1. Background
Hepatitis B is a common and serious viral infection in the world. Approximately 350 million people are chronic carriers of the virus leading to about 600,000 deaths annually (1). Hepatitis B infection is also a major public health problem because of its long-term complications such as chronic hepatitis, cirrhosis, and hepatocellular carcinoma (2). Hepatitis B virus (HBV) can cause fulminant hepatitis and lead to chronic carrier states after acute infection in about 10% of the cases. The HBV can survive at least one month on dry surfaces at room temperature, which provides an additional risk to acquire HBV infection. Before the introduction of the HB vaccine, HB infection was the most common occupational infection among hospital staff and laboratory and public safety workers following human blood or body fluid exposures (3).
Needle-stick injury is the most common source of HBV infection in health care workers. The World Health Organization (WHO) reports that before implementing the routine HB vaccination for health care workers, 6% - 8% of all HBV-infected individuals were hospital staff. This rate decreased to 3% - 4% after vaccination of health care workers, which indicates the importance of recognizing susceptible occupational groups and provide vaccination programs for them (4).
After the vaccination, anti-HBS rises in about 90% - 95% of vaccine recipients. Approximately 5% - 10% of the vaccinated individuals display inadequate response to the three standard doses of the HB vaccine at the schedule of zero, one, and six months. The percentage of such non-responders may vary depending on the type of vaccine used and the characteristics of vaccinated participants (4).
No response to the HB vaccine is high among certain groups such as smokers, diabetics, chronic renal failure patients, the elderly, and obese individuals (2, 5). The number of vaccinations has a significant role in the response to the HB vaccine (6).
To the best knowledge of the authors, the role of occupational factors in response to HB vaccine has not been addressed in any research.
2. Objectives
Thus, this study was conducted to assess the rate of antibody response in health care workers after the administration of three standard doses of HB vaccine including 20 µg of the recombinant HB vaccine, the rate of response to revaccination with additional doses of the HB vaccine in participants who had no response to primary standard doses of the vaccine, and the impact of occupational factors on the immune response to HB vaccine.
3. Methods
This cross-sectional study was carried out on health care workers at three large teaching referral hospitals of Iran during 2016 - 2018 who had referred to the occupational department for their medical surveillance. Hospital staff who were in direct contact with patients were enrolled in our study. All of the subjects were informed beforehand about the study. Demographic and occupational characteristics including age, gender, BMI, vaccination history, previous medical records, drug history, job category, shift work schedule, smoking, and previous history of needle-stick injury were determined for all the participants. They were all examined by a single physician and tested for CBC, TSH, FBS, lipid profile (triglyceride, cholesterol), BUN, creatinine, AST, ALT, hepatitis B surface antigen (HBsAg), anti-HBS, and anti-HCV-Ab (hepatitis C virus antibody) titers. Subjects with abnormal liver function tests, a history of significant hematological, hepatic, renal, and cardiac diseases, immune deficiency, or those who had received blood products within the past six months were excluded from the study. Eventually, 508 participants who had not the exclusion criteria and had not been vaccinated for hepatitis B before or had an unclear history for HB vaccination with HBS antibody titers < 10 mIU/L remained in the current study.
This study was approved by the Ethics Committee of Tehran University of Medical Sciences and the Helsinki Declaration was respected across the study.
We administered 20 µg of recombinant DNA HB vaccine to all the 508 participants at a schedule of zero, one, and six months. Then, six weeks after the third dose of injection, serum samples were obtained and tested for anti-HBs titers. Those who achieved anti-HBs titers < 10 mIU received the second series of HBV vaccination with three doses of the vaccine at a schedule of zero, one, and two months and rechecked for seroconversion six weeks later. Subjects were divided into good responders (HBs-Ab ≥ 100 mIU) and low responders (HBs-Ab < 100 mIU). The participants who showed anti-HBs titers of less than 10 mIU after the injection of the second series (total of six doses of the vaccine) were defined as non-responders.
Data analysis was performed by SPSS. Univariate analyses including the chi-square and independent-samples t-test to compare qualitative and quantitative variables, respectively. Finally, determinants univariately related to the HB immunity were entered into the logistic regression analysis (forward stepwise, likelihood ratio method). The P values of less than 0.05 were considered significant.
