48). Our findings, therefore, support these results, thus affirming that among HCWs in Nigeria, observed fear of COVID-19 is associated with anxieties and depression. We found no gender difference concerning the occurrence of fear of COVID-19. This was contrary to findings by Broche-Pérez et al. (49), which showed that being female was a predictor of medium and high levels of COVID-19 fear, corroborating international evidence that women are more vulnerable psychologically during the COVID-19 pandemic (17, 50, 51). Even though gender-disaggregated data for COVID-19 reveals an equivalent number of cases in both gender, existing research suggests higher mortality rates among men than women. However, in studies carried out during the pandemic, Huang and Zhao (52) and Sandin et al. (53) reported no significant gender difference in anxiety, stress, and depression levels, thus querying the assertions that females were more vulnerable to such disorders.
Finally, the type of job had no significant influence on the fear of COVID-19, which is a similar indication of fear of COVID 19 among medical personnel irrespective of their job role. The anxiety associated with COVID-19 reported by previous studies (27, 28) is widespread across populations (10, 12), irrespective of job type or position. Our finding supports Salari et al. (26), who reported a similar result, affirming that though the level of fear and anxiety was lower in physicians than in other hospital staff, the difference was not statistically significant. In a Filipino study among nurses, job function was a significant predictor of COVID-19 fear among frontline nurses, with part-time nurses reporting greater fear than their regular counterparts (54).
4.1. Study Limitations
It is necessary to mention some limitations and biases of our study, including selecting participants from two hospitals. Hence, the results of this study cannot be said to reflect the general perception of all Nigerian HCWs towards COVID-19. In addition, the population of this study includes all HCWs in the selected hospitals and not only those directly involved with the virus.
4.2. Conclusions
This study demonstrated a high incidence of anxiety, depression, and fear of COVID-19 among Nigerian HCWs. Factors related to the perceived vulnerability of diseases (perceived infectability and germ aversion) are strong predictors of fear of COVID-19. In addition, anxiety, and depression were found as significant joint predictors of Fear of COVID-19. Finally, fear of COVID-19 was neither influenced by gender nor the job type of the Nigerian HCWs.