1. Background
The coronavirus was first reported in December 2019 in Wuhan, China. Many patients were diagnosed within family clusters, often experiencing psychological trauma related to witnessing the severe illness or death of close family members (1). These experiences can significantly damage the mental health of survivors and increase the likelihood of post-traumatic stress disorder (PTSD). The COVID-19 pandemic has affected individuals, families, and communities in various ways, with stressors potentially increasing the number of people experiencing PTSD symptoms. Those with pre-existing PTSD may also encounter more severe symptoms (2).
In addition to physical and physiological discomfort, COVID-19 has caused psychological challenges, such as mental disorders stemming from the fear of transmitting the virus, loneliness, insomnia, home quarantine, reduced social interactions, uncertainty, stigmatization, and disruption of daily routines. These factors altered the normal lives of families, affecting their lifestyles in significant ways (2). As the disease progressed, both the clinical symptoms and psychological issues of COVID-19 patients became more pronounced, with many experiencing anxiety and depression even after physical recovery and hospital discharge (2).
The uncertainty surrounding the disease has heightened fear and anxiety, causing considerable damage to individuals' physiological health. Notable mental health impacts include post-traumatic stress, depression, anxiety, panic disorders, and behavioral changes. Contributing factors include separation from family, loneliness, misinformation from social media, financial insecurity, and the loss of loved ones. Post-traumatic stress disorder is a severe psychological condition that may develop after exposure to traumatic or terrifying events, with core symptoms such as intrusive re-experiencing of the incident, avoidance behaviors, and negative changes in cognition, along with auditory disturbances like continuous ringing in the ears.
Numerous studies have demonstrated the widespread and diverse psychological effects of the pandemic, including anger, distress, and PTSD symptoms, which are linked to prolonged quarantine, fear of infection, hopelessness, potential shortages of basic necessities, insufficient information, economic challenges, and stigmatization (3, 4).
In a study conducted by Chama et al., it was found that preventive actions and restrictions, such as quarantine and social distancing, not only led to economic losses but also contributed to an increase in mental health issues, including PTSD, among groups such as COVID-19 survivors, the elderly, and healthcare workers (5). During the COVID-19 outbreak and pandemic, providing psychiatric services and paying attention to mental health is not only a moral imperative but also a crucial health goal. This is particularly important because patients with such infections often experience high levels of psychiatric problems, and neglecting these issues increases societal vulnerability to the consequences of the COVID-19 pandemic (6).
Post-traumatic stress disorder is a syndrome that occurs after experiencing, witnessing, or being involved in a highly traumatic event. The reaction to such experiences is often accompanied by fear and helplessness, with the event being relived repeatedly in the individual's mind. The person may try to avoid remembering the trauma. The severity and frequency of PTSD symptoms depend on the intensity of the event, and chronic exposure to stress can be a significant factor in the development of PTSD (7). Post-traumatic stress disorder is characterized by symptoms such as mental preoccupation, avoidance behaviors, and heightened arousal, which may include intense psychological distress and physical reactions like sweating, palpitations, and dry mouth when recalling the trauma. Additionally, individuals may experience difficulties with sleeping, irritability, and trouble concentrating. Post-traumatic stress disorder is diagnosed when these symptoms persist for at least one month.
A study conducted in Iran revealed that more than 50% of participants experienced moderate to severe anxiety. In another study, the prevalence of moderate to severe depression, anxiety, and stress was reported as 47%, 46%, and 32%, respectively (8).
The prevalence of PTSD is influenced by the severity, duration, and proximity of the traumatic event. Certain types of traumas, such as physical or sexual abuse and exposure to war, are strongly associated with the development of PTSD. Post-traumatic stress disorder can lead to a range of reactions, including emotional numbness, indifference, helplessness, severe bitterness, and irritability. These reactions can also result in several mental health issues, including intense feelings of anger and impatience, dissatisfaction with life, guilt, shame, and social distrust (9).
2. Objectives
Therefore, this study was conducted to examine the prevalence of PTSD among COVID-19 survivors, given the importance of mental health and the significant effects of the COVID-19 pandemic on psychological well-being.
