1. Background
Over recent decades, halitosis has become a priority in oral hygiene maintenance worldwide (1) and significantly affects social relationships (1). Currently, bad breath is one of the main reasons for referral to dentists in Iran, requiring clinicians and manufacturers to make large investments in cosmetic products for halitosis improvement (1). However, the primary underlying reason for halitosis is often unclear, resulting in only temporary relief after the use of these products (2).
Volatile sulfur compounds (VSCs) are considered the main causative substances for halitosis. The majority of VSCs reportedly comprise hydrogen sulfide and methyl mercaptan (3, 4) and can cause various types of mouth odor (4). It has been shown that the main origin of oral malodor is in the oral cavity, e.g., periodontal pockets (5, 6). This phenomenon mainly results from the putrefaction of amino acids by bacteria under anaerobic conditions (1, 6). This anaerobic microenvironment houses different bacterial species that majorly include a range of gram-negative proteolytic strains (1, 3). VSC is the main product of proteolysis by these organisms, which utilizes sulfur-containing amino acid resources such as cysteine and methionine (7).
Several anaerobic gram-negative bacteria have been mentioned for their role in VSC production, with Fusobacterium species being one of the most common (5, 7, 8). Previously, it was shown that the plaque biofilm is a major source of halitosis-inducing VSCs produced by anaerobic gram-negative bacteria. Fusobacterium species play a critical role in this phenomenon, along with other bacteria in plaque biofilms (7). With regard to this issue, it was previously indicated that FomA, which is one of the major outer membrane proteins of Fusobacterium nucleatum, could be an agent for recruiting other anaerobic gram-negative bacteria into periodontal pockets, thus facilitating the formation of plaque biofilms (7).
Although halitosis is primarily the result of endogenous factors such as microbial metabolism, it is a multifactorial condition (7) that can be affected by exogenous factors such as diet and smoking or, occasionally, physiological factors such as a low salivary flow due to insufficient water intake (1, 3).
2. Objectives
Because of the reported role of Fusobacterium species in production of bad smell and the lack of a study showing an obvious association between halitosis and any specific bacterial isolate, we aimed to determine any probable relationship between the presence of Fusobacterium species and halitosis, as well as the relationship between some exogenous and physiological factors and halitosis.
3. Patients and Methods
3.1. Subjects and Study Design
In this case–control study conducted from October 2012 to March 2013, 50 patients with confirmed halitosis (27 women and 23 men; mean age, 37 ± 11 years; range, 19 - 54 years) and 50 patients (33 women and 17 men; mean age, 38 ± 12 years; range, 20 - 62 years) without oral malodor were included. All subjects were patients referred to Emam Reza polyclinic, which is affiliated to Shiraz university of medical sciences, Shiraz, Iran. Emam Reza polyclinic is a government-owned medical center with 11 floors and several clinical facilities, including dentistry, and it serves approximately 600 thousand patients in Fars province every month. All individuals who had not brushed, rinsed, smoked, eaten, or consumed any beverage for at least 2 h prior to assessment were sampling and included for analysis. Furthermore, none of the subjects had a history of antibiotic therapy for at least a month. The Ethics Committee of Shiraz University of Medical Sciences approved the study design (EC-91-6329). Informed consent was obtained from all participants before study initiation. A standardized checklist was designed by the authors and subjected to pilot tests before the survey. Self-reported information regarding medical and dental histories and a few dietary habits was obtained from all participants to evaluate the presence of potential risk factors for halitosis (Table 1).
| Oral Disease a | Drug b | Systemic Disease a | Foods with Sulfur-Containing Amino Acids c | References |
|---|---|---|---|---|
| Periodontal disease, dental cavity, cracked tooth, and ulcers, etc. | Antidepressive, antihistaminic, antihypertensive, antiparkinson, anxiolytic, diuretic, and anorexigenic agents | Sinusitis, diabetes, gastrointestinal disease, renal failure, respiratory infection, urinary tract infection, lactose intolerance, decreased salivary flow | Curry powder, chili, coffee, tea, carbohydrates (sugar), garlic, onion, yogurt, lentils, sausage, and chicken meat | (1, 3) |
a Self-reported disease was considered a positive risk factor.
b Self-reported consumption of any of the mentioned drugs was considered a positive risk factor.
c Self-reported high consumption of any of the mentioned foods was considered a positive risk factor.
