1. Context
In the evolving landscape of telehealth, remote interpretation stands out as a pivotal category, enabling the transmission of medical data across distances for timely analysis. This includes a broad spectrum of medical data, such as radiographs (teleradiology), photographs (teledermatology, teleophthalmology, and telepathology), waveforms like ECGs (telecardiology), and text-based information. These data are transmitted to specialized centers where they are stored and interpreted at a convenient time, optimizing workflow and offering significant advantages over traditional in-person examinations and real-time telehealth interactions (1).
Among the various telehealth modalities, teleradiology and teledermatology have emerged as the most prominent, with teledermatology particularly benefiting from the visual-centric nature of dermatological assessments. Teledermatology facilitates a dynamic exchange between general practitioners and dermatologists, enhancing diagnostic accuracy, continuity of care, and reducing the time to diagnosis, thereby elevating the overall efficacy of healthcare delivery (1).
Telemedicine's applications are diverse, ranging from remote consultations and education to home care, radiography, and even surgery. Teledermatology, in particular, has advanced globally with the advent of sophisticated imaging and communication technologies (2, 3). Since its inception in 1995, teledermatology has become an increasingly utilized tool, providing specialized skin care through remote diagnosis, treatment, and follow-up (4-8).
Dermatologists can now perform clinical evaluations of skin conditions remotely, offering expert care and guidance to other healthcare professionals or directly to patients (9). This approach not only bridges the gap between different levels of care but also ensures that patients, regardless of their location, have access to high-quality dermatological services at an affordable cost (4, 5, 9-11). Teledermatology is delivered through two primary methods: Live video conferencing, which allows real-time interaction between patients and doctors, and the store-and-forward technique, where images of skin lesions are sent over the internet for later examination. With the widespread adoption of smartphones, store-and-forward teledermatology has expanded its reach, making dermatological care more accessible than ever (10, 12, 13).
2. Objectives
This paper delves into the intricacies of teledermatology, comparing its diagnostic accuracy with traditional in-person dermatology, and exploring its potential to revolutionize the field of dermatological care.
3. Methods
3.1. Study Identification
We conducted a comprehensive search for literature on teledermatology systems up to February 10, 2024. The databases searched included the scientific information database (SID), Web of Science, PubMed, and the Association for Computing Machinery (ACM). Our search strategy combined free text and MeSH terms such as "mHealth*", "mobile health", "smartphone app", "remote consultation", "teledermatology", "skin disease", and "diagnosis," using Boolean operators "OR" and "AND" to broaden the search. Details of the search strategy are outlined in Table 1.
| Database | Timespan | Search Fields | Reference Type | Language | Returns | Access Date |
|---|---|---|---|---|---|---|
| PubMed | All years | All fields | All references | English | 302 | 2024/02/10 |
| Web of science | All years | Topic | All references | English | 276 | 2024/02/10 |
| ACM digital library | All years | Anywhere | All references | English | 80 | 2024/02/10 |
| SID | All years | All fields | All references | EN & FA | 58 | 2024/02/10 |
Abbreviations: ACM, association for computing machinery; SID, scientific information database.
3.2. Search Strategy Development and Study Selection
The initial search was conducted by an evaluator (R.P.) and was followed by the use of EndNote X20 (Thomson Reuters, New York, NY, USA) for reference management. Two independent evaluators (R.P. and Z.SH.) screened the titles and abstracts for relevance to teledermatology and skin lesion diagnosis. Any discrepancies were resolved by a third evaluator (A.A.), who also oversaw the project.
3.3. Inclusion Criteria, Exclusion Criteria and Data Extraction
3.3.1. Inclusion Criteria
- Studies focusing on the use of teledermatology systems for diagnosing skin lesions.
- Research relevant to the study objectives, particularly those implementing mobile or online teledermatology systems.
- Studies involving participants with any type of skin lesion.
- Peer-reviewed papers with full texts available in English.
3.3.2. Exclusion Criteria
- Studies not aligned with the research objectives.
- Research limited to specific types of skin diseases or diagnoses.
- Descriptive articles on teledermatology software, reviews, and historical accounts.
- Studies solely utilizing computer-aided diagnostics or artificial intelligence for diagnosis.
- Reviews, editorials, commentaries, and articles without full-text availability.
The full text of the publications was then reviewed by two researchers (R.P. and Z.SH.) to determine their suitability, and their selection was authorized by a third reviewer (A.A.).