3. Methods
This research is applied and descriptive-cross-sectional in terms of data collection and analysis. The statistical population consists of 97 patients from hospitals affiliated with the Abadan Faculty of Medical Sciences, selected through cluster sampling. The data for this study was collected using the Mississippi Questionnaire, a tool for assessing PTSD. This self-report scale, developed by Kian et al. in 1988, contains 35 questions, with responses rated on a 5-point Likert Scale. The total score range is from 35 to 175, where a score of 35 to 70 indicates mild PTSD, 71 to 106 indicates moderate PTSD, and a score of 107 or higher suggests the presence of PTSD. The Cronbach's alpha coefficient for this test has been reported in the range of 0.86 to 0.94 (10). In Beshrpour et al.'s research on the effectiveness of cognitive processing therapy on improving post-traumatic symptoms, quality of life, self-esteem, and marital satisfaction among women affected by marital infidelity, the test showed a Cronbach's alpha of 0.79. The Mississippi Scale demonstrates high validity and correlates well with other PTSD evaluation tools (11).
This scale was validated in Iran by Godarzi, where the Cronbach's alpha coefficient was reported as 0.92. To establish concurrent validity, correlation coefficients were calculated using three instruments: The life events list, PTSD list, and Padua list. The correlation of the Mississippi Scale with these instruments was reported as 0.23, 0.82, and 0.75, respectively (12).
Based on an article studying the prevalence of PTSD among firefighters in Isfahan, where the event impact scale was σ2 = 14.46 and the error value was 2.892 with a confidence level of 95%, the sample size was determined to be 97 using the sample size formula.
Inclusion criteria for the study were: At least one infection with COVID-19, no vaccination, and no use of anti-anxiety or antidepressant drugs. Exclusion criteria included incomplete questionnaire responses.
After obtaining ethical approval from Abadan University of Medical Sciences, the hospitals affiliated with the university were visited to collect patient contact information. Patients were contacted, and if they agreed to participate, a link to the consent form was sent. After confirming their consent, the link to the questionnaire was shared electronically, and patients were requested to complete and return the questionnaire. For those who were illiterate or did not have the required application to receive the link, the questionnaire was administered over the phone.
4. Results
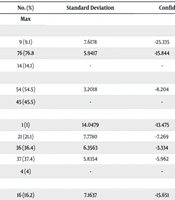
The results indicated that 54.5% of the participants were male and 45.5% were female, with 70% of the subjects being married. The average age of the participants was 42 years (standard deviation not specified). A researcher-designed questionnaire was used to collect demographic information, including age, gender, marital status, education level, occupation, number of children, and history of physical and psychiatric illness.
The majority (76%) of participants fell within the 25 - 64 age range. More than half (54%) of the subjects were male. Additionally, most of the participants were married (70%) and 22% had two children. In terms of education, the largest proportion (37%) of participants had a bachelor's degree, and 42% were employed. As shown in the Table 1, approximately half of the participants reported no history of physical illness (45%) or mental-psychological illness (41%).
