1. Introduction
Echinococcal infection is a parasitic disease that caused by Echinococcus granulosus sensu lato complex. The disease had been reported from most of the countries and it has been estimated that there are one million patients with hydatidosis worldwide currently (1, 2).
Four species of the Echinococcus worm are responsible for the disease in the human, from which granulosus and multilocularis are the most prevalent and cause the cystic echinococcosis and alveolar echinococcosis (3).
Formation of the hydatid cyst following E. granulosus infection is an important health issue especially in South America, Central Africa and the Middle East regions (4).
The human contamination occurs following the ingestion of the parasite ova. The disease begins in the liver and then may contaminate the other organs including lungs and brain. Diagnosis will be made upon radiologic in combination with serologic findings (2, 5).
This article presents a middle-aged man who presents with chest pain and abdominal pain. Evaluations revealed coexistence of hepatic and pulmonary hydatid cyst which was complicated with rupture of the hepatic cyst and diaphragm.
2. Case Presentation
A 43 years old man presented to the Emergency Department with very severe pain in right hemithorax. He mentioned intermittent chest and back pain within the past week which was mild at first and did not change with physical activity. In the last 3 days, the severity and frequency of the pain had increased and it was accompanied with the pain in the right upper quadrant of the abdomen, which worsen by breathing and sitting position. The pain was started suddenly, just before presenting to the hospital, the pain became very severe in the right hemithorax following lifting a heavy box and was followed by dyspnea. The highest intensity of the pain was at the level of the fourth and fifth ribs. It was constant and did not change with exertion. He did not complain of nausea and sweating.
He had one clinic visit in 3 past days and was treated with NSAIDs which did not improve his symptoms.
His past medical history was unremarkable and he ignored smoking, drinking or using any drugs and medications.
His vital signs at the time of admission was as below:
Blood pressure: 100/60 mmHg, pulse rate: 92/minute, respiratory rate: 24/minute and body temperature from oral root: 37.7°C.
Physical examination of the chest was normal in perception and there was no evidence of trauma and ecchymosis. Auscultation of both lungs revealed decreased respiratory sounds in the right side. Percussion of the intercostal spaces was dull in right hemithorax which was suggestive of pleural effusion.
Physical examination of the abdomen revealed tenderness in palpation of the right upper quadrant. The rest of the examination was unremarkable.
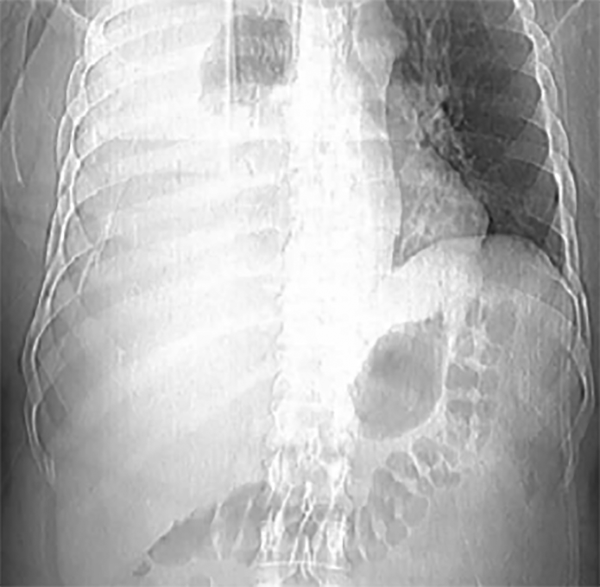
With regard to the chest pain and dyspnea along with findings of the physical examination, an upright chest X-ray was performed that revealed opacity of the right hemithorax due to pleural effusion (Figure 1). Diagnostic thoracentesis revealed an exudative pleural effusion which was indicating infections, malignancies, lymphatic abnormalities or endocrine disorders in differential diagnosis. The culture and cytology of pleural fluid was negative. A chest tube was inserted in right hemi-thorax to improve patient’s dyspnea.
