1. Background
The most prevalent subtype of urinary incontinence in women is stress urinary incontinence (SUI). SUI can be treated minimally invasively using trans-obturator slings. The use of mid-urethral synthetic slings has revolutionized the management of female urinary stress incontinence (1). The goal of this procedure is to insert the mesh with minimal damage to the surrounding tissues via the obturator foramen (OF) and under the middle of the urethra. Concerns associated with trans-obturator tape (TOT) (2) include problems such as tape erosions (3), urethral lacerations (4), and vascular issues (5). Delorme noted that there is a risk of damaging the dorsal nerve of the clitoris, which runs along the medial portion of the ischiopubic ramus. This could potentially affect postoperative sexual functions, such as arousal, orgasm, or discomfort (6). The morbidity and need for re-operations to treat erosions make it a challenging experience for both the patient and the surgeon. To ensure the safe and effective completion of surgical procedures, a thorough understanding of surgical anatomy is essential. This is particularly crucial when novel surgical methods or tools that test the surgeon's knowledge of relevant anatomical features are developed (7).
According to anatomical understanding, the highly variable structures within the obturator region have the potential to cause significant issues and result in diverse treatment outcomes. This region holds clinical significance across various medical specialties, including radiology, orthopedic surgery, vascular surgery, abdominal surgery, and urogynecology. Understanding the topographical relationships among anatomical structures and variations within the obturator region is essential to prevent inadvertent harm (8).
The bone anatomy of the female pelvis exhibits considerable variability, and this variation can have a significant impact on sling surgeries. To successfully implant TOT and reduce morbidity, one must be aware of the anatomical structure of the pelvic floor (PF), pelvic organs (PO), and perineum (9). The trans-obturator approach avoids significant bowel and vascular problems as it does not reach the retropubic area. All of these minimally invasive slings are implanted without a direct endoscopic view of the anatomical structures (10). The most common consequences are leg or thigh discomfort, mesh erosion, and infection (6, 11). One challenge in sling installation today is the lack of a tailored strategy based on differences in pelvic anatomy (12).
Anthropometric analysis of the pelvis holds significant clinical and surgical value, especially when considering potential phenotypic variations among the world's population (13). While these measurements can be obtained from cadavers, the accuracy of such data is often questioned. However, the purpose of this anthropometric research is to define and compare the size of the OF and pubic arch using digital X-ray images in the Iranian southwestern population of women to enhance safety and efficiency in surgical procedures. These differences in pelvic anatomy should also be considered in the design of trocars by companies that produce trans-obturator kits.
2. Objectives
This report aims to reduce the highlighted complications encountered in these procedures.
3. Methods
3.1. Study Sample
The cross-sectional research conducted in this study spanned from October 2021 to September 2022. A convenience sample technique was employed to select 500 anteroposterior (AP) pelvic radiographs of adult women aged 18 to 80 from southwestern Iran, which were subsequently assessed. All radiographs were provided by Shahid Beheshti Hospital, affiliated with Abadan University of Medical Sciences in Abadan, Iran. Only participants with properly aligned radiographs of their OF, pubic symphysis, and inferior edge of the pubis were included in this study. Individuals with known musculoskeletal issues, pelvic fractures, previous orthopedic procedures, congenital deformities, and general bone conditions such as rickets were excluded from the study.
3.2. Measurements
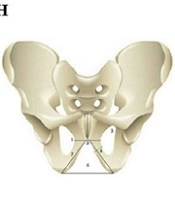
This study was conducted in accordance with the guidelines of the World Medical Association's Declaration of Helsinki and was approved by the ethical committee of Abadan University of Medical Sciences (approval number: IR.ABADANUMS.REC.1400.057). The measurements were obtained using conventional digital anteroposterior (AP) pelvic radiographs, with a distance of 100 cm between the film and the X-ray source. A skilled technician ensured proper subject positioning during radiography under strict supervision (14). To minimize measurement errors, two specialists independently performed each measurement. A pelviometric form was developed for the study, serving as the basis for assessing the linear, area, and angular characteristics of the pelvis. PACS software was employed to measure the points (Figure 1). These parameters included (15):
• Inter-obturator foramina distance: The shortest distance between OF (Figure 1A).
• Pubic symphysis length: The distance between the upper and lower pubic symphysis edges (Figure 1B).
• OF area: The region enclosed by the superior and inferior ramus (Figure 1C).
• Pubic ramus width: The distance between the farthest points on the side edges (Figure 1D).
• Pubic arch angle: The angle formed by the junction of these two lines on the inferior border of the pubic rami was measured (Figure 1E).
• Anterior urogenital triangle area: The area bounded by the pubic ramus as one of the triangle's two sides and an imaginary line as its base (Figure 1F).
