1. Background
The spleen contains lymphoid tissue containing splenic macrophages, which is crucial in eliminating encapsulated organisms (1, 2). The role of the spleen was first described in the 1900s (1). However, the first morbidity and mortality rates associated with the absence of the spleen were discovered in the 1950s (3). Asplenia is primarily caused by congenital or surgical conditions (4). Splenectomy has decreased recently but may still be indicated due to trauma, cancer, or hematologic conditions (5).
Infections and thrombotic events are the most common medical complications of splenectomy, and it is necessary for clinicians to be familiar with these possibilities (2, 6). There is an increase in the rate of infections following splenectomy by three folds during the first 30 months and an increase in intra-abdominal abscess formation by four folds (7, 8). Sepsis may result from any organism, including bacteria, viruses, fungi, and protozoa, in an asplenic patient (9). Despite this, Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae are the most common pathogens causing infection in splenectomized patients due to compromised opsonization and phagocytosis. Statistics show that around 60% of infection cases and mortalities belong to S. pneumoniae. Furthermore, 6% of infection cases are attributed to N. meningitidis, with a mortality rate of 32% (10).
Overwhelming post-splenectomy infection (OPSI) was first described in 1951 as a potentially serious complication following splenectomy (3, 11). It is estimated that the prevalence of OPSI is 0.04% in patients with routine splenectomy and 0.03% in trauma-related splenectomies (12). OPSI mainly presents with flu-like prodromal signs and symptoms. Patients report chills, fevers, headaches, fatigue, myalgia, nausea, and vomiting (13). Thus, patients with asplenia should take any episode of fever of any grade seriously and consult a physician immediately (14).
2. Objectives
The aim of our study is to investigate the bacterial etiology of fever episodes in splenectomized patients at three specialized centers in Mashhad.
3. Methods
This cross-sectional study was conducted on all splenectomized patients with fever episodes referred to Imam Reza, Ghaem, and Dr. Sheikh hospitals between 2006 and 2017. The Ethics Committee approved the present study of Mashhad University of Medical Sciences.
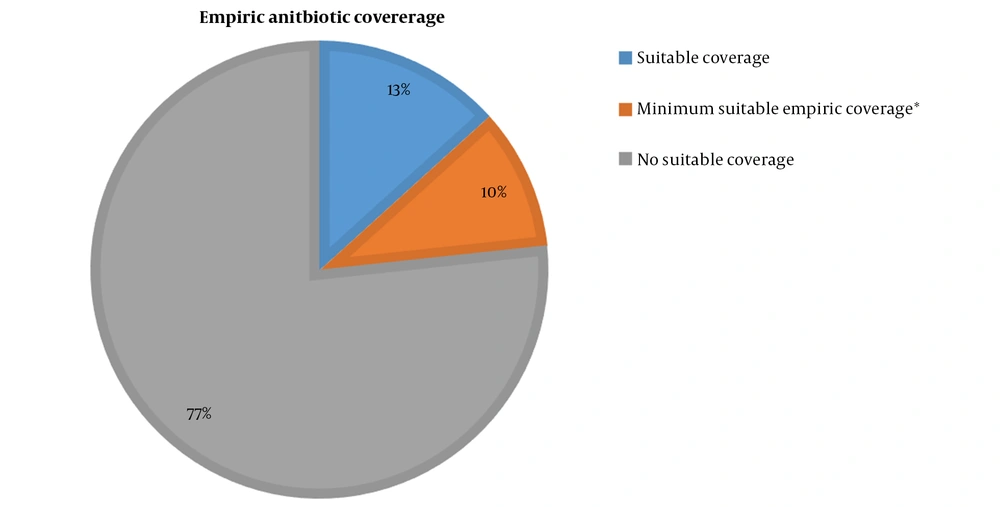
Patient data were extracted from archived patient records and coded to maintain confidentiality and patient privacy. The provided checklist for extraction included age, gender, age at splenectomy, times of hospitalization due to fever episodes, duration of hospitalization, indications for ICU admission, recorded vital signs at admission, clinical signs and symptoms (flu-like signs and symptoms, fever, headache, fatigue, chills, myalgia, weight loss, abdominal pain, nausea, vomiting, diarrhea, pneumonia, meningitis, electrolyte disturbances, acidosis, hypoglycemia, respiratory distress, altered mental status, and shock,), bacterial culture results, antibiotic prophylaxis, vaccination history, hospital outcome, and 6-month and one-year outcomes. In addition, antibiotic coverage was classified as either suitable (e.g., ceftriaxone + vancomycin or a fluoroquinolone + vancomycin), not suitable, or minimum suitable empiric coverage, in which broad-spectrum antibiotic coverage was justified according to the clinician, but may not be compliant with stewardship guidelines (15).
