1. Introduction
Hydatidosis is a cyclo-zoonotic disease in which human involvement is dominantly caused by the larval stage (metacestode) of a dog tapeworm namely Echinococcus granulosus (1). Dogs and humans act as definitive and intermediate hosts, respectively. Human contamination occurs via poorly washed vegetables contaminated with the ova of E. granulosus (2, 3). When the visceral organs of intermediate hosts are eaten by canines, the cysts transform to adult worms in their small intestine (2). Hydatid cyst is frequently localized in the liver (60% - 70%) and lungs (10% - 15%) (4). However, the cases of the central nervous system (brain, spinal cord, and orbit) are responsible for 2% to 3% of the reported hydatid cysts (2, 5). The intraorbital cyst is very uncommon, reported being less than 1% of all hydatid diseases in endemic areas (2, 4). Nevertheless, in Argentina and Iraq, orbital hydatid cysts include up to 5% to 20% (5, 6).
The major sites for orbital hydatid cyst are the intraconal and extraconal spaces although extraocular muscle cases have rarely been reported (6-10). Because of the limited space in the orbital cavity, the hydatid cysts grow by an average of 1.5 centimeters each year and patients generally become symptomatic earlier than 2 years (8-10).
The orbital hydatidosis usually characterizes with slowly progressive and painless proptosis (6-10). Spontaneous cyst rupture following surgery or trauma causes swiftly progressive proptosis (11). In this article, we report intraorbital unilocular hydatid cysts in two pediatric patients in northwest Iran and emphasize the importance of an accurate diagnosis in endemic regions before surgery in order to avoid complications.
A, Preoperative appearance of the patient with proptosis of the right eye. B and C, Axial and sagittal CT scan showing a well-defined cystic mass along the posteromedial wall of the orbit. D, Intact removal of hydatid cyst. E, Hydatid cyst layers (germinal and laminated layers) in the histopathological section (H and E, 10×).
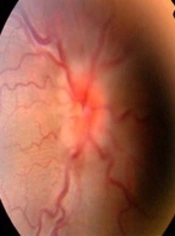
A, Preoperative appearance of the patient with proptosis of the right eye. B, Fundus photography showing optic disc swelling; C, T2 MRI revealed an intraconal mass. D, T1 MR demonstrated a homogeneous intraconal lesion. E, Hydatid cyst layers (germinal and laminated layers) in the histopathological slide (H and E, 10×).
2. Case Presentation
2.1. Patient 1
A 4-year-old boy presented with the axial proptosis of the right eye (Figure 1A). His past medical history was unremarkable. He had 3 mm proptosis in his right eye. Visual acuity was 10/10 in both eyes. Slitlamp examination, intraocular pressure, and funduscopy were normal. Orbital CT scan revealed a cystic mass on a superonasal aspect of orbit (Figure 1B and C). He underwent anterior orbitotomy and the cyst totally was removed (Figure 1D). Histopathological examination revealed explicitly an infertile (sterile) unilocular cyst composed of a PAS-positive laminated hyaline wall attached to a germinal layer (Figure 1E). Treatment with albendazole was continued for another two months. After one year of treatment, no recurrence in the orbit and liver was detected.
2.2. Patient 2
A 13-year-old boy referred because of the reduced vision in his right eye. His best-corrected visual acuity was 8/10 and 10/10 in right and left eyes, respectively. He had 3 mm axial proptosis and optic disc swelling in the right eye (Figure 2A). Fundus photography showed optic disc swelling symptoms (Figure 2B). On both MRI and CT scan, a cystic mass was seen in the retrobulbar intraconal area (Figure 2C and D). By lateral orbitotomy, the mass totally was excised. On the day after the operation, proptosis decreased significantly. Histopathological examination revealed an infertile unilocular cyst composed of a PAS-positive laminated hyaline wall attached to a germinal layer (Figure 2E). Treatment with albendazole was continued for another two months. After one year of treatment, no recurrence in the orbit was detected and the proptosis completely disappears. The patient was followed up for 5 years and there was no recurrence.
3. Discussion
The orbital hydatid cyst due to echinococcal infection is an uncommon hydatidosis in hypoendemic to hyperendemic countries. Orbital hydatidosis mostly affects children/young adults and both sexes equally (12). Furthermore, it is rare to find other simultaneous hydatid cysts elsewhere in the body (12, 13). The orbital hydatidosis is generally unilateral and affects mainly the left orbit (12). This can be described by the path of the left carotid artery. Interestingly in this study, the orbital unilocular hydatid cysts were removed from the right orbit. Rajabi et al. (2013) reported orbital hydatid cysts with diverse localities in extraconal, medial rectus, intraconal space, lacrimal gland, and intraosseous of the orbital wall (14). Bagheri et al. (2010) showed two different presentations of orbital echinococcosis due to hydatid and alveolar cysts in Iranian patients (15).
In endemic areas, the orbital hydatid cysts should be differentiated from other cystic lesions of the orbit such as mucocele, teratoma, dermoid, and lipodermoid cysts, schwannoma and paraganglioma hematocele, encephalocele, and inclusion cyst (8, 10, 16). An accurate diagnosis is essential preoperatively in order to prevent the misdiagnosis and subsequently wrong treatment. The rupture of hydatid cyst can cause lethal anaphylactic shock or seeding of protoscoleces during operation field that may become secondarily infected (16, 17). Moreover, delayed treatment may lead to blindness by optic nerve compression (13, 16, 18). Generally, orbital hydatidosis is sited either within the muscle cone or outside in the superolateral/superomedial angles (19, 20). The clinical features of intraorbital hydatidosis present the unilateral proptosis, visual impairment, ocular tension, optic atrophy, lid edema, papilledema, and chemosis.
The diagnosis of hydatid cyst in endemic areas is provided by clinical aspects, radiological explorations, and serology assays (21). If the serological results were negative, the identification of hydatid cysts should be considered in the differential diagnosis of orbital cystic lesions. However, in some cases, an accurate diagnosis depends on a histopathological assessment of the surgical case. Currently, surgical therapy is still the definitive treatment of orbital hydatidosis because of the rapid growth rate of the hydatid cyst. In this report, the patients were exposed to albendazole medication after the operation; however, recent findings have highlighted the effective therapeutic of albendazole-loaded PLGA-PEG and biosynthesized silver nanoparticles on protoscoleces in in vitro condition (22, 23). So far, no eligible genotyping has been done on orbital hydatidosis yet; however, it is expected the predominant genotype of ocular hydatidosis belongs to G1 strain because of the widespread extension of sheep-dog biology in Iran. Differential diagnoses of orbital hydatid cysts from orbital cystic lesions should be unequivocally noticed in endemic areas prior to surgery in order to avoid complications. The preoperative diagnosis of the hydatidosis is essential to avoid cyst rupture and prevent severe anaphylactic reactions, seeding, and recurrence of the disease.