1. Background
Smoking is a widespread habit with well-documented adverse effects on general health, and its impact becomes even more significant when considering specific medical conditions such as androgenic alopecia (1). Androgenic alopecia, or male pattern baldness, is a common form of hair loss affecting a large portion of the population. It is characterized by a receding hairline and thinning on the crown and temples, often leading to partial or complete baldness. The condition is primarily caused by genetic factors and the sensitivity of hair follicles to dihydrotestosterone (DHT), a byproduct of testosterone metabolism (2). Although not life-threatening, androgenic alopecia can have profound psychological and social effects, often reducing self-esteem and quality of life (3).
Hair transplantation has become a popular and effective treatment option for androgenic alopecia, involving the transfer of healthy hair follicles from densely haired areas of the scalp to regions affected by hair loss. This technique has been shown to produce natural-looking results and can significantly improve the appearance of hair (4). However, the success of hair transplantation is influenced by several factors, including the patient’s general health, age, and lifestyle habits, such as smoking.
Smoking is linked to various health issues, including cardiovascular disease, lung cancer, and respiratory problems. In the context of hair transplantation, smoking may have specific implications for patients with androgenic alopecia. Studies indicate that smoking can impair wound healing, increase the risk of complications, and negatively affect the survival of transplanted hair follicles (5). Additionally, smoking is associated with increased inflammation and oxidative stress, which may contribute to the progression of androgenic alopecia (6). Previous studies have shown that nicotine can overstimulate cellular nicotinic acetylcholine receptors, leading to their desensitization and destruction of hair follicles through the activation of programmed cell death pathways in keratinocytes (7).
This study examines the relationship between smoking, alcohol consumption, hookah usage, and outcomes in patients with androgenic alopecia who underwent hair transplantation at the Jordan Clinic in Tehran, Iran, between 2011 and 2013. By exploring the effects of these lifestyle factors on this specific patient population, we aim to highlight potential complications, outcomes, and considerations relevant to treating hair loss in individuals who consume these substances. Understanding these effects is crucial for optimizing treatment strategies and improving the management of androgenic alopecia in clinical practice (8). By identifying the potential risks and complications associated with smoking, healthcare professionals can develop targeted interventions to optimize treatment outcomes. These may include encouraging smoking cessation, implementing specific surgical techniques, and providing tailored post-operative care.
2. Objectives
Additionally, the results of this study contribute to the growing body of knowledge on the impact of lifestyle factors on hair transplant outcomes, informing future research and clinical practice in hair restoration.
3. Methods
This study employed a robust and rigorous methodology to investigate the effects of smoking on patients with androgenic alopecia who underwent hair transplantation at the Jordan Clinic between 2011 and 2013.
3.1. Study Design and Setting
This was a retrospective observational study conducted at the Jordan Clinic, a leading hair restoration center in Jordan. The study population consisted of patients with androgenic alopecia who underwent hair transplantation at the clinic between 2011 and 2013. Sampling was conducted using a convenience sampling method, with the study population comprising 97 non-smokers and 23 smokers. All patients were classified as stage III according to the Ludwig classification system.
3.2. Data Collection and Analysis
Patient data were systematically extracted from the clinic’s electronic medical records. A comprehensive data collection checklist was developed to capture relevant demographic, clinical, and treatment-related variables, including patient age, gender, smoking status, severity of androgenic alopecia, details of the hair transplant procedure, and postoperative outcomes. A total of 23 patients (19.2%) reported smoking, 28 patients (23.3%) smoked hookah, and 36 patients (30%) consumed alcohol. Inclusion criteria consisted of a diagnosis of androgenic alopecia and the feasibility of patient follow-up, while exclusion criteria included conditions such as AIDS, hepatitis, coagulation disorders, and psychological illness.
The collected data were entered into SPSS version 13 for analysis and subsequently evaluated using repeated-measures ANOVA statistical methods. Descriptive statistics were employed to summarize the demographic and clinical characteristics of the study population. Inferential analyses, such as regression modeling, assessed the association between smoking status and various hair transplant outcomes, including graft survival, patient satisfaction, and complication rates. All analyses were conducted using a reputable statistical software package, with the significance level set at a p-value of less than 0.05.
3.3. Ethical Considerations
This study was approved by the Institutional Review Board of the Jordan Clinic, and all data collection and analysis procedures were conducted in accordance with the tenets of the Declaration of Helsinki. Patient confidentiality was strictly maintained, and informed consent was obtained from all participants before their inclusion in the study. Using this rigorous and comprehensive methodology, the researchers aimed to provide robust and reliable evidence on the impact of smoking on hair transplant outcomes in patients with androgenic alopecia. The findings of this study will have significant implications for healthcare professionals involved in the management of this condition, as well as for patients seeking hair restoration treatment.
4. Results
The study population consisted of 94.2% male patients and 5.8% female patients. Eight of the smokers exhibited spontaneous bleeding at the implant site following surgery. After crusting, these areas were observed to be hairless, a finding not present in non-smoking patients. Notably, non-smokers experienced a higher incidence of head injuries, and the prevalence of baldness in these patients appeared to be higher than in smokers. Among smokers, 11 individuals showed significantly lower hair density and slower hair growth in the middle postfrontal area compared to non-smokers. Overall, hair growth in the central area was reduced in smokers compared to non-smokers.
