1. Context
MERS is now known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). When a person infected with the virus sneezes or coughs into the air or onto a surface, the virus enters the host's body through the mouth, nose, or eyes. Among the challenges associated with this disease are increased inactivity, obesity, and a rise in inflammatory factors and related diseases (2). Conversely, both the World Health Organization (WHO) and the Ministry of Health have mandated home quarantine measures for affected countries. Accordingly, a fundamental question arises: Are individuals permitted to engage in sports activities during these epidemic conditions to maintain minimal physical fitness? If exercise is deemed safe for some individuals during a coronavirus outbreak, what are the recommended practices (3)? To date, there has been limited scientific research on the coronavirus, particularly concerning the effects of exercise and physical activity on its various dimensions. However, based on the physiological characteristics of the coronavirus and its impact on the immune system, this article aims to address these issues by reviewing previous research on the effects of exercise on the immune system in other viral diseases, along with existing sports recommendations. Moreover, specific sports guidelines for various groups should be established to offer scientific insights for sports professionals, coaches, and the general public during periods of home quarantine and social distancing (2).
2. Evidence Acquisition
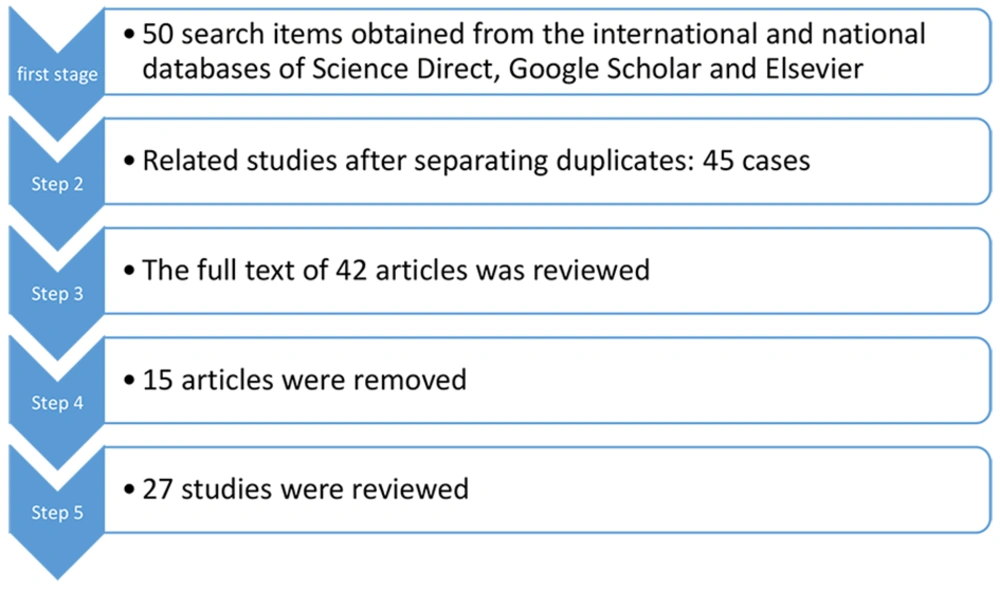
This study belongs to the category of secondary research, employing a methodology focused on reviewing the most pertinent sources available. The examination of sources occurred within the specific timeframe from January 2019 to November 2020. During this investigation, the latest Persian and English articles from reputable domestic and international journals, as well as those indexed in databases such as PubMed, Google Scholar, Science Direct, WHO, etc., were scrutinized (4, 5). Among these articles, those most relevant to the impact of COVID-19 on exercise physiopathology were selected for thorough review and analysis.
The study falls under the classification of secondary research, wherein the latest Persian and English articles from reliable domestic and international scientific databases and journals were surveyed. This process involved databases such as PubMed (American medical science database), ACSM (American college of sports medicine), Science Direct, Google Scholar, and Elsevier publications. The search spanned from 2010 to 2022, resulting in the identification of 42 articles. Subsequently, 15 articles that did not align with the research objectives were excluded, leaving 27 articles for analysis. Criteria for inclusion in the study encompassed topical relevance, novelty, inclusion of non-athletes in the studied population, and the intervention of various types of sports training in the prevention or amelioration of diverse complications. Following a meticulous review process utilizing standardized templates, the abstracts and relevant sections of the selected studies were categorized and subjected to content analysis.
Among the identified articles, those most pertinent to the effects of COVID-19 on sports physiopathology were singled out. Additionally, indicators such as topical relevance, novelty, inclusion of non-athletes in the studied population, and the intervention of various types of sports training in the prevention or amelioration of various complications were employed as criteria for the inclusion of articles in this study. The findings of the selected texts were subsequently subjected to further analysis (Figure 1).