3.2. Oral Malodor Assessment
The degree of oral malodor in each subject was assessed by two dentists (kappa = 0.82, P < 0.05) using an organoleptic test (OLT). Scores were estimated on a scale of 0 - 5: 0, no malodor; 1, very slight; 2, slight; 3, moderate; 4, strong; and 5, very strong. Subjects with a score of > 2 were included in the halitosis group, while those with a score of ≤ 2 were included in the control group (4).
3.3. Clinical Sampling
Samples were obtained from the periodontal pockets of subjects under aseptic conditions using absorbent paper points. After sampling, the paper points were pooled in capped plastic tubes containing 1 mL of anaerobic transport medium composed of thioglycollate broth (Merck, Germany), 0.05% Tween 80 (Merck, Germany), 5 μg of hemin (Sigma, UK) per mL, and 0.5 μg of menadione (Sigma, UK) per mL. All samples were immediately transported to the laboratory and cultured.
3.4. Culture and Identification
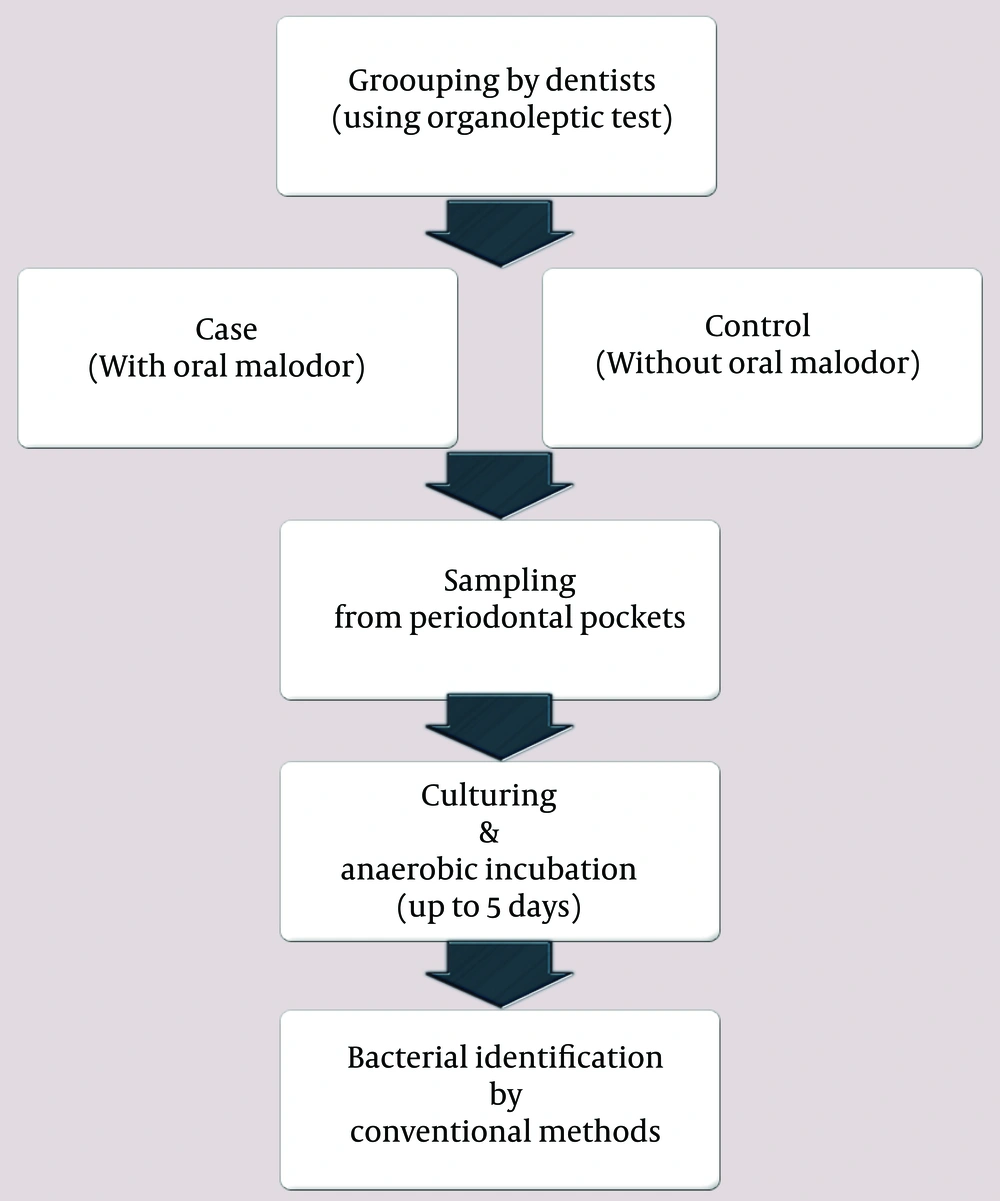
The samples were mixed using a vortex for 1 min to allow the dispersal of bacteria. Then, 20 μL of the solution was taken from each tube and spread onto an anaerobic agar plate modified for the selection of Fusobacteria. The agar comprised columbia agar (Merck, Germany), 0.05% Tween 80 (Merck, Germany), 0.5 μg of menadione (Sigma, UK) per mL, and 5% fresh defibrinated blood. This medium was supplemented with vancomycin (5 μg/mL, Sigma), neomycin (100 μg/mL, Sigma), and erythromycin (5 μg/mL, Sigma) (9, 10). The plates were incubated in anaerobic jars using GasPak A (Merck, Germany) for up to 5 days at 37°C. The primary identification of Fusobacterium was based on the presence of typical pleomorphic, gram-negative, rod-shaped or fusiform bacilli on gram staining and positive susceptibility of Fusobacterium species to kanamycin (1 mg) and colistin (10 μg) and resistance to vancomycin (5 μg) on susceptibility testing (MAST, UK). The species were characterized through standard biochemical tests (11). A simplified flow chart of the study is illustrated in Figure 1.
3.5. Statistical Analysis
All statistical analyses were performed using SPSS software version 19.0 (IBM Corp., Armonk, NY, USA). The frequency of bacterial isolation and risk factors are presented as descriptive statistics in terms of relative frequency. Chi-square and Fisher’s exact tests were used to estimate any statistical associations as appropriate. A P value < 0.05 was considered statistically significant.
