1. Background
Diabetes is a major metabolic disorder primarily characterized by elevated blood glucose concentrations. The number of people affected by diabetes is continuously increasing worldwide, and risk factors such as improper nutrition and physical inactivity play significant roles in its incidence, prevalence, and associated complications. Global studies investigating the prevalence of diabetes estimate that by 2030, the prevalence will reach 4.4% across all age groups, and the total number of individuals with diabetes will rise to 366 million. This projected increase assumes that obesity levels will remain constant. Among different age groups, the greatest rise in prevalence is expected among individuals over 65 years old. Notably, the largest overall increase will occur in developing countries, where the prevalence of diabetes is predicted to grow by up to 170%. Studies conducted in Iran also do not indicate a more favorable situation. The prevalence of diabetes among older adults in Iran has been reported to be as high as 14.4%, and, similar to trends observed in other developing countries, the prevalence of diabetes in Iran is expected to continue rising (1-4).
In many countries, diabetes is the leading cause of blindness and the most common cause of limb amputation and chronic kidney failure among individuals aged 20 to 70 years. Diabetes is also one of the five major factors contributing to the cardiovascular disease epidemic in Asia (5). Over the long term, diabetes causes microvascular complications such as retinopathy and neuropathy, as well as macrovascular complications such as myocardial infarction, angina pectoris, and stroke. In addition, diabetes-related complications — such as fear of hypoglycemia, lifestyle changes, and concerns about long-term consequences — may lead to a decrease in Health-Related Quality Of Life (HRQOL) (6). The prevalence of depression is also higher among individuals with diabetes compared to those without diabetes (7). Recent studies have shown that the risk of depression in people with diabetes is twice that of non-diabetic individuals (7-9). One study demonstrated a distinction between major depressive disorder (MDD) and diabetes-related depression (DD) (10), noting that even in the absence of MDD, DD is significantly associated with self-care behaviors and blood glucose control (7, 8, 10, 11). Depression in diabetic patients has been linked to factors such as poor glycemic control, non-compliance with treatment, and an increased risk of vascular complications including retinopathy, neuropathy, diabetic nephropathy, and macrovascular diseases (12-14). Some studies have also identified depression as a risk factor for mortality among diabetic patients (15). According to the aforementioned points, proper care and the application of preventive measures — such as effective blood sugar control and the management of associated conditions like hypertension and hyperlipidemia, along with proper nutrition and regular exercise — can prevent or delay the onset of dangerous complications in diabetic patients. Moreover, implementing strategies to prevent diabetes-related complications can significantly reduce healthcare costs and mortality rates (16).
When diabetic patients do not receive adequate treatment and care, they are at a higher risk of developing multiple chronic complications, which can lead to irreversible disabilities and even death. Numerous studies in the United States have shown that the current standard of care for diabetic patients falls short of the American Diabetes Association (ADA) guidelines (17). Independent of the coronavirus pandemic, the pattern of common diseases in Iran is shifting from communicable to non-communicable diseases. The high prevalence of diabetes represents one of the most significant non-communicable diseases in Iran. Among the indicators of this trend, the increasing importance of diabetic patient care stands out, highlighting its critical impact on the quality of life (QOL) across all dimensions for diabetic patients. It is well recognized that many factors influence the quality of diabetes care, including access to healthcare services, patient adherence to treatment protocols, annual medical testing, and lifestyle behaviors. Because no prior study had been conducted in Behbahan city regarding the quality of care for diabetic patients, there was no available information on the quality of care provided to this population. Considering that the care of diabetic patients is influenced by various factors — including access to different levels of specialized healthcare services and the level of patient awareness about self-care practices — and given that the quality of the primary healthcare system in delivering appropriate services can vary significantly from one region to another, it was essential to conduct an evaluation in this specific setting.
Until now, no study had been carried out within the population covered by Behbahan Faculty of Medical Sciences to assess the quality of diabetic patient care based on standard criteria, and no information was available regarding the effectiveness of the primary healthcare system in this regard.
2. Objectives
This study was conducted to evaluate the quality of care provided to diabetic patients and to investigate how the quality of care is influenced by factors such as QOL, psychological distress, physical activity, family history of diabetes, marital status, and other variables. The ultimate aim is to provide valuable information to the healthcare system and support the implementation of necessary interventions to enhance the quality of diabetic patient care.
3. Methods
This cross-sectional, descriptive-analytical, and correlational study, initially scheduled to be conducted in the winter of 2018, was postponed due to the onset of the coronavirus pandemic, the excessive involvement of health workers in patient follow-up and contact tracing, and the resulting impossibility of collecting data. The study was eventually carried out from January to March 2021 in Behbahan city. The research population included all patients with type 2 diabetes who were covered by the health homes affiliated with Behbahan School of Medical Sciences. The required sample size for the study was determined based on previous studies (17-19) and included 310 patients. Using a multi-stage sampling method, first, several health homes were selected from each rural health center, and then, through random sampling, 310 patients with type 2 diabetes were selected. After obtaining verbal consent, the relevant questionnaires were administered to them. The inclusion criteria were: Patients with type 2 diabetes aged between 20 and 70 years, having an active care record in the health homes, and residing in rural areas. Exclusion criteria included: Having other types of diabetes (e.g., type 1 diabetes, gestational diabetes) and unwillingness to participate in the study. Sampling was performed using a simple random method.