3. Results
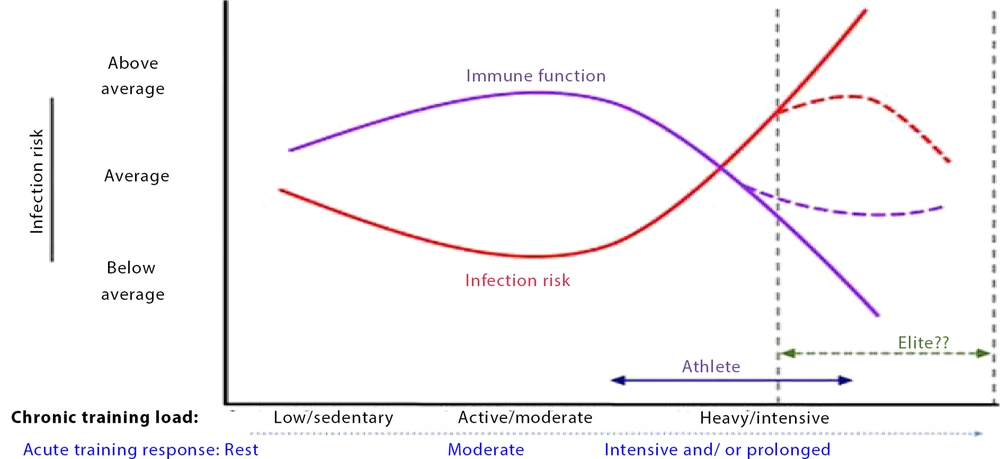
The COVID-19 pandemic and its impact on the immune and respiratory systems have raised many questions about how exercise can protect our bodies against viral infections by boosting immunity. Inactivity increases the risk of type 2 diabetes (6), cardiovascular diseases (7), various cancers (8, 9), depression (10), and increased subcutaneous fat (11). Conversely, the anti-inflammatory effects of sports activities on diseases related to chronic inflammation are well-documented (12). During periods of inactivity, an increase in glucocorticoids such as cortisol weakens the immune system, significantly reducing the ability of T cells to proliferate in response to infectious agents (13). In contrast, each exercise session, especially dynamic cardiorespiratory activities, rapidly mobilizes billions of immune cells, notably those capable of performing crucial functions such as identifying and killing virus-infected cells (13). Among these functions is the release of anti-inflammatory cytokines, which help maintain immunity and enhance the body's resistance to infection (14). Some research findings suggest that exercise offers protection against viruses such as influenza, rhinovirus, and herpesviruses, including Epstein-Barr, varicella-zoster, and herpes simplex virus type 1 (14, 15). However, the type of exercise is important. It has been demonstrated that moderate-intensity exercise during active influenza infection prevents death in mice, maintains better immune cell structure, and alters lung cytokines, ultimately leading to greater survival in rats (16). Moderate-intensity training increases the immune response to vaccines and reduces exhausted T cells (17). Conversely, increasing the proliferation of T cells results in a decrease in inflammatory cytokines such as IL2 (17, 18). One of the most prominent complications of coronavirus disease is an increase in inflammation and inflammatory markers, including C-reactive protein. However, different types of exercise can reduce both inflammation and inflammatory markers (19, 20). Various hypotheses exist about the intensity of exercise and the rate of infection, including hypothesis J. This hypothesis illustrates the relationship between the risk of upper respiratory tract infection and the level of physical activity, as shown in Figure 2.
The J-curve is a concept that describes the relationship between the amount of physical activity and the risk of cardiovascular diseases. It suggests that the risk of cardiovascular diseases is higher in people who engage in very little or excessive physical activity, and lower in those who engage in moderate physical activity.
This concept originates from many researches in the field of physical activity and health. Some studies show that moderate intensity exercise can reduce the risk of cardiovascular diseases and other chronic diseases such as diabetes, respiratory disease, cancer, and increases life expectancy.
Therefore, it can be said that this concept originates from many researches in the field of physical activity and health, and it shows that the risk of cardiovascular diseases is higher in people who have too little or too much physical activity. Therefore, in order to maintain good health, it is recommended to keep your physical activity at a moderate level that contributes to good health.
Research indicates that moderate-intensity physical activity improves immune system function and reduces mortality (21), while high-intensity and stressful exercise can have the opposite effect (22). Epidemiological studies suggest that high-intensity and competitive exercise increases susceptibility to upper respiratory tract infections, whereas gentle physical activity may reduce the symptoms of these infections (23).
The J-curve illustrates that individuals experiencing mild symptoms of upper respiratory tract infections can engage in exercise, whereas those with severe sore throat, body aches, shortness of breath, general fatigue, dry cough, or fever should avoid physical activity. Recovery from viral infections generally requires 2 to 3 weeks of rest. Once symptoms have completely subsided, engaging in light sports activities is considered safe (24, 25).