4. Results
A total of 508 participants were enrolled in the present study including 288 females (56.7%) and 220 males (43.3%) with a female/male ratio of 1.3. The mean age of the study subjects was 29.34 ± 5.22. In the meanwhile, 271 (53.3%) of the participants were nurses while 172 (33.9%) were service workers and the remaining 65 (12.8%) participants were medical doctors. Moreover, 174 (34.3%) of the subjects worked at critical units (i.e., emergency unit, CCU, ICU and operation room). Table 1 shows the baseline characteristics of the study population.
| Values | |
|---|---|
| Categorical Variables | |
| Gender | |
| Female | 289 (56.9) |
| Male | 219 (43.1) |
| Working shift | |
| Night shift | 101 (19.9) |
| Rotatory shift | 95 (18.7) |
| No shift | 312 (61.4) |
| Working unit | |
| Criticab | 144 (28.3) |
| Non-critical | 364 (71.7) |
| Job category | |
| Physicians | 65 (12.8) |
| Nurses | 271 (53.3) |
| Supportive | 170 (33.9) |
| Continuous Variables | |
| Age, y | 29.34 ± 5.22 |
| BMI | 25.72 ± 3.51 |
| Work experience, y | 11.43 ± 4.32 |
aValues are expressed as No. (%) or mean ± SD.
bCritical units: ICU, CCU, Operation Room, and Emergency Unit.
Six weeks after the injection of the final dose of primary series of the vaccine, 303 subjects (59.6%) showed anti-HBS levels ≥ 100 mIU (good responders) and 148 (29.1%) of them had anti-HBs levels ranging 10 - 99 (low responders). In addition, 57 (11.2%) of the participants achieved antibody levels below 10 mIU (hypo-responders). The mean level of anti-HBs titers following the third dose of the vaccine was 226.02 mIU/dL. A comparison of the characteristics according to the response level of the antibody is presented in Table 2.
| HBS Ab < 10 | HBS Ab ≥ 10 | P Value | Odds Ratio (CI 5%) | |
|---|---|---|---|---|
| Continuous Variables | ||||
| Age | 34.46 ± 6.74 | 28.69 ± 4.61 | 0.021 | |
| Working history | 11.35 ± 8.41 | 5.18 ± 5.63 | 0.552 | |
| BMI | 28.30 ± 2.88 | 25.39 ± 345 | 0.000 | |
| Categorical Variables | ||||
| Working shift | 0.001 | 0.440 (0.271 - 0.714) | ||
| Yes | 46 (23.5) | 150 (76.5) | ||
| No | 11 (3.5) | 301 (96.5) | ||
| Job category | 0.005 | 0.390 (0.223 - 0.681) | ||
| Nursing Group | 33 (12.2) | 238 (87.8) | ||
| Physician | 14 (21.5) | 51 (78.5) | ||
| Supportive Unit | 10 (5.8) | 162 (94.2) | ||
| Working unit | 0.000 | 1.23 (1.13 - 1.34) | ||
| Critical | 117 (81.2) | 27 (18.7) | ||
| General | 345 (94.8) | 19 (5.2) | ||
aValues are expressed as No. (%) or mean ± SD.
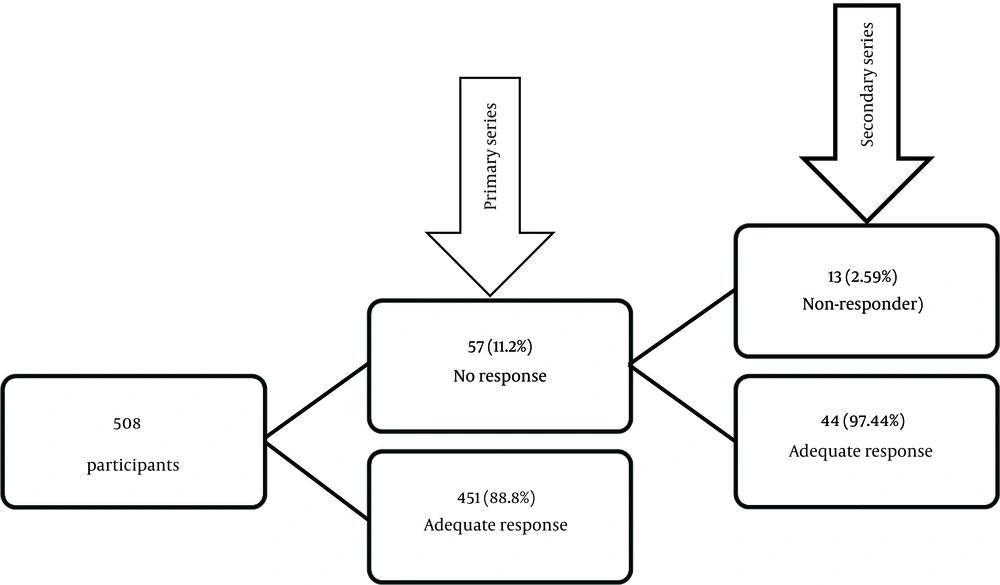
Those 57 subjects who did not respond to the initial series received additional three doses of recombinant vaccine (20 µg) of which, 77.19% (44 staff) achieved protective antibody titers (≥ 10 mIU). According to these results, 495 (97.44%) of the participants responded to the HB vaccine while 13 (2.56%) of them did not respond to the second series of vaccination and were considered as non-responders (Figure 1).
