1. Introduction
Cutaneous tuberculosis is a rare extrapulmonary manifestation of tuberculosis. It is imperative for dermatologists to diagnosis the variants of cutaneous tuberculosis since they masquerade a variety of conditions. Papulonecrotic tuberculid (PNT) is a rare subtype of cutaneous TB believed to represent a hypersensitivity reaction to TB antigen (1). Erythema induratum is a kind of granulomatous lobular panniculitis, most commonly appearing as subcutaneous nodules in legs and thighs (1).
The simultaneous occurrence of PNT and Erythema induratum (EI) is extremely rare (2). Here, we present a case of concomitant PNT and EI in a 53-year-old woman as the primary presentation of mycobacterium tuberculosis infection.
2. Case Presentation
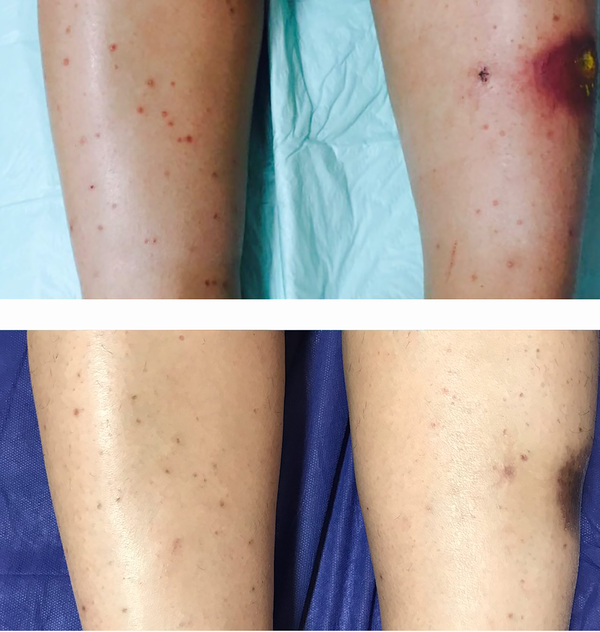
A 53-year-old woman referred to our dermatology clinic with a six-month history of multiple erythematous papules and a large red-violaceous plaque on her lower extremities. The patient did not have any systemic symptoms except for mild arthralgia of knee joints. Her past medical history was significant for cervical cancer treated with radical hysterectomy, followed by chemotherapy. Three months later, the lesions appeared as papules with gradual spreading to proximal parts of lower extremities. A physical examination revealed multiple symmetric red to brown monomorphic 2 - 3 mm sized papules with bilateral distribution on both shins, along with a large red indurated plaque with a central necrotic ulcer on the left shin. A smaller similar plaque was observed above her right lateral malleolus (Figure 1). The patient was otherwise healthy and her physical evaluation showed no significant finding. She denied any present or previous contact with active tuberculosis patients.
We performed a thorough evaluation of laboratory tests that revealed only a mild elevation in the erythrocyte sedimentation rate while all other laboratory tests including complete blood count, routine biochemistry profile, and serologic tests for HIV and VDRL were normal. Tuberculin skin test (PPD) and interferon-gamma release assay were negative and chest X-ray revealed no signs of previous or active tuberculosis.
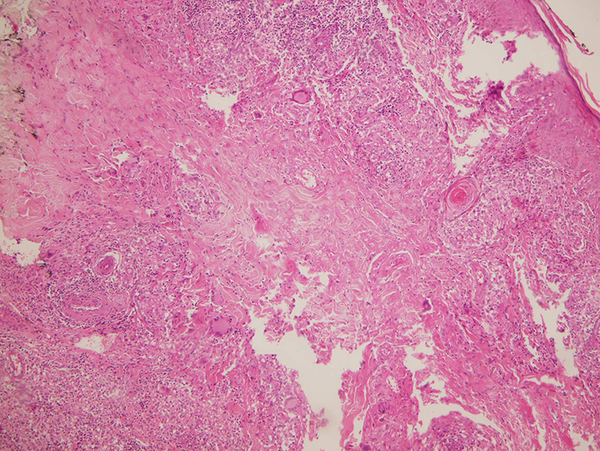
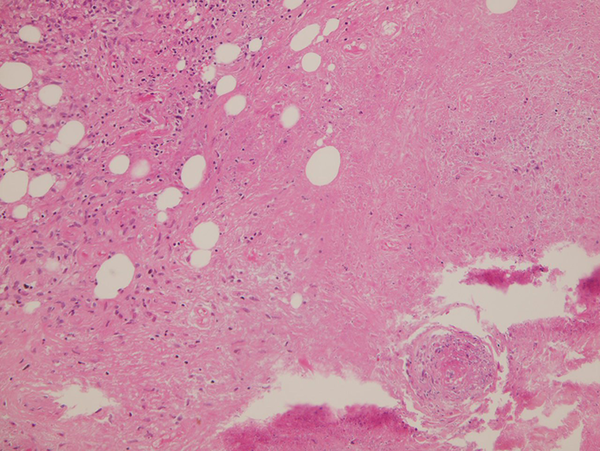
A biopsy from one of the papular lesions of the pretibial area demonstrated a tuberculoid necrotizing granulomatous inflammatory dermal reaction associated with small vessel vasculitis in favor of papulonecrotic tuberculid (Figure 2). Skin biopsy from large violaceous plaques revealed acanthosis and mild spongiosis in epidermis along with the aggregation of histiocytes with central necrosis in the underlying dermis. Moreover, inflammatory infiltration was present in the prevascular area and throughout fat lobules in the subepidermal layer (Figure 3).