4. Results
Statistical analysis revealed no significant association of sex and age with halitosis. In total, 26% (n = 13) and 8% (n = 4) samples from the halitosis and control groups, respectively, were positive for Fusobacterium species, with F. nucleatum present in the largest proportion in both groups (Table 2).
| Isolates | Groups | ||
|---|---|---|---|
| Individuals With Oral Malodor | Individuals Without Oral Malodor | Level of Significance, P-Value | |
| F. nucleatum | 10 (20.0) | 4 (8.0) | 0.148 |
| F. necrophorum | 3 (6.0) | 0 (0) | 0.242 |
| Total | 13 (26.0) | 4 (8.0) | 0.05 |
a Data are presented as No. (%).
The frequency of halitophobia was significantly higher in the halitosis group (68%) than that in the control group (26%). Sinusitis was the major systemic disease in the halitosis [70% (14/20)] and control groups [61.5% (8/13)] and in subjects with positivity for Fusobacteria species.
Curry powder, chili, and sausage consumption was more common (P < 0.05) in the diet of subjects with halitosis than in those without. There were no significant differences in other diet patterns between the two groups. Correlation analyses for risk factors in the studied groups are presented in Table 3.
| Risk Factors | Groups | ||
|---|---|---|---|
| Individuals With Halitosis | Individual Without Oral Malodor | Level of Significance (P-Value) | |
| Fusobacteria isolation | 13 (26.0) | 4 (8.0) | 0.05 |
| Halitophobia | 34 (68.0) | 13 (26.0) | 0.001 |
| Active or passive smoking | 8 (16.0) | 10 (20.0) | 0.79 |
| Job-related dryness of mouth | 13 (26.0) | 5 (10.0) | 0.05 |
| Drug usage | 9 (18.0) | 8 (16.0) | 0.79 |
| Oral disease | 19 (38.0) | 18 (36.0) | 0.84 |
| Sinusitis | 14 (28.0) | 8 (16.0) | 0.23 |
| Systemic disease | 20 (40.0) | 13 (26.0) | 0.14 |
| Tooth brushing | 48 (96.0) | 49 (98.0) | 0.56 |
| Flossing | 20 (40.0) | 23 (46.0) | 0.55 |
| Rinsing | 9 (18.0) | 14 (28.0) | 0.24 |
| Curry powder | 37 (74.0) | 27 (54.0) | 0.05 |
| Chili | 27 (54.0) | 17 (34.0) | 0.05 |
| Coffee | 9 (18.0) | 10 (20.0) | 0.8 |
| Tea | 32 (64.0) | 30 (60.0) | 0.68 |
| Carbohydrates | 32 (64.0) | 27 (54.0) | 0.31 |
| Garlic | 14 (28.0) | 12 (24.0) | 0.65 |
| Onion | 26 (52.0) | 25 (50.0) | 0.84 |
| Yogurt | 42 (84.0) | 42 (84.0) | 1.0 |
| Lentil | 30 (60.0) | 23 (46.0) | 0.16 |
| Sausage | 12 (24.0) | 2 (4.0) | 0.05 |
| Chicken meat | 43 (86.0) | 40 (80.0) | 0.42 |
a Data are presented as No. (%).