Moreover, 53.4% of shift workers were low responders after the first series of vaccination and 23.2% of them remained as non-responders after the second series, which was significantly higher than the rate in day workers (P = 0.001). The mean HBS antibody level in shift workers was 109.2 mIU/L whereas the average titer of HBS antibody in all participants was 299.5 mIU/L.
In addition, 28.6% of the subjects who worked in critical units had a low response to the HB vaccine, which was significantly higher than the rate in other staff (P = 0.004). The mean HBS antibody titer in this group was 171.23 versus 243.65 in the staff of non-critical units.
Finally, 21.5% of the physicians were low responders, which was significantly higher than in two other groups (P = 0.005) and the mean Ab level in this group was 195.04 versus 235.45 in nurses and service workers.
5. Discussion
In the current study, 97.44% of the participants developed seroprotection. This is in line with the results of some similar studies conducted previously (4, 6, 7). There was a significant association between some variables and a low response to the HB vaccine in this study. Shift work, working at critical wards, and job category (physicians) were all related to low immunity after hepatitis B vaccination in univariate analyses (Table 2).
In our study, 53.4% of shift workers were low responders and 23.2% of them were non-responders, which was significantly higher than the rate in day workers (P = 0.001). The mean anti-HBS level in shift workers was 109.15 mIU whereas the average titer of anti-HBS was 299.45 mIU in subjects with no shift work; it suggests that shift work significantly decreases the immune response to recombinant HB vaccine.
In a previous study conducted by Prather et al. (8) in 2010, it was indicated that sleep deprivation and shortening of sleep time had an impact on antibody response to the HB vaccine and decreased the level of antibody. In another study, Savard et al. (9) showed that chronic insomnia was associated with some immune alternations. Similarly, in a study by Cuesta et al. (10), it was unveiled that night shifts could disrupt the immune system function in humans. Savard et al. (9), in their study, demonstrated that chronic insomnia was related to lower counts of some lymphocyte subgroups such as CD3+, CD4+, and CD8+ cells and lower total lymphocyte count. Moreover, in another study conducted by Cuesta et al. (10), it was revealed that night shift disrupted circadian rhythms of the immune function and made changes in cytokine secretion. These effects of insomnia and night shift on the immune system function may justify the low response to HB vaccine in shift workers in the present study.
In this study, 28.6% of the subjects who worked in critical units had a low response to the HB vaccine, which was significantly higher than the rate in other staff (P = 0.004). The mean anti-HBS titer in this group was 171.23 versus 243.65 in the staff of non-critical units. These findings indicate that working in critical units may have negative effects on response to hepatitis B vaccination. This could be due to the impact of stress on the immune response to the HB vaccine, as indicated in some studies (11-13). Moreover, stress is common in people working in critical units because of high demands and low control (5). Because the effect of the working unit on response to HB vaccine has not been addressed in any other article according to our search, we suggest that more studies be conducted on this subject.
In our study, 21.5% of the physicians were low responders, which was significantly higher than the rate in the two other groups (P = 0.005). The mean Ab level in this group was 195.04 versus 235.45 in nurses and service workers. These findings indicate an association between job category and a low response to the hepatitis B vaccine, which has been addressed in no article in the literature.
5.1. Conclusions
In this study, in addition to well-known risk factors such as old age, diabetes, and smoking, the researchers found that other risk factors that may affect the immune response to HB vaccine include the working unit, job category, and shift work. These findings indicate that seroconversion after vaccination is a multifactorial condition and may be affected by occupational factors.
Based on the results of this study, it is proposed that to achieve an appropriate seroprotection in health care workers; it may be helpful to provide a suitable shift work schedule and reduce stressful situations for them. Shift workers, subjects who work in critical units, and physicians may need more protective measures in their occupational settings.
In every human attempt, no doubt, there exist some limitations that need to be acknowledged. Some hospital staff enrolled in this study had an unclear history of vaccination with anti-HBs levels < 10 mIU/L; they might be the persons who had complete vaccination and were non-responders. In this study, it was not possible to exactly evaluate shift workers to determine their sleep and waking cycles and determine if they had sleep deprivation, short sleep duration, or circadian rhythm disturbances. In addition, the researchers only found some associations between variables and immune response to the HB vaccine, so the causal relationship is limited in the present study.