1. Context
COVID-19 is a systemic respiratory disorder caused by the SARS-CoV-2 virus. The acute respiratory syndrome of COVID-19 may manifest with mild to severe respiratory symptoms, multiple organ failure, and death (1). This disease started in China at the end of 2019, spread rapidly worldwide, and became a major health crisis (1). The WHO (World Health Organization) declared the COVID-19 disease a significant threat to physical and mental health (2). COVID-19 has caused various problems, such as fear of infection (3-5) and death anxiety (6). As a result, it has affected various physical, psychological, and even economic aspects of life (7). Fear, anxiety, mood changes, and depression are common in this disease, and depression (8) and mood disorders (9) are also prevalent. Anxiety is a very unpleasant and vague feeling accompanied by one or more physical symptoms such as shortness of breath, palpitations, sweating, headache, restlessness, and the urge to move. According to diagnostic guidelines and mental disorder statistics, anxiety is one of the most common mental health problems (10, 11). Anxiety disorder is also the most common clinical problem during childhood and adolescence, and approximately 5% of children and adolescents fulfill the diagnostic criteria for an anxiety disorder during childhood. More than 20% of people experience anxiety problems before the age of 16 years (12, 13). Therefore, childhood and adolescence are high-risk periods for developing anxiety. In addition, spontaneous recovery from anxiety symptoms is low in children and adolescents, presenting a continuous problem throughout the growth period (14-16).
During the COVID-19 pandemic, children and teenagers were assumed to be one of the most vulnerable groups in society (17). Quarantine inflicted many physical and psychological effects on children (18). In this context, several studies have investigated the psychological disorders of people during quarantine. The results of a study demonstrated that during the COVID-19 pandemic and after the closure of schools in China, more than 180 million students were quarantined at home. This restriction during the outbreak of COVID-19 caused symptoms such as anxiety and depression in children (19, 20). Ghosh et al.'s study showed that during the outbreak of COVID-19, children suffered from different psychological problems (21). Zhao et al. reported that children often had more behavioral and emotional problems during the COVID-19 outbreak due to forced isolation and closure of schools, reduced activities, and reduced communication with their friends and classmates (22). Also, during the pandemic, quarantine at home, exposure to domestic violence, and reduced opportunities for playing and entertainment severely affected children's mental health (23, 24). Compared to adults, children and adolescents are less severely affected by COVID-19, and most of them have mild symptoms and a good prognosis. Nevertheless, the disruption of family support, increased fear of losing dependents, and the death of a family member can lead to severe mental health problems in children, leading to changes in their adaptation capabilities and mood. This phenomenon provides the basis for stress, anxiety, depression, and even suicidal thoughts in children (25).
Children are one of the vulnerable groups in society, and their mental health problems, besides tourniquet complications and costs, can threaten the functioning of the family and society (26-28). Therefore, it is important to timely recognize stress and anxiety in children during disease outbreaks, such as the COVID-19 pandemic, so that families, professionals, and psychologists can implement effective preventive measures, educational plans, and therapeutic interventions. Already, various studies have examined the consequences of the COVID-19 disease and its mental health consequences in children. Therefore, the present systematic review aims to investigate the severity of depression, anxiety, and stress in children and adolescents during the COVID-19 pandemic.