3.3.3. Data Extraction
Two researchers (R.P. and Z.SH.) conducted a thorough review of the full texts to assess their relevance. Following this review, a third evaluator (A.A.) provided final approval.
3.4. Quality Assessment
The quality of studies meeting the inclusion criteria was assessed using the Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS), which evaluates potential biases across 14 items related to subject selection, index testing, reference standards, and flow and timing. Each item was rated as "yes," "no," or "uncertain" to determine the risk of bias in the studies (14).
4. Results
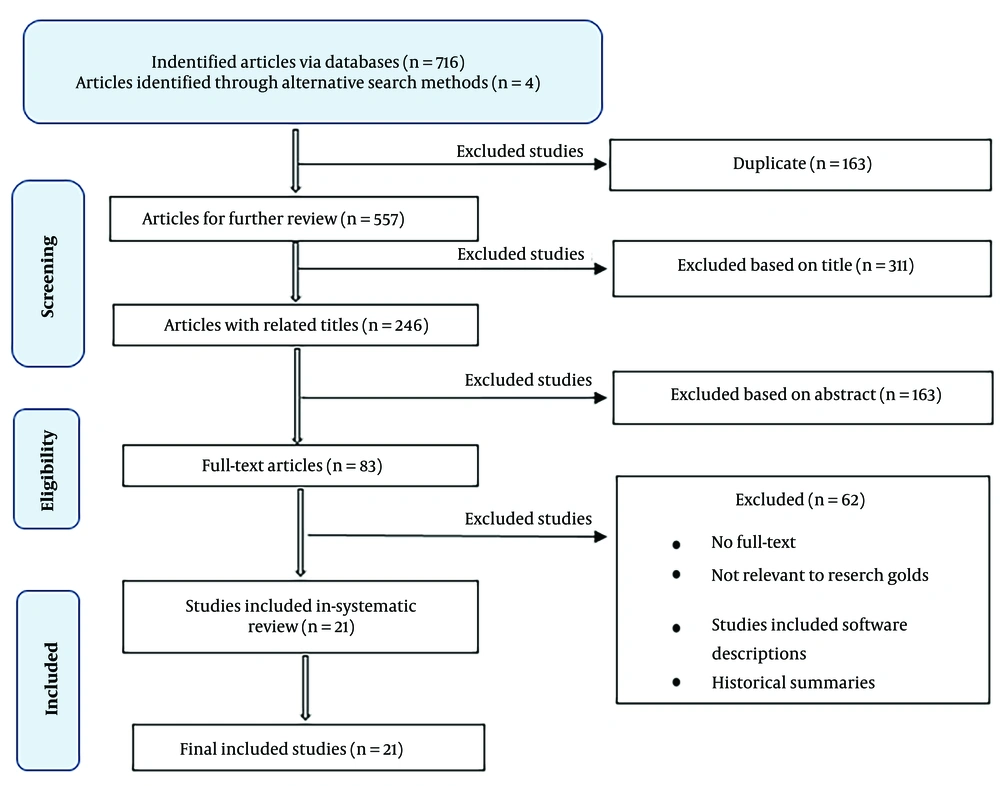
Our initial search yielded 720 records, including four papers from gray literature and 716 from online databases. After removing 163 duplicates, we screened 557 titles and abstracts. Of these, 311 were excluded for not meeting the study criteria. We then assessed 246 full-text articles, resulting in 21 studies being included in our final analysis. A detailed flowchart of the study selection process is presented in Figure 1.
The key characteristics of the included studies, including objectives, sample sizes, methodologies, types of teledermatology systems used, and main findings, are summarized in Table 2.