4. Conclusions
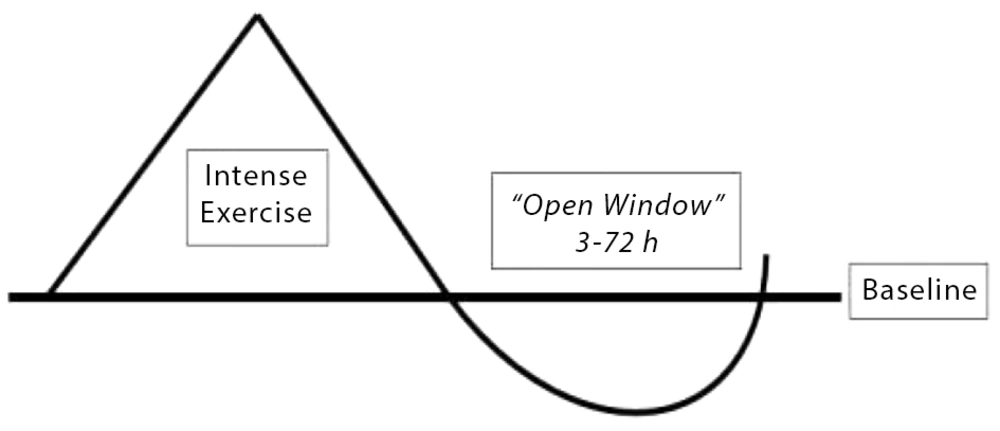
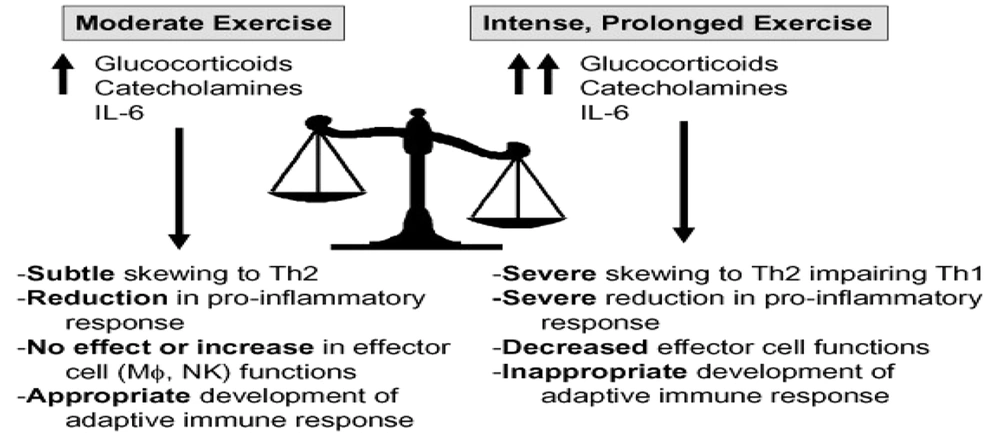
Performing intense and stressful activities suppresses immune parameters, while moderate-intensity exercise reduces inflammation and respiratory viral infections (25). Some studies demonstrate the relationship between regular sports activities and the reduction of influenza and pneumonia incidence (26). It is advisable to limit sports activities during respiratory tract infections because, according to the open window hypothesis, engaging in high-intensity sports activities increases susceptibility to infection in untrained individuals (Figure 3). According to this hypothesis, the immune system's function decreases 3 to 72 hours after intense exercise. Moderate-intensity exercise causes a relative increase in catecholamines, IL6, and glucocorticoids, along with a slight increase in the ratio of Th1 to Th2, ultimately enhancing adaptive immune responses. Conversely, intense and prolonged exercise leads to a further increase in catecholamines, IL6, and glucocorticoids, disrupting adaptive immune responses (Figure 4).
A model for describing the effect of dose-response of exercise activity on Th1 and Th2 (27)
Based on research regarding the intensity of sports activities and TH1 and TH2 immune responses to respiratory virus infections, it can be concluded that healthy and asymptomatic individuals can engage in moderate-intensity exercises following health protocols (27). Although studies on the effects of regular exercise specifically on this disease have not yet been published due to the novelty of COVID-19, previous research on the effects of physical activity on immune system function and similar viral diseases like influenza suggests that regular exercise and an active lifestyle, by increasing energy expenditure and improving physical and mental fitness, promote health and reduce the likelihood of viral infections. In the event of COVID-19 infection, regular exercise can aid in recovery. Considering that both interval and resistance training have significant impacts on cardiorespiratory endurance and muscle strength, respectively, a combination of these activities is recommended to enhance overall health and fitness. Additionally, recognizing that different age and social groups respond differently to COVID-19 and sports activities, prescribing sports activities tailored to specific guidelines for each group is advisable to prevent further harm and risks.