2. Methods
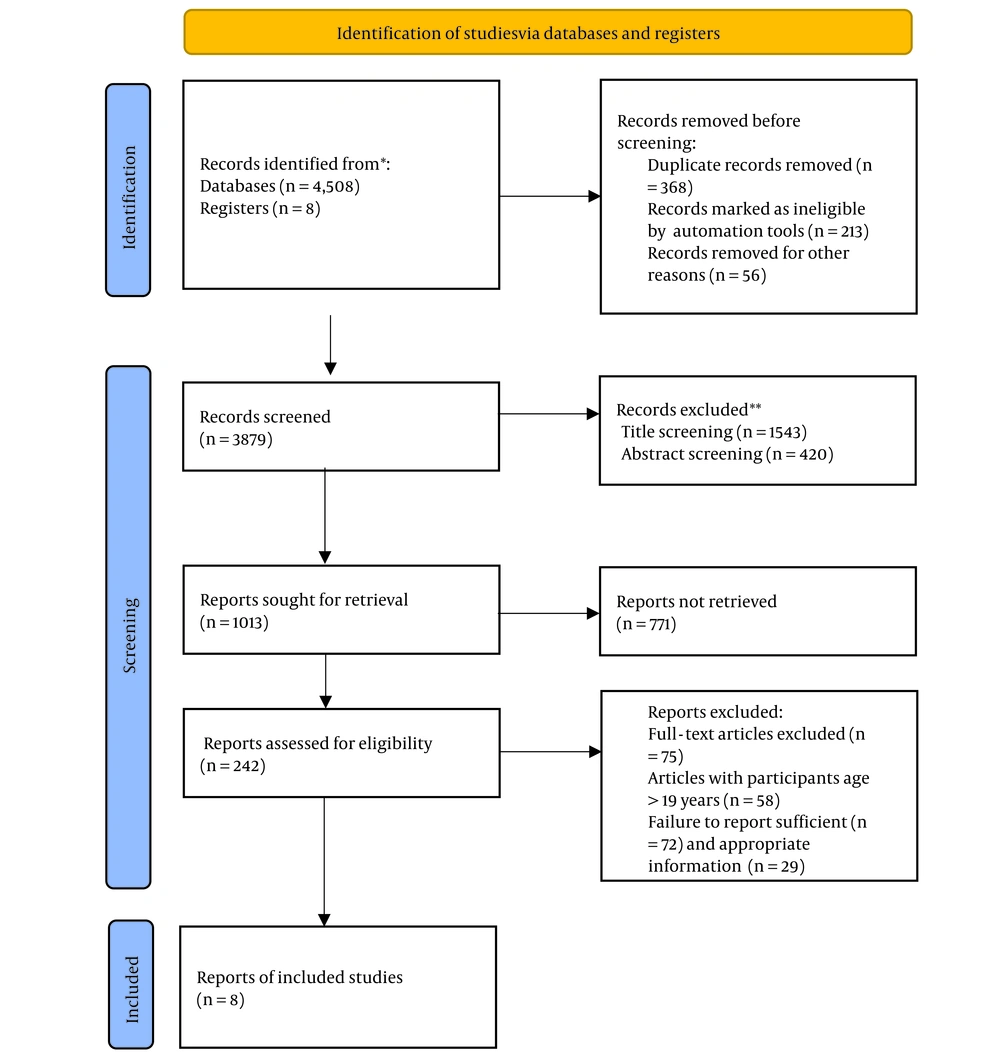
This systematic review was conducted and organized according to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyzes) guideline (29). We focused on quantitative studies published during the COVID-19 pandemic on changes in anxiety and depression in children and adolescents.
2.1. Data Sources and Search Strategy
A comprehensive electronic search was conducted in multiple databases from December 2019 to December 2021. The language was limited to English. The databases included Embase, Cochrane, PubMed, Web of Science, Scopus, and Google Scholar. We also applied the technique of "backward snowballing" to find other relevant articles (30) by reviewing the reference lists of the selected articles. Controlled vocabularies and keywords describing mental health problems of children and adolescents in the context of the COVID-19 pandemic were used for the search. In accordance with the topic of our study, the keywords that were searched included “depression”, “anxiety”, “children”, “adolescents”, and “COVID-19”. Each keyword was searched individually. In similar reviews or other meta-analyses containing these keywords, we checked if there were synonymous terms with different meanings. We then integrated these words into the search formula to extend the search scope. The following search syntax was used: (“Mental health” OR “mental illness*” OR “mental disorder*” OR “psychological illness*” OR “psychiatric disorder*” OR “depress*” OR “depressive disorder*” OR “depressive symptom*” OR “emotional depression” OR “affective disorder*” OR “mood disorder*” OR “anxiety” OR “angst” OR “nervousness” OR “hypervigilance” OR “social anxiety” OR “anxiety disorder*” OR “anxious” OR “overanxious disorder*”) AND (“adolescent*” OR “teenager*” OR “child*” OR “student*” OR “juvenile*” OR “school*” OR “teen*” OR “young” OR “youth*” OR “minors”) AND (“COVID-19” OR “coronavirus” OR “SARS-CoV-2” OR “cov-19” OR “2019-nCoV” OR “severe acute respiratory syndrome Coronavirus2”). Two authors (NK and MS) independently searched all six databases using the same syntax to ensure that no relevant studies were missed.
2.2. Inclusion and Exclusion Criteria
All survey studies investigating depression and anxiety in children and adolescents in the context of COVID-19 were included in this review. In accordance with the age definitions proposed by the WHO and the United Nations, we included people aged 0-19 years (children and adolescents) (31, 32). All types of survey data, including questionnaires and interviews, reporting the prevalence of depression or anxiety or reporting depression or anxiety scores in different countries were considered. There were no restrictions regarding the type of intervention, the comparison, or data analysis methods. Articles that exclusively reported data on participants older than 19 years, studies on populations with clinical conditions (patients with COVID-19 or other diseases), those unrelated to our epidemiological and clinical aspects of interest (i.e., psychological consequences), and studies not written in English were excluded.