| References | Study Country | Study Aim | Samples | Type of Teledermatology System | Modality | Diagnostic Concordance | Results |
|---|---|---|---|---|---|---|---|
| Massone et al. (15) | Austria | Creating a platform for using teleconsultation services to diagnose and treat difficult skin cases | 348 health care professionals and 783 requests for consultations | Computer-based | Store- and forward | Not mentioned | By developing a free platform for teleconsultation in dermatology, this study demonstrates that the practice of employing teleconsultation in dermatology has been effective and that a skin problem may be remotely diagnosed by many dermatological professionals on a global scale. |
| Janardhanan et al. (16) | Singapore | Nursing home's use of a web-based teledermatology system. | 50 samples, average age 82 years | Computer-based | Store- and forward | Not mentioned | This article illustrated how the residents' diagnosis and follow-up are frequently handled using teledermatology. Residents were able to get entire dermatological treatment from the convenience of the nursing home thanks to the use of teledermatology, which frequently prevented the need for face-to-face referrals. |
| Chen et al. (1) | United States | Teledermatology system implementation to monitor patient demographics, diagnostic agreement, and treatment trends for patients under the age of 13 | 429 pediatric patients | Computer-based | Store- and-forward | 48% | The practicality and value of teledermatology as a means for primary care providers to quickly acquire the necessary specialized guidance were highlighted in this research of the store and forward teledermatology consultations. Additionally, store and forward teledermatology can enhance therapeutic and diagnostic treatment for children without access to dermatologists who have skin conditions. |
| Rubegni et al. (17) | Italy | To compare the effectiveness of face-to-face consultations versus store-and-forward teledermatology in senior patients | 130 geriatric patients, mean age 80.58 years | Mobile based | Store- and-forward | 87.7% | This study demonstrated "almost perfect agreement" between face-to-face and store-and-forward diagnosis, demonstrating the value of teledermatology as a support tool and potential replacement for traditional in-person examination. |
| Lasierra et al. (12) | Spain | Utilization of the store-and-forward teledermatology system and evaluation of its drawbacks and advantages | 120 teleconsultations, 82 pediatric and 28 adults | Computer-based | Store- and-forward | 55% < | Using the teledermatology system, a good level of diagnosis accuracy was accomplished with reasonable technological constraints, and physicians were happy with the technology. However, the time required for consultations in primary care was a limiting issue. |
| Berndt et al. (18) | Germany | Implementation of a mobile teledermatology service to aid in the treatment and follow-up of patients with skin problems | 13 patients | Mobile based | Store- and-forward | Not mentioned | In this study, dermatologists, nurses, and patients express their satisfaction with the viability and efficacy of teleconsultation utilizing new generation communication technologies to assist treatment and post-treatment monitoring of patients with skin illnesses. |
| Kaliyadan et al. (11) | Saudi Arabia | The purpose of this study was to assess the effectiveness of using a 4G smart phone for mobile teledermatology. Examining the impact of local religious and cultural settings on the adoption of mobile teledermatology was a secondary goal. | 166 patients | Mobile based | Store- and-forward | 95% (kappa = 0.66) | The study revealed that mobile teledermatology had great diagnostic and treatment concordance, as well as high patient satisfaction. |
| Shin et al. (19) | Korean | Smartphone and MMS use, on the diagnostic effectiveness of teledermatology consultations for common skin conditions among army troops | 100 patients | Mobile based | Store- and-forward | 70.7% (kappa = 0.73) | This article demonstrates how using a smartphone for teledermatology consultations includes straightforward procedures, incurs few expenditures, and has a high degree of diagnostic agreement with in-person consultations at dermatological clinics. In actuality, the diagnostic precision of cellphones is better than that of dermatology-unspecialized physicians. |
| Paradela-De-La-Morena et al. (9) | Spain | Examining the efficacy and dependability of store and forward teledermatology (STD) as a pediatrician diagnostic aid and to decrease in-person consultation | 383 patients | Computer-based | Store- and-forward | 57% | In this study, store and forward teledermatology (STD) was shown to be effective in > 50% of instances for screening dermatologic referrals, minimizing delays, and avoiding pointless face-to-face consultations (FFC). |