Further evaluation to identify underlying mycobacterial infection included interferon gamma release assay (IGRA), Ziehl-Neelsen stain and culture for acid-fast bacilli, and polymerase chain reaction (PCR) of skin lesions, all of which were negative. Bone scan revealed an insignificant mild inflammation in the sacroiliac joint.
The presumptive diagnosis of simultaneous PNT and EI was made based on the histopathological findings of skin lesions and clinical presentation. The empirical treatment with anti-tuberculosis agents started. This treatment included a combination of isoniazid (INH) 300 mg/day, pyrazinamide (PZA) 1500 mg/day, ethambutol (EMB) 1200 mg/day, and rifampin (RIF) 600 mg/day for two months, followed by a four-month-period of Isoniazid 300 mg/day and Rifampin 600 mg/day. Treatment led to significant improvement of the lesions after five months and no recurrence was observed during a two-year follow-up of the patient (Figure 1).
3. Discussion
First described by Darier in 1896, tuberculids encompass a heterogeneous group of immune-mediated cutaneous reactions caused by hematogenous dissemination of Mycobacterium tuberculosis or its antigens in individuals with intact cell-mediated immunity (1). There is an ongoing debate about the association of tuberculid with M. tuberculosis. Evidence in favor of this association includes a positive PPD test in individuals with tuberculids, evidence of present or previous tuberculosis infection, histopathological features mimicking cutaneous tuberculosis, positive PCR for Mycobacterium DNA in a number of lesions (which provides strong evidence in favor of this association), and favorable response to anti-tuberculosis drugs (3, 4). However, none of the aforementioned characteristics could be applied to all patients and the primary internal source of TB is usually absent in affected individuals (5).
Although rare, in some cases, multiple forms of tuberculids can coexist, among which the coexistence of PNT and EI has been sporadically reported in the literature (Table 1). This co-occurrence may represent a kind of vasculitis that involves the vessels of different sizes, followed by a delayed hypersensitivity reaction. While small superficial vessels are affected in the lesions of PNT, deep-larger vessels are the main sites of involvement in EI (6).
| No. of Patient / (Reference) | Age/Sex | Site of Skin Lesion | Underlying Tuberculosis Infection | PCR for Mycobacterium DNA | PPD | Drug/Duration | Response to Treatment |
|---|---|---|---|---|---|---|---|
| 1 / Yoshikawa et al. (7) | 43/F | PNT: extremities; EI: lower extremities | Pulmonary calcification + cervical and axillary lymphadenopathy | Not mentioned | Positive | PNT: H, S / 40 days; EI: H, R, S / 30 days | Good |
| 2 / Chuang et al. (8) | 32/M | PNT: chest, trunk, extremities; EI: Buttocks, legs, feet | Not found | Not mentioned | Positive | H , E , R / 9 months | Good response after 2 weeks; relapsed after cessation of treatment |
| 3 / Jordaan et al. (5) | 28/F | PNT: upper and lower extremities; EI: extremities | Inguinal lymphadenopathy | Not mentioned | Positive | H, E, R / 6 months | Good |
| 4 / Jordaan et al. (5) | 25/F | PNT: upper and lower extremities; EI: lower extremities | Not found | Not mentioned | Positive | H, E, R / 6 months | Good |
| 5 / Jordaan et al. (5) | 17/M | PNT: face, trunk, extremities; EI: lower extremities | Abnormalities in chest radiograph | Not mentioned | Positive | H, E, R / 6 months | Good |
| 6 / Wilson-Jones and Winkelmann (9) | 11/F | PNT: hands and feet; EI: calves | Not found | Not mentioned | Positive | Combination therapy | Good |
| 7 / Oon et al. (10) | 31/F | PNT: thighs and forearm; EI: shins and calves | Not found | Not mentioned | Positive | Not mentioned | Lost to follow up |
| 8 / Moon et al. (6) | 34/M | PNT: both arms; EI: legs | Cervical lymphadenopathy | Negative | Positive | H, R / 9 months | Good |
| 9 / Kim et al. (11) | 12/F | PNT: both extremities, buttocks; EI: lower extremities | Pulmonary tuberculosis | Negative | Positive | H, E, R, Z / 2 months; followed by H, R / 4 months | Good |
| Current case | 50/F | PNT: lower extremities; EI: lower extremities | Not found | Negative | Negative | H, E, R, Z / 2 months; followed by H, R / 4 months | Good |
Study Literature
A review of previous cases revealed that most affected individuals with PNT and EI were young women. The most frequent sites of involvement were lower extremities. PPD was positive in almost all previously reported cases and the patients responded favorably to anti-tuberculosis drugs (Table 1). Nevertheless, the negative PPD test in our patient could be due to the long-term inactivity of tuberculosis or immunosuppression due to chemotherapeutic drugs. A low detection rate of tuberculous foci in previous studies was in accordance with our case, which can be explained by inaccessible or deactivated mycobacterium infection (2). PCR is considered a sensitive diagnostic tool for detecting mycobacterium in tuberculid skin lesions but its sensitivity ranges in individual studies from 54% to 100% based on the immunity status of the patients, the number of bacilli in a lesion, and the method of PCR assay (12).
To sum up, the clinical presentation and histopathological correlation are still the mainstay modalities for the diagnosis of tuberculids. Here, we presented a case with no previous history of tuberculosis infection with negative PPD and PCR tests for M. tuberculosis. However, the diagnosis was further confirmed by her favorable response to anti-tuberculosis drugs.