2.3. Study Selection and Data Extraction
Two authors (MA and FM) independently reviewed the titles and abstracts of all publications and read their full text for qualification. The information of each study, including the first author’s name, country, publication date, population under study, study design, sample size, age, interventions, type of depression or anxiety, and outcomes, was extracted and recorded into a password-protected Microsoft Excel spreadsheet. If the two researchers disagreed, a third party (the lead researcher, MS) intervened in the discussion and resolved any disagreement. When articles presented results from the same study, we selected those that reported outcomes that most closely matched our eligibility criteria. We also carefully reviewed the references of the included studies to find potentially relevant research.
2.4. Quality Assessment
The quality of the studies was assessed using a 14-item quality assessment tool presented in the National Heart, Lung, and Blood Institutes (NHLBI) study for observational cohort and cross-sectional studies (33). These items included the statistical power of the study, the strength of the causal relationship between the exposure and outcomes, and the potential risk of selection bias, information bias, measurement bias, or confounding bias. The studies were then categorized as high, moderate, or low quality, and the overall rating of each study was determined (see Appendix 1 in the Supplementary File).
2.5. Data Synthesis
In order to ensure accurate reporting, we followed the PRISMA checklist in this review. Given the diversity of the data from the initial studies, we created descriptive summary tables using Microsoft Excel version 2016 (Microsoft Corp, Redmond, WA, USA) to provide a concise overview of the literature.
3. Results
We identified 4,516 potentially relevant articles. After removing duplicates and irrelevant records, 3,879 articles remained. After screening titles and abstracts, we excluded 3,871 articles due to the lack of fulfillment of inclusion criteria in at least one of the following steps: (1) Title screening, (2) abstract screening, and (3) retrieving of results. When reading the full text of the remaining 242 articles, 75 papers were removed for not having useful data, 58 for being conducted on participants older than 19 years, 72 for reporting insufficient data, and 29 for insufficient information. Ultimately, 8 eligible studies were selected to be comprehensively reviewed here. The screening process is summarized in a PRISMA 2020 flowchart (Figure 1).
The results of all studies that met the inclusion criteria were carefully reviewed. A summary of the content of these articles is provided in Table 1. The objectives, measurements, and conclusions of these studies are summarized in Table 2.
The selection procedure is shown in the PRISMA 2020 flowchart. It is recommended, if possible, to specify the number of records identified from each individual database or register searched and not the total number from all databases or registers. If automation tools were used, it is also important to indicate the number of records excluded by humans and the number of records excluded by automation tools. This information was taken from (34, 35). Further details can be found at: http://www.prisma-statement.org.
| Authors | Year | Country | Design | Ethics Approval | Informed Consent | Sample Size | Population | Age, y | Results | |
|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety | Depression | |||||||||
| Giannopoulou et al. (36) | 2020 | Greece | Cross-sectional | Yes | Yes | 442 | High school students | Senior high school students (SHSS) | 10.59 ± 5.79 | 13.59 ± 7.25 |
| Burdzovic Andreas and Brunborg (37) | 2020 | Norway | Longitudinal | Yes | Yes | 915 | Adolescents students | 8th - 10th grade | 8.58 ± 7.41 | |
| Belanger et al. (38) | 2020 | Canada | Longitudinal | Yes | Yes | 2099 | Students in grades 9th - 12th | 14.1 ± 1.0 | 6.23 ± 5.44 | |
| Black et al. (39) | 2020 | United States | Cross-sectional | No | Yes | 362 | Children under the age of 18 years | 10.68 ± 2.28 | 12.02 ± 5.13 | |
| Westrupp et al. (40) | 2020 | Australia | Cross-sectional | Yes | Not report (NR) | 2,365 | Children aged 0 - 18 years | 8.66 ± 5.14 | 3.04 ± 2.65 | 5.04 ± 12.35 |
| Mayne et al. (41) | 2020 | United States | Cross-sectional | No | No | 47,684 | Adolescents aged 12 - 21 years | 15.3 ± 2.1 | 10,929 (22.92) | |
| Gladstone et al. (42) | 2021 | United States | Longitudinal | Yes | Not report (NR) | 228 | Adolescents in 7th, 9th and 11th grades | 14.5 ± 1.60 | 4.37 ± 4.88 | |
| Jolliff et al. (43) | 2021 | United States | Cross-sectional | Yes | Yes | 134 | Teenagers aged 13 - 17 years | 15.2 ± 1.4 | 5.37 ± 5.18 | 5.27 ± 5.06 |
a Values are expressed as mean ± SD or No. (%)
| Authors | Study’s Aims | Measurement Tools | Conclusions |
|---|---|---|---|
| Giannopoulou et al. (36) | Investigating how the nationwide lockdown affected anxiety and depression in high school students preparing for the upcoming national college entrance exams in Greece. | Anxienty (GAD-7), Depression (PHQ-9) | The surprisingly high levels of anxiety and depression required immediate action to address and manage students' mental health issues in future pandemic outbreaks. |