• Pubic ramus length: The distance between the highest and lowest locations (Figure 1G) (white areas in radiographs)
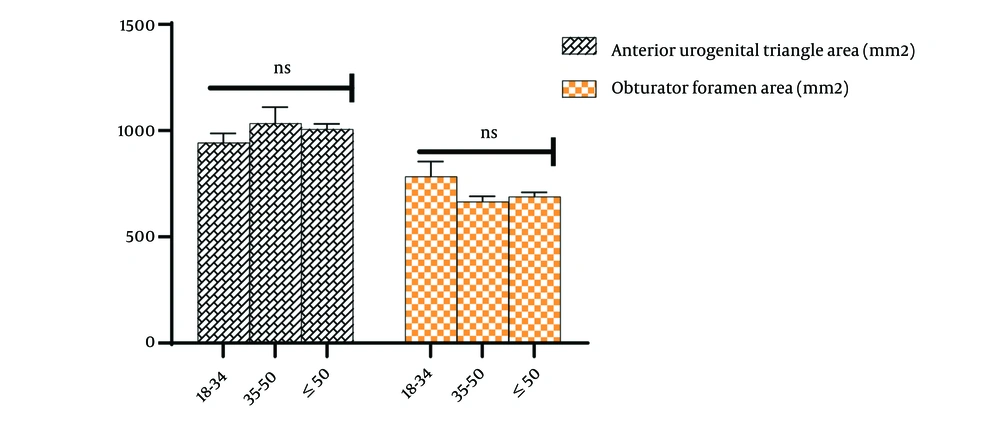
• All anthropometric parameters were illustrated on a schematic image (Figure 1H).
A, Measurements of Inter-obturator foramina distance; B, pubic symphysis; C, obturator foramen area; D, pubic ramus width; E, pubic arch angle; F, anterior urogenital triangle area; G, pubic ramus length in a plain X-ray of the pelvic bone in an adult patient; H, anthropometric parameters on a schematic image.
3.3. Statistical Analysis
STATA (version 14) was used to analyze all the data. The participants were categorized into three age groups: 18 - 34, 35 - 50, and above 50. The normality of each quantitative variable was assessed using the Shapiro-Wilk test. For parametric data analysis, the ANOVA test was utilized, while in non-parametric scenarios, the post-hoc test and the Kruskal-Wallis test were used. P-values less than 0.05 were considered significant.
4. Results
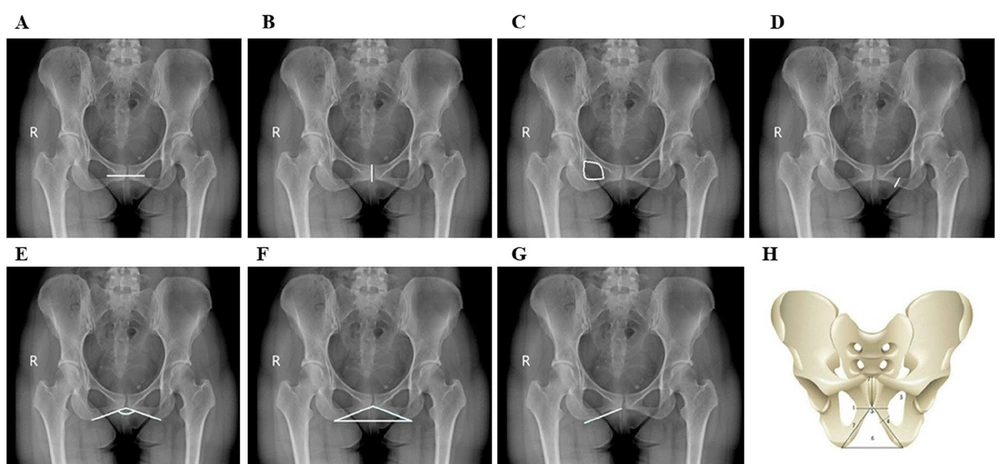
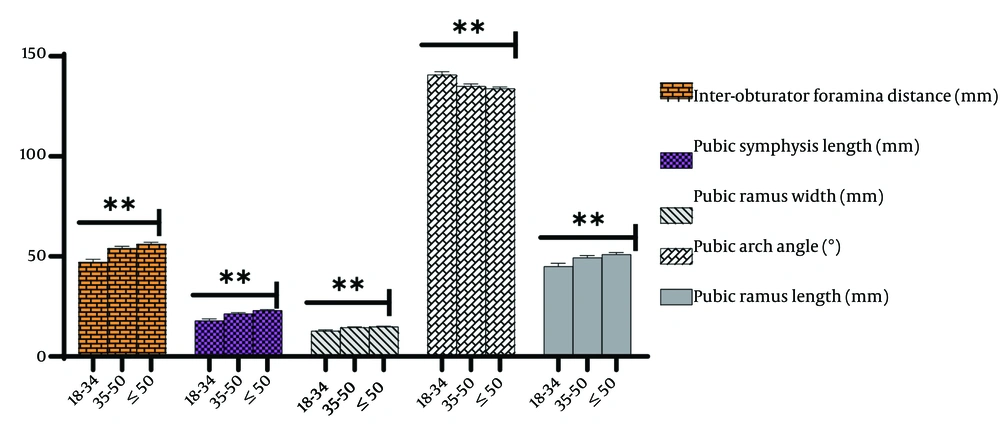
In this study, we employed 500 anteroposterior (AP) radiographs of adult women from the southwest of Iran, representing diverse pelvic morphologies. As depicted in Figures 2 and 3, we utilized indices of parameters related to the OF and pubic arch across three age groups: 18 - 34, 35 - 50, and above 50. Various age groups exhibited significant variations. We identified substantial differences based on the estimated indices of parameters related to the OF and pubic arch.