Based on previous studies and the study conditions, 310 patients who were willing to participate were selected. Research data were collected by trained nurses at the health centers using the interview method. To collect information, a demographic questionnaire was used, which included items on age, sex, weight, height, marital status, occupation, income status, insurance coverage, education level, and duration of illness. In addition, care information (results recorded in the patient’s care file and the results of the most recent tests performed over the past year) was gathered. In this study, the quality of patient care was assessed using a scoring system based on several important care indicators from the past year. The evaluated variables included measurement of HbA1c, fasting blood sugar, systolic and diastolic blood pressure, blood lipids, and microalbuminuria (MA) at least once during the previous year, as well as whether the patient was undergoing treatment with oral medications or insulin (2021). In this scoring method, a minimum of 0 and a maximum of 10 points were assigned to each care quality indicator. Considering the four care quality indicators, the overall score could range from 0 to 40, with higher scores indicating better quality of care.
3.1. Quality of Life Questionnaire
The World Health Organization quality of Life (WHOQOL-BREF) is a 26-item instrument consisting of four domains: Physical health (7 items), psychological health (6 items), social relationships (3 items), and environmental health (8 items); it also includes two items assessing overall QOL and general health. Each item of the WHOQOL-BREF is scored on a five-point ordinal scale, ranging from 1 to 5. The raw scores are then linearly transformed to a 0 – 100 scale.
The physical health domain includes items related to mobility, daily activities, functional capacity, energy, pain, and sleep. The psychological domain measures aspects such as self-image, negative thoughts, positive attitudes, self-esteem, mentality, learning ability, memory and concentration, religious beliefs, and overall mental status. The social relationships domain contains questions regarding personal relationships, social support, and sexual life. The environmental health domain covers financial resources, safety, access to health and social services, the physical living environment, opportunities for acquiring new skills and knowledge, recreation, the general environment (including noise and air pollution), and transportation (20). The validity and reliability of the Persian version of this questionnaire were confirmed by Nejat et al. in 2014 (21).
3.2. Distress Questionnaire
This brief tool was developed for the purpose of screening for mental disorders. The questionnaire consists of ten questions, each with five possible response options. The total score is calculated by summing the scores of all items, resulting in a range from 10 to 50. The validity and reliability of the Persian version of this questionnaire were confirmed in the study conducted by Ataei et al. (22).
3.3. Statistical Analysis
Data analysis was performed using SPSS version 24 for descriptive statistics and smart partial least squares (SmartPLS) version 3 (23) for structural equation modeling (SEM) analysis. Partial least squares (PLS) is a variance-based method, in contrast to traditional covariance-based methods. The significance level for all hypotheses was set at P-value < 0.05.
4. Results
This study was conducted on 310 patients. The mean age of the participants was 58.01 ± 11.75 years. Approximately 27.4% of the participants were male and 72.6% were female. Additionally, 93.5% of the participants were married. The mean duration of diabetes among participants was 8.65 ± 4.22 years. Regarding psychological distress, 36.1% of participants had low levels, 23.9% had moderate levels, 31.6% had high levels, and 8.4% had very high levels of distress. The mean and standard deviation of HbA1c levels — one of the most important indicators of diabetes care—were 9.71 ± 2.13. Table 1 presents the mean and standard deviation of other laboratory parameters relevant to the care of patients with type 2 diabetes.
| Variables | Mean ± SD |
|---|---|
| Fasting blood sugar level | 196.23 ± 81.18 |
| Systolic blood pressure value | 131.12 ± 23.01 |
| Diastolic blood pressure | 81.42 ± 9.89 |
| Amount of cholesterol | 191.41 ± 44.12 |
| LDL amount | 108.11 ± 36.23 |
| HDL amount | 43.32 ± 11.89 |
| Amount of triglycerides | 197.23 ± 97.11 |
| HBA1C amount | 9.71 ± 2.13 |
The Mean and Standard Deviation of Laboratory Criteria for Care of Patients with Type 2 Diabetes
Table 2 presents the mean and standard deviation of the HRQOL dimensions. The mean and standard deviation of the total QOL score for the study sample were 46.33 ± 13.33.