| Burdzovic Andreas and Brunborg (37) | Investigating the self-reported mental and physical well-being of adolescents in Norway before and during the pandemic and the health impact of pandemic-related anxiety. | Depression (PHQ-9) | The adolescents in the group affected by COVID-19, who felt very anxious due to the pandemic, were much more likely to have poorer mental and physical health compared to the pre-pandemic period. |
| Belanger et al. (38) | Assessing the impact of the initial response to COVID-19 on adolescents' mental well-being and general health in a real-world study. | Anxiety (GAD-7) | The early phases of COVID-19 lockdown measures had no negative impact on the mental health of young people. The decline in mental well-being during the first COVID-19 wave was not as bad as the decline before the pandemic. |
| Black et al. (39) | Investigating the impact of COVID-19 on the relationship between depressive symptoms and irritability in children and their parents. | Depression (MFQ-A) | Stress caused by COVID-19 was associated with higher levels of symptoms in parents and children, and it was suggested that family dynamics could play a role in interactions between these symptoms. |
| Westrupp et al. (40) | To examine trends in parents’ and children’s (0-18 years) mental health, parental substance use, marital conflicts, parenting practice, and family dynamics during COVID-19 compared to pre-pandemic data and to identify families that were particularly vulnerable to negative outcomes caused by demographic and individual factors as well as stressors caused by COVID-19. | Anxiety (SCAS), Depression (MFQ) | When it comes to children's mental health, existing parental health problems and the psychological and environmental stress caused by COVID-19 were repeatedly linked to increased anxiety and depression symptoms in children. This was observed in cases where the child was diagnosed with ADHD or ASD. |
| Mayne et al. (41) | Explaining changes in screening, signs of depression, and suicide risk in teenagers during the COVID-19 pandemic. | Depression (PHQ-9) | Depression and suicidal thoughts increased among female teens during the pandemic, underscoring the need for regular screening for depression and suicidal thoughts, as well as for consistent mental health monitoring of this population. |
| Gladstone et al. (42) | To investigate how the COVID-19 pandemic affected the depressive feelings of a group of young people and to examine the relationship between the stress caused by COVID-19 and factors that make them more or less vulnerable to depression, and how these factors contributed to changes in depressive symptoms over time. | Depression (PHQ-8) | The study investigated how major negative life events could influence the risk of depression in adolescents in their future lives. Because depression can have lasting effects on adolescents and because negative life events during adolescence can predict depression risk in adulthood, it is important that mental health professionals and school personnel be alert to the potential rise in depression in adolescents during the pandemic. |
| Jolliff et al. (43) | Comparing the levels of depression and anxiety in two groups of teenagers in the United States before and during the COVID-19 pandemic and examining the correlation of demographic factors and daily activities with depression and anxiety. | Anxienty (GAD-7), Depression (PHQ-8) | Adolescents who were part of the pandemic group or for whom the pandemic led to changes in their daily activities did not show higher levels of depression or anxiety. However, it was found that adolescents from less privileged backgrounds had significantly higher levels of anxiety during the pandemic than their more advantaged peers. It is important to offer low-income young people both practical support and psychological help. |
Abbreviations: GAD, general anxiety disorder-7; PHQ, Patient Health Questionnaire-9, MFQ, Mood and Feelings Questionnaire, SCAS, Spence Children's Anxiety Scale; ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; SES, socioeconomic status.
The spread of the COVID-19 disease nurtured psychological consequences and anxiety in children and adolescents. The review of the studies conducted in this field showed that the most important consequences were as follows.
3.1. Behavioral and Emotional Problems
The closure of schools, quarantine at home, fear of contracting the COVID-19 infection, and lack of communication with classmates decreased physical activities and social interactions of children and adolescents. Almost all these events cause or intensify behavioral and emotional problems in children and adolescents (37, 44).
3.2. Anxiety and Stress
In epidemics like COVID-19, fear of disease, death, and disruption in daily functioning cause anxiety due to fear of contagious diseases. The spread of the COVID-19 disease and continuous quarantine rules overexposed families to sad pandemic news and children and teenagers to fear and anxiety. The fear of losing parents, the rapid spread of the disease, the fear and anxiety of contracting the disease, as well as the fear of a painful death were mentioned in studies (45). According to studies (39, 40, 44, 46-48), COVID-19 has a high prevalence and increases stress and anxiety in parents and families.