For statistical analyses, recorded data were entered in SPSS Statistics 20. The descriptive analysis mainly included calculating relative and absolute frequency, mean, standard deviation, and median.
4. Results
We reviewed 280 patients who underwent splenectomy between 2006 and 2017 and were able to enroll 23 splenectomized patients who experienced fever episodes. Some of the enrolled patients had a history of several hospitalizations due to fever, amounting to 30 fever episodes.
Among the 280 patients reviewed, 40% were males, and 60% were females. In addition, 220 of the participants were adults, and 60 were children. Seventy-six patients underwent splenectomy due to idiopathic thrombocytopenic purpura (ITP), 17 to abdominal trauma, and 17 to spherocytosis. Patient ages ranged from 1 to 76 years.
A total of 23 splenectomized patients with fever episodes had a mean age of 24.2 ± 1.6 years, ranging from 1 to 69 years. In the study, 47.8% of the patients were males, and 52.2% were females. Sixty-two percent of the patients with fever episodes had a complete pneumococcal vaccination, while the remainder did not. The mean age at splenectomy was 19.6 ± 1.6 years, with an age range of 1 to 65. The most common causes of splenectomy were spleen masses (i.e., spleen tumors and spleen abscesses) and idiopathic thrombocytopenic purpura (ITP), each accounting for four (17.4%) cases. Hemolytic anemia, thalassemia, and Gaucher's disease accounted for three (13%), two (8.7%), and two (8.7%) cases, respectively (Table 1).
| Feature | Statistic |
|---|---|
| Age | 24.2 ± 1.63 |
| Gender | |
| Male | 11 (47.8) |
| Female | 12 (52.2) |
| Age of the patient at the time of splenectomy | 19.6 ± 1.6 |
| Cause of splenectomy | |
| Spleen mass | 4 (17.4) |
| Thalassemia | 2 (8.7) |
| ITP | 4 (17.4) |
| Hemolytic anemia | 3 (13.0) |
| Gaucher's disease | 2 (8.7) |
| Other | 8 (34.8) |
a Values are expressed as mean ± SD or No. (%).
The median admission duration was seven days, ranging from 1 to 52 days. The interval between splenectomy and the first episode of fever ranged from 0 days to more than three years. In most cases, admissions were caused by intra-abdominal infections (26.7%), pneumonia (13.3%), and bacteremia (10.0%). There was one case (3.3%) of meningitis and one (3.3%) case of soft tissue infection.
Two patients (6.7%) presented with sepsis. In 30 fever episodes, only two (6.7%) resulted in the patient's death. (Table 2)
| Feature | Statistics, No. (%) |
|---|---|
| The time between splenectomy and episode of fever | |
| 0 - 30 day | 9 (30.0) |
| 31 - 90 day | 8 (26.7) |
| 91 - 365 day | 2 (6.7) |
| 1 - 3 year | 8 (26.7) |
| After three year | 3 (10.0) |
| Cause of admission | |
| Pneumonia | 4 (13.3) |
| Bacteremia | 3 (10.0) |
| Meningitis | 1 (3.3) |
| Soft tissue infection | 1 (3.3) |
| Abdominal infection | 8 (26.7) |
| Sepsis | 2 (6.7) |
| Other | 11 (36.7) |
| Outcome | |
| Alive | 28 (93.3) |
| Expired | 2 (6.7) |
Table 3 shows the results of different cultures, including blood, stool, urine, CSF, bronchial secretions, and abdominal samples. Four cases (13.3%) of blood cultures were positive for S. pneumonia, Staphylococcus aureus, Citrobacter, and Brucella. Urine culture was positive in one case (3.3%) for a coagulase negative staphylococcus. The bronchial culture was positive in three cases (10.0%), comprised of S. aureus, Pseudomonas aeruginosa, and Enterobacter. In one case (3.3%), the abdominal culture was positive for Staphylococcus epidermidis. However, CSF culture was negative in one case of meningitis despite evidence of polymorphonuclear infiltrate and flame-shaped gram-positive diplococci on microscopy.
| Feature | Frequency (%) |
|---|---|
| Blood culture | |
| Positive | 4 (13.3) |
| Negative | 15 (50.0) |
| Not done | 11 (36.7) |
| Stool culture | |
| Negative | 1 (3.3) |
| Not done | 29 (96.7) |
| Urine culture | |
| Negative | 12 (40.0) |
| Positive | 1 (3.3) |
| Not done | 17 (56.7) |
| Chest or abdominal culture | |
| Positive | 3 (10.0) |
| Not done | 27 (90.0) |
| CSF culture | |
| Negative | 1 (3.3) |
| Not done | 29 (96.7) |
The results of antibiotic coverage are shown in Figure 1. Patients received suitable antibiotic coverage in 13.3% (i.e. ceftriaxone + vancomycin or a fluoroquinolone + vancomycin), minimum suitable empiric coverage in 10.0%, and no suitable coverage in 76.7% of episodes.