| Patro et al. (20) | India | Documentation of the degree of agreement between primary care physicians (PCPs) and teledermatologists in the diagnosis of common dermatological disorders | 206 patients | Computer-based | Store- and-forward | 56% | This study found that teledermatology can minimize the requirement for routine clinical consultations while still preserving clinical safety. It can also enhance specialized dermatological services in remote places. |
| Tandjung et al. (21) | Swiss | The practicality and diagnostic accuracy of utilizing digital images of skin lesions in a teledermatological approach | 78 GPs, 981 images | Store- and-forward | 78% | Teledermatology was viable in this study from both a general practitioner and a specialist standpoint, but it raises issues about specialized treatment and calls into question the marketing of teledermatology in clinical practice. | |
| Montazeri et al. (22) | Iran | Planning and execution a teledermatology web-based system to reduce provincial travel | 91 patients | Computer- based | Store- and-forward | Kappa = 0.77 | In this study, the diagnosis was the same in both remote and face-to-face approaches in 85.22% of cases, and it was established that using the software results in a decrease of 82.36% of trips to the province's center. |
| Mahdizadeh and Esmaeili (8) | Iran | Evaluation and comparison accuracy of the diagnoses and treatment plans supplied by the teledermatology approach for the elderly residents of the Kahrizk charity center was to the in-person method. | 37 patients | Computer- based | Store- and-forward | 86% | This study found that teledermatology can increase access to quality skin services for the elderly while reducing referrals and unnecessary transfers to specialized skin hospitals. |
| Faye et al. (23) | Mali, West Africa | Evaluation and feasibility of the impact a teledermatology program on the management of skin disorders | 180 patients | Computer-based | Store- and-forward | 95% | This study shown that implementing a remote dermatology program in primary health care services is possible and can improve skin condition management. |
| Seol et al. (24) | Korea | The use of live interactive teledermatology (LITD) to investigate the prevalence and clinical effects of dermatologic illnesses in Korean prisons | 406 patients | Computer-based | Synchronous | 86.7% | This study found that live interactive teledermatology (LITD) allowed for the detection of new onset dermatologic problems and distinguished them from previously diagnosed conditions. LITD can also contribute to a positive clinical outcome and may thus be an effective alternative to face-to-face consultation in prisoners and other underserved populations. |
| Giavina Bianchi et al. (2) | Brazil | Determine the proportion of pediatric patients' skin lesions that could be managed at primary care level via teledermatology, avoiding in-person visits with dermatologists; and, secondly, assess the frequency, treatment, and referrals of the most common skin lesions in children and adolescents. | 14,925 patients waiting for dermatologist consultation. 6,879 participants. 6,588 visitors | Mobile- based | Store- and-forward | 63% | In this study, teledermatology was used to address a considerable portion of skin lesions without a patient visiting a dermatologist, and patient wait times were also decreased on average. |
| Giavina Bianchi et al. (5) | Brazil | Major objective was to determine how many lesions in people 60 years and older could be treated utilizing teledermatology in combination with primary care doctors. Second, evaluation the distribution and reasons for referrals made by the teledermatologists, as well as the most prevalent skin lesions and therapies given to patients. | 6633 patients | Mobile- based | Store- and-forward | 66.6% | The majority of the patients' dermatoses were treated by teledermatology in this study without the need for an in-person appointment with a dermatologist, keeping them in the primary care setting. The reduction in mean waiting time was unquestionably beneficial for the population who presented with more complex diseases. |
| Rizvi et al. (25) | Norway | Creation of a mobile application that allows users to take clinical images of skin lesions, transmit those images to a professional in skin diseases, and then assess the outcome. | 178 patients | Mobile- based | Store- and-forward | 70% | The results of this study showed that smartphone-based teledermatological technology has a great impact and can lead to decreased patient waiting times, quicker start-up of treatment, reduced travel time, decreased health care costs, and improved access to specialized knowledge. In this pilot study, 70% of patients avoided regular consultation in the specialist health service |