| Parameter and Group | No. (%) | Standard Deviation | Confidence Interval 95% | P-Value | |
|---|---|---|---|---|---|
| Min | Max | ||||
| Age | 0.172 | ||||
| < 25 | 9 (9.1) | 7.6178 | -25.335 | 4.526 | |
| 25 - 64 | 76 (76.8 | 5.9417 | -15.844 | 7.447 | |
| 65 > a | 14 (14.1) | - | - | - | |
| Gender | 0.547 | ||||
| Male | 54 (54.5) | 3.2018 | -8.204 | 4.347 | |
| Female a | 45 (45.5) | - | - | - | |
| Degree | 0.317 | ||||
| Un-educated | 1 (1) | 14.0479 | -13.475 | 41.592 | |
| Lower than diploma | 21 (21.1) | 7.7780 | -7.269 | 23.221 | |
| Diploma | 36 (36.4) | 6.3563 | -3.334 | 21.582 | |
| Bachelor | 37 (37.4) | 5.8354 | -5.962 | 16.913 | |
| Postgraduate diploma a | 4 (4) | - | - | - | |
| Marital status | 0.822 | ||||
| Single | 16 (16.2) | 7.1637 | -15.651 | 12.430 | |
| Married | 70 (70.7) | 5.7612 | -14.766 | 7.818 | |
| Widow | 8 (8.1) | 8.3570 | -19.554 | 13.204 | |
| Divorce | 5 (5.1) | - | - | - | |
| Job | 0.507 | ||||
| Housekeeper | 25 (25.3) | 4.6765 | -6.059 | 12.272 | |
| Self-employment | 14 (14.1) | 5.1506 | -5.490 | 14.700 | |
| Employee | 42 (42.4) | 4.7503 | -4.249 | 14.372 | |
| Retired | 9 (9.1) | 8.0837 | -7.974 | 23.713 | |
| Other a | 9 (9.1) | - | - | - | |
| History of physical disease | 0.991 | ||||
| Yes | 45(45.5) | 2.6137 | -5.735 | 5.801 | |
| No a | 54 (54.5) | - | - | - | |
| History of mental illness | 0.631 | ||||
| Yes | 41 (41.4) | 1.1339 | -3.869 | 6.376 | |
| No a | 58 (58.6) | - | - | - | |
a The reference group.
Table 2 presents the average PTSD scores as mean ± standard deviation for the study participants. The average PTSD score was 104.12 ± 10.84. No participants were in the "no effect" group, 51.5% were in the "moderate impact" group, and 48.5% were in the "severe impact" group. The Cronbach's alpha value for the PTSD scale was 0.549.
| PTSD | Low (PTSD ≤ 70) | Moderate (70 < PTSD < 105) | Severe (PTSD ≥ 106) |
|---|---|---|---|
| 0 (0.0%) | 51 (51.5%) | 48 (48.5%) | |
| Mean ± SD | 104.12 ± 10.84 | ||
Abbreviation: PTSD, post-traumatic stress disorder.
The regression results in Table 1 indicate a direct relationship between PTSD and age, with older individuals reporting more psychological effects. However, this relationship was not statistically significant (P = 0.480). The PTSD score was higher in men compared to women. Additionally, participants with lower levels of education reported higher levels of PTSD. Married individuals showed a higher rate of PTSD compared to others, and retired participants had higher PTSD scores than those in other occupations. No statistically significant relationship was found between PTSD and variables related to physical or mental illness (P < 0.05).
5. Discussion
The purpose of this study is to investigate the prevalence of PTSD in patients who have recovered from COVID-19. According to the results, 51.5% of the participants reported a moderate level of PTSD, while 48.5% reported a severe level, indicating a high overall prevalence. In a study conducted by Wang et al. (13) on the general population in China, 53.8% of participants rated the psychological effects of the COVID-19 pandemic as moderate to severe, which aligns with the findings of this study. Similarly, another study examining the impact of the Ebola outbreak on mental health in Sierra Leone found that symptoms of PTSD and anxiety-depression were still prevalent one year after the epidemic was contained, with 48% reporting anxiety-depression symptoms and 76% experiencing PTSD (14). Sim et al.'s study on the psychological effects of the SARS outbreak in Singapore revealed that nearly a quarter of the study population had symptoms of PTSD (15).
Research on mental health following outbreaks of infectious diseases like SARS, MERS, Ebola, influenza, and AIDS has shown that while many mental health problems diminish once the epidemic subsides, PTSD symptoms may persist long after, leading to disability and significant distress (16). Therefore, this issue requires greater attention. The demographic data from this study also suggest that individuals with lower education and income levels are at a higher risk of developing PTSD. Studies show that after infectious disease epidemics, survivors often report the highest prevalence of PTSD (17).
One limitation of this study is its cross-sectional design and the loss of some samples during the study. To address this, the treatment willingness analysis method was employed. Further research is recommended to explore the chronic course of PTSD symptoms and their prognosis. Given the increasing number of individuals at risk of contracting COVID-19, it is crucial to provide mental health services aimed at preventing PTSD in survivors and other at-risk groups. These measures could include psychoeducation, screening for PTSD symptoms in COVID-19 survivors and vulnerable populations, and ensuring timely access to counseling and treatment services.