3.3. Depression and Suicidal Thoughts
Concerns over depression and suicidal thoughts increased during the pandemic, especially among female teenagers. The high and unexpected rise in the prevalence of anxiety and depression requires an urgent solution to reduce harm and ensure students' mental health in the next epidemic crises. Studies suggest continuous screening for depression and suicidal thoughts among adolescents and high school students is a crucial task (36, 41).
3.4. Abuse and Emotional Abuse
The relationship between parents and children is crucial for creating safety and affection. The closure and bankruptcy of some businesses at the peak of the outbreak created many economic problems for some families, causing family disputes and increasing tensions and arguments in families, which would often lead to the mistreatment of children (49). Economic problems and family conflicts can affect the interaction between parents and children (50). Therefore, the more severe the psychological problems of parents, such as anxiety and stress, the higher the risk of behavioral disorders, such as aggression and anxiety, in children (21).
3.5. Depression and Post-traumatic Stress
Being quarantined at home during the COVID-19 outbreak was traumatic for many children and teenagers and might have led to loneliness and depression in this sensitive society group. Children and adolescents who lose a family member due to COVID-19 show the symptoms of post-traumatic stress or acute stress (42, 48).
Most studies have reported the adverse effects of COVID-19 on the mental health of children and adolescents. However, some studies also argued that neither being inflicted with COVID-19 disease nor experiencing changes in daily activities due to COVID-19 disease was associated with the exaggeration of depression or anxiety compared to before the pandemic. However, we found that young people with a lower socioeconomic status (SES) were more anxious during the pandemic than their peers with a higher SES. According to these results, instrumental and psychological interventions are necessary for low-income teenagers (38, 43).
4. Discussion
The present systematic review aimed to determine the severity of depression and anxiety in children and adolescents under 19 years of age during the outbreak of COVID-19. The current study demonstrated that COVID-19 could be associated with increased depression, anxiety, and stress among children and adolescents. The results of this research align with the findings of a review study by Viner et al. (51), who reported that the closure of schools increased psychological problems in children and adolescents (51). In this context, mental health support and similar interventions seem necessary. The results of various studies showed that in critical and emergency conditions, such as the coronavirus epidemic, the effects of the disease not only cause mental health problems in children and adolescents but also lead to persistent negative emotions (22, 52-55). Also, during disease outbreaks, the resultant economic and social consequences and financial damages to families will cause many problems for society and families, leading to fear, tension, frustration, and anxiety (17, 24, 56).
Generally, various studies indicate that children and teenagers are less vulnerable than adults to COVID-19 (57), but psychologically and socially, this group is more vulnerable than adults (58-60). Fear of illness, excruciating death, rumors, interruption in daily activities, prohibitions or restrictions on travel and commute, financial problems, limitation of social interactions, psychological burden and pressure on families, lack of playing during home quarantine, staying away from the school, lack of communication with friends and classmates, having no entertainment, and domestic violence all threaten the mental health of children and teenagers (57-63). Among the most common psychological consequences were the stressful situation caused by the COVID-19 disease and the lack of information about effective and efficient treatments, exaggerating anxiety (11, 64, 65).
Strengths and limitations: One of the strengths of this review was that the eight papers analyzed included more than 54,000 children and adolescents aged 0 - 19 years in five countries worldwide. They provided data on various mental health issues and evaluated changes in mental health before and after the pandemic. However, this study also had some limitations. Due to variabilities in study designs and mental health outcomes, no meta-analysis was performed. In addition, only peer-reviewed English-language papers were included, excluding studies in other languages. Although eight studies were included, only one presented a representative population-based data set, limiting the assessment of anxiety and depression on a larger scale. In addition, there were few studies on children under the age of ten years, making the extrapolation of findings to this age group difficult. Finally, all reviewed studies focused on changes in the early phase of the pandemic, so future research should focus on the impact of later waves of the pandemic on the mental health of children and young people.
4.1. Conclusions
Several survey studies have shown a strong link between the COVID-19 pandemic (and its consequences, such as social distancing, quarantine, and school closure) and mental health problems in children and adolescents. Anxiety, depression, stress, loneliness, and tension have been frequently reported. It is crucial to urgently apply positive coping strategies and provide family and social support to these individuals, as recommended in clinical practice guidelines. However, existing evidence is limited, and there is a need for more comprehensive studies, including intervention-based research, on this topic.