| Fadaizadeh et al. (26) | Iran | Assess the level of agreement and accuracy in the diagnosis of skin disorders in the teledermatology method and clinical | 71 patients | Not mentioned | Store- and-forward | 91.5% (kappa = 0.77) | This study demonstrated that the high degree of correlation between teledermatology findings and results from face-to-face diagnosis demonstrates the method's efficacy in identifying skin illnesses as well as its validation and beneficial effects. |
| Mu et al. (27) | China | Using the Teledermatology to examine patient features and prevalent skin conditions during the COVID 19 epidemic in mainland China | 698 patients | Mobile- based | Synchronous | 74.3% | This paper demonstrated the value of synchronous teledermatology as a tool for dermatologists to communicate. Additionally, the price of the service is reasonable. |
| Tugrul et al. (4) | Turkey | Assessment dermatologists and plastic surgeons' diagnostic accuracy rates and treatment methods for nonmelanocytic skin lesions (NMSLs), as well as the contribution of the teledermoscopy (TDS) method to dermatologists' diagnostic accuracy | 26 patients | Mobile- based | Store- and-forward | 75% | This study shown that Telemedicine (TM) is a simple tool with up to 75% diagnostic accuracy for the detection of Non-Melanocytic Skin Lesions (NMSLs). Dermatologists' ability to diagnose NMSLs with more precision is improved through teledermatology and teledermoscopy. |
4.1. Distribution of Articles by Year
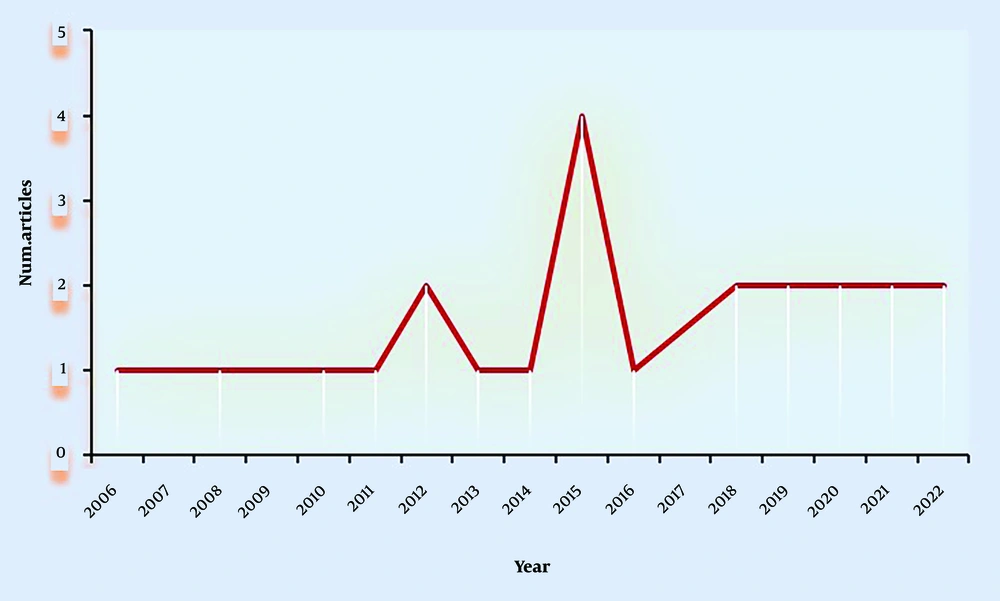
The 21 selected studies span from 2006 to 2022, with the highest concentration in 2015 (19.04%, n = 4) and 2020 (14.28%, n = 3), indicating a growing interest in teledermatology research over the years (Figure 2).
4.2. Capture Information
In all studies, the image of a skin lesion was considered the primary criterion for remote diagnosis, followed by clinical records, age, and gender (Tables 3 and 4).
| Rows | Important Factors | References |
|---|---|---|
| 1 | Photographs of skin lesions, age, location, clinical history, sex | (15) |
| 2 | Digital image of patient's skin condition | (16) |
| 3 | Photographs of skin lesions, age, sex, site of lesion, reason for consultation, and the chronicity of the skin problem | (1) |
| 4 | Digital photographs of the skin manifestations | (17) |
| 5 | Photographs of skin lesions | (12) |
| 6 | Photographs of skin lesions, skin image data and biofeedback information (pain, itching, redness, and weeping) | (18) |
| 7 | Photographs of skin lesions, brief clinical history | (11) |
| 8 | Digital photographs of the skin lesions, age, the duration and symptoms of the lesion, any significant medical history, and/or any concomitant medication | (19) |
| 9 | Images, age, sex, clinical data | (9) |
| 10 | Digital photographs of the skin lesions, age, sex, type of lesion, site of lesion | (20) |
| 11 | Images of the lesion, sex, age, skin phototype, family history and personal history, changes of the skin lesion within the last 4 weeks | (21) |
| 12 | Photo of the lesion, age, sex, history of taking medication, disease history, duration of illness, recurrence of the lesion, family history and symptoms associated with the disease | (22) |
| 13 | Photographs of lesions, age, sex, skin color, disease history, history of taking medication, allergy | (8) |
| 14 | Images, short medical history | (23) |
| 15 | Digital photographs of the skin lesions, short clinical history and patient data | (2) |
| 16 | Digital photographs of the skin lesions (one photo with enough distance to include the entire part of the body in question, a second one in close up, around 15 cm away from the lesion, and a third one in a lateral view to capture the volume of the lesion), short clinical history and patient data | (5) |
| 17 | Photo of the lesion, 1 - 5 predefined questions related to the lesion, brief history | (25) |
| 18 | Image of the lesion (from three angles), patient history | (26) |
| 19 | Photographs of skin lesions, age, sex, medical history | (27) |
| 20 | Clinical and dermoscopic images, age, gender, duration and localization of the lesions, clinical and histopathological diagnoses | (4) |
| Rows | Data Elements | Frequent (%) |
|---|---|---|
| 1 | Photographs of skin lesions | 100 |
| 2 | Clinical history | 61.90 |
| 3 | Age | 52.38 |
| 4 | Sex | 42.85 |
| 5 | History of taking medication | 14.28 |
| 6 | Duration of appearance of skin lesion | 14.28 |
| 7 | Symptoms associated with the disease | 14.28 |
| 8 | Location of the lesion | 14.28 |
| 9 | Family history | 9.52 |
4.3. Study Design
As depicted in Table 2, the majority of the studies focused on the development and evaluation of store-and-forward teledermatology systems. These systems were primarily assessed for diagnostic agreement between primary care physicians and dermatologists. Only two studies utilized live interactive consultations. Regarding the technology used, 52.38% of the studies employed computer-based systems, 38.09% used mobile-based systems, and 9.52% did not specify the type of system used.