5. Discussion
The main aim of our study was to assess the bacterial etiology responsible for episodes of fever in splenectomized patients. The majority of patients were admitted due to intra-abdominal infections (26.7%), pneumonia (13.3%), and bacteremia (10.0%). Positive blood culture was reported in four (13.3%) cases and a positive bronchial culture in three (10%) cases. In one (3.3%) case, both the abdominal and urine cultures were positive. On the other hand, there was one case of meningitis in which a CSF culture was negative, but microscopy revealed a polymorphonuclear infiltrate and flame-shaped gram-positive diplococci. Isolated organisms were varied and included S. pneumoniae, S. aureus, coagulase negative staphylococci, P. aeruginosa, Brucella, and Citrobacter. A lack of attention to timely sample collection before antibiotic administration may have contributed to the high rate of false negatives. 76.7% of cases received no suitable antibiotic coverage, while 23.3% received at least the minimum suitable empiric coverage.
Among 33 patients who underwent splenectomy, Barmparas et al. (7) reported 8 cases of urinary tract infections, 5 cases of bacteremia, 3 cases of intra-abdominal abscess formation, and 2 cases each of ventilatory-associated pneumonia, wound infection, and catheter-related bloodstream infection. They reported that splenectomy made patients three times more susceptible to infection and four times more susceptible to intra-abdominal abscess formation. In our study, of 30 episodes in splenectomized patients, there were eight cases of intra-abdominal infection, four cases of pneumonia, three cases of bacteremia, two cases of sepsis, and one of meningitis, and one case of soft tissue infection (Table 2). Based on these statistics, it appears that intra-abdominal infections are very common among splenectomized patients.
In their study, Thai et al. (16) reported 14 cases of pneumonia, seven cases of gastrointestinal, urogenital, and skin infections, and five cases of infection of unknown origin among 94 patients undergoing splenectomy due to immune thrombocytopenia. As a result of the 26 episodes of infection, five cases of sepsis or septic shock were reported, three of which resulted in death. In our study, only two (6.7%) of 30 fever episodes resulted in death. According to our study, most infections occurred within 31 to 90 days or one to three years following splenectomy. Other studies have found that the incidence of the infection increases during the first two years following splenectomy, but the risk persists throughout life (17, 18). A longitudinal study conducted by Bisharat et al. found that approximately half to two-thirds of infections following splenectomy occurred within the first two years with an average of 22.6 months (19). Holdsworth et al. (20) reported that the time to infection is lower in patients with splenectomy due to hematologic problems (median interval of 20 months) compared to post-traumatic splenectomy (median interval of 50 months). Partially removing the spleen is thought to be associated with a lower risk of infection, but there are still some controversies (21, 22). In our study, all cases had undergone total splenectomy.
Asplenic patients may be at risk of serious infections. Preventative measures, such as receiving the 23-valent pneumococcal vaccine, are believed to cover around 70 to 90% of strains responsible for OPSI (4). It is also important to educate patients that fevers of any type should be taken seriously and that they should consult a physician immediately (23, 24).
Our study investigated the rate and etiology of different infections in splenectomized patients and their outcomes. Despite extending the study period to 11 years to maximize sample size and increase accuracy, we were able to include only 23 patients due to the rarity of fever episodes in splenectomized patients.
5.1. Conclusions
Our study aimed to assess the bacterial etiology of fever episodes in patients who had undergone splenectomy. We found that intra-abdominal infection (26.7%), pneumonia (13.3%), and bacteremia (10.0%) were the most prevalent infections, with all causes accounting for a total of 30 fever episodes. Bacterial culture was conducted on various samples, including blood, stool, urine, bronchial secretions, and abdominal samples, and nine (24%) were positive. Isolated organisms were varied and included S. pneumoniae, S. aureus, coagulase negative staphylococci, P. aeruginosa, Brucella, and Citrobacter. Despite the presence of a polymorphonuclear infiltrate and flame-shaped gram-positive diplococci on microscopy in one case of meningitis, a CSF culture was negative. A high proportion of negative culture results may be explained, in part, by the collection of samples following the administration of antibiotics.
Moreover, about 76.7% of the cases had no suitable antibiotic coverage, and about 23.3% had received at least the minimum suitable empiric coverage. Ultimately, 2 of 30 episodes ended in patient death, accounting for an episode survival rate of 93.3%. This study reinforces the importance of timely sample collection before antibiotic administration, proper attention to culture results in order to guide antibiotic coverage, and education regarding appropriate empiric treatment.