Specifically, when examining the inter-obturator foramina distance, we observed the following values: 18 - 34 = 47 mm, 35 - 50 = 53.9 mm, and < 50 = 56.1 mm, with a P-value of 0.001. For pubic symphysis length, we found 18-34 = 17.9 mm, 35 - 50 = 21.4 mm, and < 50 = 23 mm, with a P-value of 0.002. In the case of pubic ramus width, the measurements were 18 - 34 = 12.8 mm, 35 - 50 = 14.5 mm, and < 50 = 14.9 mm, with a p-value of 0.004. Finally, for pubic ramus length (mm), we observed 18-34 = 45.1 mm, 35-50 = 49.4 mm, and < 50 = 51.1 mm, with a P-value of 0.002. These measurements showed a significant increase with advancing age. However, the subpubic angle exhibited a significant decrease as age increased.
Regarding the pubic arch angle, we measured 18 - 34 = 140.8 mm, 35 - 50 = 135.1 mm, and < 50 = 133.9 mm, with a P-value of 0.001. In contrast, we did not observe a significant difference in the anterior foramen area (mm2) between the age groups, with measurements of 18 - 34 = 783.9 mm2, 35 - 50 = 665.8 mm2, and < 50 = 689.8 mm2, and a P-value of 0.07. Similarly, there was no significant difference in the anterior urogenital triangle area (mm2), with measurements of 18 - 34 = 943.5 mm2, 35 - 50 = 1034 mm2, and < 50 = 1006.4 mm2, and a P-value of 0.6.
5. Discussion
In this study, we assessed variations in anthropometric parameters of the OF and pubic arch among the female population in southwestern Iran. Our investigation revealed significant differences in the inter-obturator foramina distance, pubic symphysis length, pubic ramus width and length, and pubic arch. However, we found no significant difference between the OF area and the anterior urogenital triangle area.
When comprehensively analyzing the morphometric features of different shapes of the mature female pelvic bone, a wide range of variations in linear, area, and angular parameters, as well as OF size, have been reported. These variations may have implications for procedures using the transobturator approach. The superolateral aspect of the OF houses important vascular and neurologic structures within the pelvis, and the bony components of the obturator complex serve as a framework for these structures. Therefore, variations in its shape can influence the placement of transplanted prostheses in the surrounding tissues.
It is worth noting that measurements of the distance between the ischiopubic ramus and specific anatomic components within the OF in cadavers exhibited substantial variation. The distance between the midpoint of the ischiopubic ramus and the obturator canal ranged from 4.2 to 5.5 cm, likely influenced by the size and shape of the OF. This anatomical diversity aligns with findings from several other studies (16, 17).
In this study, we examined variations in anthropometric parameters of the OF and pubic arch within the female population of southwestern Iran. Our investigation revealed significant differences in the distances between the inter-obturator foramina, pubic symphysis length, pubic ramus width and length, and pubic arch. However, we did not observe any significant difference between the area of the OF and the area of the anterior urogenital triangle.
As age increases, there is a significant difference in the inter-OF distance, ranging from 47 mm to 56.1 mm, pubic symphysis length, ranging from 17.9 mm to 23 mm, as well as pubic ramus width, ranging from 12.8 mm to 14.9 mm, and length, ranging from 45.1 mm to 51.1 mm.
The results of the operations on women align with those reported in other studies. In research conducted by Whiteside and Walters on six recently deceased females (18), it was found that the posterior branch of the obturator nerve and the mesh in the TOT outside-in operation were separated by an average distance of 25 mm. Similarly, in a related investigation by Spinosa et al. (19) involving five recently deceased individuals in Switzerland, the posterior branch of the obturator nerve and the TOT mesh were reported to be separated by 27 mm. These findings are consistent with those of Achtari et al. (6).