4.4. Imaging Requirements
The requirement for image quality varied across the studies. In 38.09% of the cases, diagnoses were made based on skin lesion images without specific prerequisites. In contrast, 61.90% of the studies emphasized predefined imaging requirements, such as resolution, camera specifications, and the use of dermoscopy devices.
4.5. Classification of Diagnoses
A significant portion of the studies (61.90%) reported on common skin conditions such as eczema (19, 20, 23, 25-27), dermatitis (1, 8), acne vulgaris (11), and various inflammatory dermatoses and infections (9, 12, 24), indicating a focus on prevalent dermatological issues in teledermatology research.
5. Discussion
Given the interest of physicians and many institutions in teledermatology, as well as the high percentage of studies related to this subject, the present systematic review of published research comparing the reliability of teledermatology diagnoses with in-person examinations shows a high concordance between remote and in-person diagnoses. The average concordance between remote and in-person diagnoses in these studies was calculated to be 72.8%, which is comparable to the concordance values obtained in the study by Mu and colleagues in 2021 and the study by Tugrul et al. in 2022, which reported diagnostic concordance values of 74% and 75%, respectively (4, 27).
More than half of the studies found the use of teledermatology beneficial, introducing it as a suitable adjunct option that saves time and costs. These studies also reported high levels of patient and physician satisfaction. According to a study conducted by Rizvi and colleagues in 2020, teledermatology can be effective in reducing costs, increasing access to dermatology specialists, and minimizing travel and waiting times for patients (25). However, it is not possible to conclusively determine the overall usefulness and cost-effectiveness of teledermatology systems or their widespread implementation because assessing the level of satisfaction and usefulness in real-world diagnostic and treatment environments requires the long-term implementation of remote systems.
We also analyzed studies to extract data elements used alongside patient lesion photos for remote diagnosis. The goal was to determine how much the use of additional data elements alongside the patient's skin lesion photo affects the accuracy of remote diagnosis. According to the reviews conducted in this study, the average reported diagnostic concordance for studies that only used images of skin lesions for remote diagnosis, compared to those that used additional data elements as supplementary information, did not show a significant difference. Most studies recommended using high-quality images to improve remote diagnosis. Lasierra and colleagues, in their 2012 study, reported that high-quality images of patients' skin lesions significantly increased the accuracy of remote diagnoses (12).
However, the use of teledermatology systems is limited by factors including technological problems, legal limitations, diagnostic limitations, challenges related to patient and physician acceptance, and issues concerning reimbursement. Another significant limitation of remote programs is issues related to the privacy and safety of patient data. Solutions such as the development of remote systems software, the provision of relevant laws, the use of predetermined standards, increased patient and physician participation, and enhanced data security may help address these limitations. Other methods to increase the use of teledermatology systems include fostering collaboration between healthcare providers, patients, technical engineering development companies, and policymakers to set necessary standards.
The main strength of our study is the comprehensive electronic search for evidence related to the topic, using systematic review methods. Additionally, no time range limitation was applied for retrieving studies. However, the lack of a time limitation, while considered a strength, may also be a weakness because older studies that are less advanced in today's technology were also retrieved and included in the analysis process. To address this issue, efforts were made to include the most relevant studies based on the title, abstract, and full text, as well as the use of technology in the analysis.
5.1. Conclusions
In conclusion, the results of the included studies indicate that teledermatology can be a reliable adjunct option that increases access to services, saves costs and time, and enables patients to take timely action for the treatment of skin conditions. Therefore, utilizing findings from previous studies to overcome obstacles and limitations will be beneficial for the effective implementation of teledermatology programs.