The mean hair count in smokers at the second week and the end of the twelfth month was 12.6 and 8.1, respectively. In non-smokers, these values were 14.6 and 12.2, respectively. Additionally, among alcohol users, the mean hair count was observed to be 10.9 and 8.6 at two weeks and twelve months, respectively, compared to non-drinkers, who exhibited 14.5 and 11.1 hairs at the same intervals, demonstrating a statistically significant difference (P > 0.05).
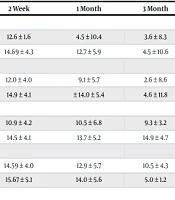
There was no statistically significant difference in hair growth between male and female patients throughout the study (P > 0.05). However, hair count was significantly lower in smokers than in non-smokers at all time points (P < 0.05). The number of cigarettes consumed had no effect on hair count at any time point (P > 0.05). Patients who smoked hookah had significantly lower hair counts at all times compared to non-hookah smokers (P < 0.05). Furthermore, patients who smoked both cigarettes and hookah simultaneously also showed significantly lower hair counts compared to non-smokers (P < 0.05). Similarly, alcohol users had significantly lower hair counts than non-drinkers at all times during the study (P < 0.05). These results are presented in Table 1.
| Variables | 2 Weeks | 1 Month | 3 Months | 6 Months | 12 Months | P-Value |
|---|---|---|---|---|---|---|
| Smoking | > 0.05 | |||||
| Yes (N = 23) | 12.6 ± 1.6 | 4.5 ± 10.4 | 3.6 ± 8.3 | 9.3 ± 5.9 | 8.1 ± 3.7 | |
| No (N = 97) | 14.69 ± 4.3 | 12.7 ± 5.9 | 4.5 ± 10.6 | 10.0 ± 5.6 | 12.2 ± 5.4 | |
| Hubble-bubble | > 0.05 | |||||
| Yes (N = 28) | 12.0 ± 4.0 | 9.1 ± 5.7 | 2.6 ± 8.6 | 7.0 ± 3.3 | 8.5 ± 0.7 | |
| No (N = 92) | 14.9 ± 4.1 | ± 14.0 ± 5.4 | 4.6 ± 11.8 | 11.8 ± 5.8 | 11.3 ± 5.8 | |
| Alcohol | > 0.05 | |||||
| Yes (N = 36) | 10.9 ± 4.2 | 10.5 ± 6.8 | 9.3 ± 3.2 | 8.3 ± 5.5 | 8.6 ± 0.7 | |
| No (N = 84) | 14.5 ± 4.1 | 13.7 ± 5.2 | 14.9 ± 4.7 | 11.7 ± 5.8 | 11.1 ± 5.5 | |
| Gender | > 0.05 | |||||
| Male (N = 113) | 14.59 ± 4.0 | 12.9 ± 5.7 | 10.5 ± 4.3 | 9.9 ± 5.2 | 11.5 ± 5.7 | |
| Female (N = 7) | 15.67 ± 5.1 | 14.0 ± 5.6 | 5.0 ± 1.2 | 15.0 ± 9.8 | 9.5 ± 0.7 |
a Values are expressed as mean ± SD.
5. Discussion
There is a growing body of evidence linking smoking to various health problems, including cardiovascular diseases and respiratory disorders. The negative impact of smoking on hair health is well-documented (7, 9). The mechanisms by which smoking causes hair loss are multifactorial, involving vasoconstrictor effects, DNA damage, oxidative stress, and inflammation (5). Smoking can reduce blood flow to hair follicles, disrupt the endocrine system, and lead to hair loss and premature graying (9).
The study found that smoking significantly negatively impacted hair transplant outcomes in patients with androgenic alopecia. Specifically, smokers experienced higher rates of complications, such as spontaneous bleeding at the implant site, and lower rates of hair growth compared to non-smokers. This corroborates previous studies that identify smoking as a contributing factor to hair loss (6). Additionally, the study found that hookah smoking and alcohol consumption were associated with poorer hair transplant outcomes. This aligns with existing research showing that smoking is a risk factor for various health issues (5, 6). These findings are consistent with previous studies demonstrating that smoking contributes to reduced hair follicle growth following transplantation. The results of our study also support prior research indicating smoking as a contributing factor in the development of androgenetic alopecia (10), possibly due to the impact of cigarette smoke on the molecular pathways regulating hair follicle function (11).
However, this study provides new insights into the specific effects of hookah smoking and alcohol consumption on hair transplant outcomes. It is acknowledged that the study is limited by its retrospective design and the potential for bias in data collection. Future studies should address these limitations and provide more comprehensive insights into smoking's effects on hair transplant outcomes. Additionally, studies comparing the effects of different types of smoking, such as cigarettes and hookah, on hair transplant outcomes would be valuable. The findings have significant implications for healthcare professionals managing androgenic alopecia and patients seeking hair restoration treatment (7). These results indicate that smoking cessation should be strongly encouraged for patients undergoing hair transplantation to enhance treatment outcomes and reduce the risk of complications.
5.1. Conclusions
Existing literature consistently emphasizes the detrimental effects of smoking on hair health, including negative impacts on hair transplant outcomes, increased hair loss, and premature graying. The evidence highlights that smoking cessation both before and after hair transplantation is essential for achieving optimal results and supporting a healthy recovery process.