Although the majority of subjects positive for Fusobacterium species in the halitosis group (53.8%) exhibited some form of oral disease (periodontal disease, dental caries, cracked tooth, ulcers, etc.), there were no significant differences in the disease incidence between these subjects and those negative for Fusobacterium species (Table 4). Furthermore, job-related dryness of mouth was more frequent in subjects positive for Fusobacterium species than in their negative counterparts in the halitosis group (P < 0.001). In addition, the rates of flossing and consumption of chili, coffee, tea, carbohydrates, garlic, and onion were significantly different (P < 0.05) between the positive and negative subjects in the halitosis group.
| Risk Factors | Groups | ||
|---|---|---|---|
| Fusobacteria positive/With Oral Malodor | Fusobacteria Negative/With Oral Malodor | Level of Significance (P-Value) | |
| Halitophobia | 9 (69.2) | 25 (67.6) | 0.89 |
| Active or passive smoking | 3 (23.1) | 5 (13.5) | 0.39 |
| Job-related dryness of mouth | 8 (61.5) | 5 (13.5) | 0.0006 |
| Drug usage | 4 (30.8) | 5 (13.5) | 0.16 |
| Oral disease | 7 (53.8) | 12 (32.4) | 0.17 |
| Sinusitis | 3 (23.1) | 11 (29.7) | 0.67 |
| Systemic disease | 5 (38.5) | 15 (40.5) | 0.89 |
| Tooth brushing | 12 (92.3) | 36 (97.3) | 0.44 |
| Flossing | 10 (76.9) | 10 (27.0) | 0.0019 |
| Rinsing | 4 (30.8) | 5 (13.5) | 0.16 |
| Curry powder | 11 (84.6) | 26 (70.3) | 0.32 |
| Chili | 6 (46.2) | 21 (56.8) | 0.53 |
| Coffee | 0 (0) | 9 (24.3) | 0.05 |
| Tea | 5 (38.5) | 27 (73) | 0.028 |
| Carbohydrates | 4 (30.8) | 28 (75.7) | 0.0038 |
| Garlic | 1 (7.7) | 13 (35.1) | 0.05 |
| Onion | 3 (23.1) | 23 (62.2) | 0.015 |
| Yogurt | 2 (15.4) | 31 (83.8) | 0.93 |
| Lentil | 9 (69.2) | 21 (56.8) | 0.41 |
| Sausage | 4 (30.8) | 8 (21.6) | 0.50 |
| Chicken meat | 12 (92.3) | 31 (83.8) | 0.43 |
a Data are presented as No. (%).
5. Discussion
Halitosis is associated with not only severe personal problems and social embarrassment but also periodontal disease (5). Therefore, accurate diagnosis of the underlying cause is important for effective therapy (12).
The relationship between the presence of Fusobacterium species in periodontal pockets and halitosis in our study is consistent with that observed in the study by Donaldson et al. who also isolated Fusobacterium species from patients with and without halitosis. However, the rate of bacterial isolation was slightly higher in the halitosis group in our study (P < 0.05) (13). The majority of isolates (82.3%, 14/17) in our study were those of F. nucleatum. F. nucleatum causes halitosis through the production of large amounts of VSCs and the accumulation of other VCS-producing bacteria (7, 14). In addition, it is often associated with periodontal diseases (14). Fusobacterium species with the ability to cause oral malodor belong to endogenous flora (7). Of the total Fusobacterium isolates in our study, 23.1% were those of F. necrophorum, a proportion close to that in the study by Gomes et al. (15). Although not confirmed, F. necrophorum has been predicted to be a part of the commensal flora in the oral cavity, considering its close association with infections in the head and neck region (16, 17).