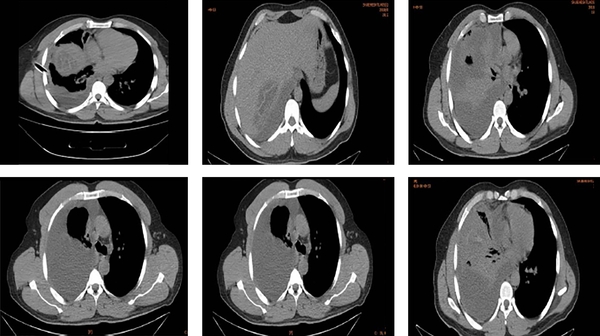
Abdominal ultrasound revealed a 75 × 39 mm heterogeneous mass in sub-diaphragmatic region of the liver which could be suggestive of an abscess. Thoraco-abdominal CT scan was performed for further evaluation of the mass which showed a hypodense mass in the right lobe of the liver, suggesting a liver hydatid cyst. Serologic tests for hydatidosis were negative (Figure 2).
The patient underwent surgery and a liver hydatid cyst with remnants of a ruptured cyst and a thoracic cyst were excised. Diaphragmatic rupture was restored. Samples were sent for pathological study and the diagnosis of hydatidosis was confirmed. The patient was discharged after surgery with good general condition. He underwent medical treatment with 400 mg albendazole twice a day for three 4 week cycles. He had no complications in follow up.
3. Discussion
The infection with E. granulosus is asymptomatic at the beginning. The cyst grows slowly in a spherical shape. It usually remains asymptomatic until it reaches a significant size. The most common site of cyst formation is the liver with an estimated prevalence of 67%, following with pulmonary cyst which accounts for 25% of cases. Although the prevalence of the pulmonary cyst, involvement of the chest and diaphragm is not common and its prevalence has been estimated 0.6% - 1.6% in previous studies with a mortality rate varying between 5.6% to 43.7% in different studies (6, 7).
More than 70% of patients present with a single cyst. According to the literature, multiple organ involvement with hydatid cyst is a rare occurrence. The mortality and morbidity rates in case of coexistence of liver and pulmonary cyst had been estimated 0% - 3% and 6% - 47% in the literature (7, 8).
The patient described above, had 2 cysts in the liver and a cyst in the chest, which is an uncommon occurrence.
The hydatid cyst will finally present as a space occupying lesion or rupture. Rupture of the cyst may occur spontaneously or following trauma. Liver cysts rupture into the peritoneal cavity in more than 60% of cases and lead to peritonitis. They also may rupture into the pleural cavity following perforation of the diaphragm and lead to pulmonary hydatidosis or bronchial fistula. Systemic symptoms, including anaphylactic reaction may be present following rupture of a hydatid cyst (9, 10).
Imaging techniques including computed tomography (CT) scan or magnetic resonance imaging (MRI) and serologic tests could be applied for the diagnosis. The definite diagnosis is based on the aspiration of the cyst to detect protoscoleces, but it is not advised to aspirate the cyst as it may lead to contamination of adjacent tissues and increases the risk of rupture and anaphylactic reaction (11).
Surgery is the treatment of choice in complicated cystic echinococcosis (including rupture, biliary fistula, cysts that compress vital structures and cysts causing infection or hemorrhage), However, Aribas et al. (7) introduce an old man with simultaneous ruptured hydatid cyst of liver and lung, who was treated successfully with percutaneous drainage, due to his poor general condition. In case of multiple daughter cysts, large cysts (greater than 10 cm in diameter) and extra-hepatic disease, surgery is the treatment method of choice too. Treatment with albendazole should be considered from one week before surgery and continue for four weeks after surgery to reduce the risk of seeding (12).
Other cases may be treated with percutaneous drainage and medical therapy.
In endemic regions, treatment of infected dogs and vaccination of sheep, may prevent the disease.
Atypical forms of the disease should be kept in mind as differential diagnosis in regions with high prevalence of echinococcosis.