Since the trocars used in trans-obturator mid-urethral slings and prolapse repair kits have fixed sizes and angles, the observed variability has significant clinical implications. While it remains unclear how the size and shape of the OF affect the location of blood vessels and nerves, it is possible that women with smaller OFs may be more susceptible to neurovascular injury resulting from these treatments (20).
The obturator internus muscle has a physical connection to the ischiopubic ramus, and the pubic arch angle determines the distance between the obturator internus muscle and the mid urethra. Several slings allow for mesh attachment to the obturator internus muscle without the need for trocars in the trans obturator or retropubic regions (20). The mean pubic arch angle ranged from 140.8 to 133.9° across various age groups. As women age, their anatomical pelvic dimensions undergo significant changes. In an anthropometric survey conducted in the capital of Iran by Akhlaghi et al., the mean subpubic angle in females was found to be 140.5°. While there might be some discrepancy due to the study's design focusing on the adult female population in southwestern Iran, both studies yielded nearly identical measurements (14). This finding closely aligns with previously reported subpubic angle measurements (21-23). The wide variation in pubic arch angles observed in our study could have implications for sling placement and tensioning. However, the acquired subpubic angle in the Iranian population was greater than previously reported (23-25). This difference might be attributed to various factors such as ethnicity, geography, regional differences, dietary habits, lifestyle, and age-related variables, as our study specifically focused on the adult female population in southwestern Iran. Additionally, substantial variations were observed among different age groups. While the subpubic angle significantly decreased with age, other characteristics like inter obturator foramina distance, pubic symphysis length, pubic ramus width, and pubic ramus length increased significantly with age. Previous research has also indicated this relationship, which is likely influenced by ethnic, dietary, and lifestyle differences. Future studies should further investigate this finding and consider it in clinical operations (14, 23, 26). Reports have highlighted differences between sexes and demographic groups in terms of the size and shape of the OF (20), the width of the ischiopubic ramus (27), and the subpubic angle (20, 28).
Females of African, American, and European descent exhibit significant differences in height, OF shape, and subpubic angle (20). In addition to population affinity, the role of height in these variations has been discovered. The authors have hypothesized that urogenital surgical procedures utilizing the transobturator approach may be influenced by the substantial variability of the OF in females, as well as the connection between the OF and subpubic angle with stature (20). Further research has unveiled a correlation between the width of the ischiopubic ramus, OF height and shape, and needle trajectory during transobturator surgeries (16).
Drawing upon American data as the gold standard, pelvic measurements from European populations were employed in the construction of the needles. The male transobturator tape (TOT) procedure was developed by Bauer et al. (29), the female TOT outside-in technique by Delorme (30), and the TVT (Tension-free Vaginal Tape) procedure was transformed into the TVT-O (Tension-free Vaginal Tape Obturator) inside-out approach by de Leval (14) in Belgium (29, 30). It is essential to bear in mind that anatomical differences have an impact on the efficacy of these stress urinary incontinence (SUI) techniques in South Africa. Therefore, it is advisable to conduct research aimed at standardizing needles for the adult female population in the southwestern region of Iran and validating their effectiveness in a clinical setting.
Utilizing radiographic osteometric measurements offers several advantages, including ease of use and applicability to living subjects (31). To validate the presented correlations, it is necessary to gain a deeper understanding of the functioning of the obturator muscles and the obturator membrane, as well as to explore the morphology of the paraurethral region. However, it's important to note that this study solely examined the bony component of the obturator complex through X-ray imaging, which constitutes a limitation of our research. Further investigations are needed to establish the clinical implications of these findings since this dataset lacked information related to medical history, parity, or pelvic floor issues (32).
Any surgical technique necessitates a comprehensive understanding of anatomical structures. Female pelvic bone anatomy exhibits significant variations, and these discrepancies can profoundly impact sling treatments. The findings indicate a robust correlation between anthropometric measurements of the obturator foramen (OF) and the pubic arch among women of varying ages. The transobturator method circumvents significant bowel and vascular complications as it does not extend to the retropubic region. All of these minimally invasive slings are implanted blindly, lacking direct or endoscopic visualization of anatomical features. Both manufacturers and healthcare professionals bear responsibility for the prudent adoption of emerging procedures and materials. Healthcare professionals should refrain from disseminating potentially misleading outcomes with limited follow-up.
Further research should replicate the study in a clinical setting where procedures like TOT and TVT-O, as well as operations requiring obturator nerve blocks, are routinely performed. The obturator nerve and its branches should be re-located, utilizing sonographic imaging on live subjects.