In our study, there was a significant correlation between halitosis and job-related dryness of mouth (lack of water intake for several hours during work). A decrease in the salivary flow rate is generally considered a risk factor for bad breath because of the decreased cleansing action normally provided by the flow of saliva, with a concomitant change in the pattern of the oral flora (18). However, in our study, the presence of dry mouth was self-reported by subjects.
It was previously mentioned that oral hygiene maintenance (e.g., tooth brushing, flossing, and rinsing) could be an influential factor in the elimination or amelioration of halitosis, although there were no significant differences in this regard between subjects with and without halitosis in our study (Table 3) (19).
The correlation between systemic diseases and oral malodor, particularly sinusitis, was not strong in our study, although some authors have reported systemic diseases as possible risk factors (7, 20).
Several studies have reported strong correlations between halitosis and periodontal diseases, which are characterized by deep pockets that are considered sites for bacterial interactions and, consequently, greater VSC production (12, 21). However, there was no significant difference in the rate periodontal diseases between the halitosis and control groups in our study. Oral diseases were observed in up to 40% subjects in both groups, with an incidence of >50% among subjects positive for Fusobacterium species.
Halitophobia is a psychological problem used to describe apparently healthy individuals with a delusional fear of halitosis, even though it is not actually present (22). In our study, the majority (68%) of individuals with an organoleptic score of >2 before examination by a physician complained of bad breath. It can be concluded that the fear of halitosis is more likely to come true in those with the actual condition.
There are reports of a consistent association between halitosis and the consumption of volatile foods such as onion, garlic, and spices giving rise to transient changes in breath odor (1, 3). One of the main influential factors in the present study was the consumption of foods containing cysteine and methionine residues, which are potential nutrient sources for proteolytic anaerobic bacteria and subsequent VCS production (1, 7). Increased consumption of curry powder, chili, and sausage in individuals with halitosis is indicated to be a potential etiological factor (3).
The proportion of isolated anaerobic bacteria was reported to be significantly higher in individuals with active periodontal sites characterized by probing depths of ≥ 6 mm than in those with shallow and noninflamed sites (23). This may explain the significant difference in the Fusobacterium isolation rate between subjects who flossed and those who did not in the halitosis group in our study (Table 4).
In our study, there was no significant association between carbohydrate consumption and halitosis (Table 3). However, the consumption of carbohydrates was significantly higher in subjects negative for Fusobacterium species than in those positive for the same in the halitosis group (Table 4). Previously, it was documented that pH reduction by the production of acid compounds from carbohydrates, the main nutrients for oral bacteria, may inhibit the growth of proteolytic bacteria such as Fusobacterium (24-26). Moreover, Han et al. showed that the attachment of F. nucleatum to epithelial cells involves a lectin-like adhesin that can be inhibited by galactose-containing sugars (27). However, it has been demonstrated that the presence of fimbriae play a key role in the attachment of F. necrophorum to host cells (28).
Also, another notable finding in the halitosis group in our study was a significantly (P < 0.05) higher consumption of chili-containing foods, coffee, tea, garlic, and onion by subjects negative for Fusobacterium species than by those positive for the same. Such eating habits could be another cause of oral malodor regardless of the presence of Fusobacterium, because volatile foods such as onion and garlic can affect breath odor (3). This finding highlights the possible role of Fusobacterium species in the development of halitosis in the other group as well.
The present study has some limitations. First, we used conventional methods for the detection of bacterial isolates. Because of the fastidious nature of anaerobic bacteria, if molecular methods were also employed, they could improve our detection rates. Second, our sampling spot was limited to periodontal pockets, while anaerobic bacteria could colonize in other spots of the human oral cavity as well (23, 29). Finally, and most importantly, our sample size was small and the results cannot be generalized to the entire community.
In summary, within the limitations, the results of this study suggest that the presence of Fusobacterium species in periodontal pockets is an important risk factor for halitosis and may be associated with some background factors that can contribute to halitosis. Therefore, the development of treatment strategies focused on Fusobacterium eradication may effectively prevent the progression of bad breath. However, until the optimal treatment is established, further studies should work toward determining the specific role of anaerobic bacteria other than Fusobacterium species.