| Variables | Mean ± SD |
|---|---|
| Physical health | 50.71 ± 15.37 |
| Mental health | 52.38 ± 11.59 |
| Community relation | 56.13 ± 11.36 |
| Social environment | 56.80 ± 10.58 |
| Total QOL number | 46.33 ± 13.23 |
Mean and Standard Deviation of Quality of Life Dimensions Related to the Health of Patients with Type 2 Diabetes
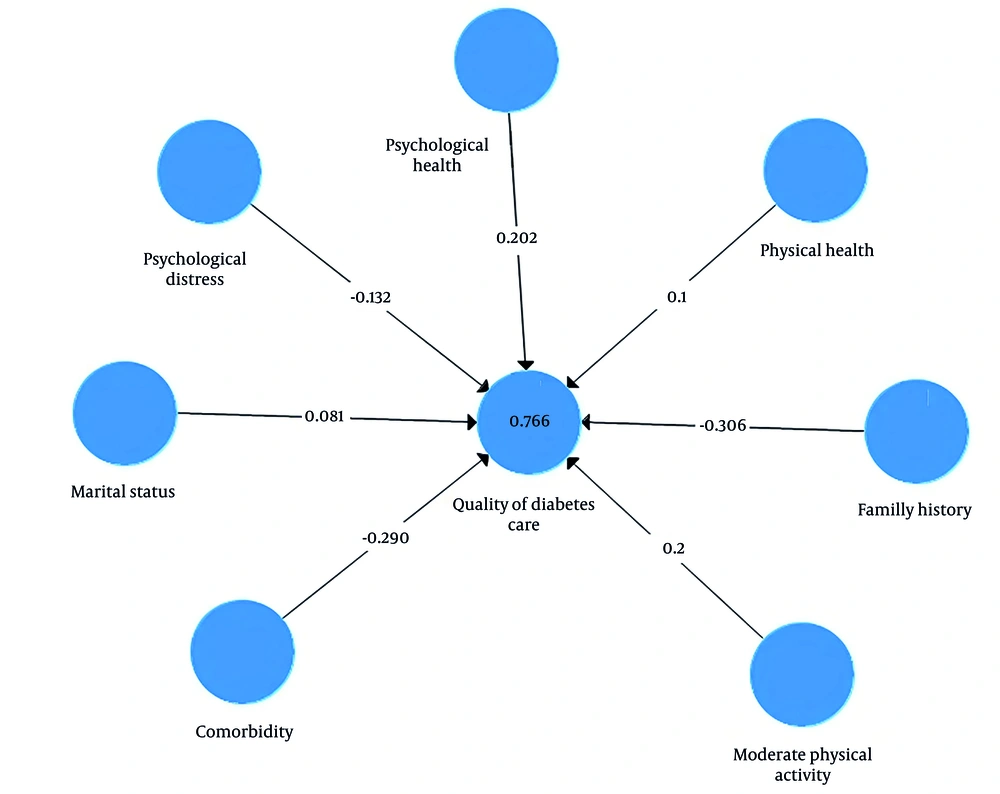
After testing the model, only the variables that had a significant relationship with the quality of diabetes care remained in the final model. Figure 1 shows the final model after these adjustments. The coefficient values for comorbidity, moderate physical activity, mental health, and family history on the quality of care were 0.29, 0.20, 0.20, and 0.30, respectively, indicating the strong impact of these variables on the quality of diabetes care. Mental distress, physical health, and marital status also showed significant relationships with the quality of care, although their effect sizes were comparatively smaller.
The validity and reliability of the structural model in PLS were assessed using Cronbach’s alpha, average variance extracted (AVE), composite reliability, and rho-A. The values for all constructs indicated appropriate validity and reliability of the model.
Table 3 presents the fit indices of the PLS model. The SRMR value was less than 0.08 and the NFI value was greater than 0.90, confirming a good model fit. Additionally, the R2 value was 0.76, further supporting the appropriate fit of the model. Other fit indices reported in the table also fall within acceptable ranges.
| Fit Index | Estimation Model | Saturation Model |
|---|---|---|
| SRMR | 0.05 | 0.05 |
| d ULS | 0.34 | 0.34 |
| d-G1 | 0.15 | 0.16 |
| d-G2 | 0.13 | 0.12 |
| Chi-square | 623.24 | 624.36 |
| NFI | 0.91 | 0.90 |
Model Fitting Indices of Quality Care of Type 2 Diabetic Patients and Some Related Factors
Table 4 shows the coefficients of the paths. According to the results presented in Table 4, all the relevant pathways are statistically significant at the level of P < 0.001. The highest path coefficients are associated with family history and comorbidity.
| Path | Original Sample (O) | Sample Mean | SD | t-Test | P-Value |
|---|---|---|---|---|---|
| Mental health → quality of diabetes care | 0.20 | 0.20 | 0.078 | 21.331 | 0.000 |
| Physical health → quality of diabetes care | 0.10 | 0.10 | 0.049 | 11.501 | 0.000 |
| Moderate physical activity → quality of diabetes care | 0.20 | 0.20 | 0.096 | 21.441 | 0.000 |
| Family history → quality of diabetes care | -0.306 | -0.306 | 0.084 | 34.652 | 0.000 |
| Psychological distress → quality of diabetes care | -0.132 | -0.132 | 0.066 | 14.126 | 0.000 |
| Marital status → quality of diabetes care | 0.0813 | 0.0813 | 0.019 | 7.724 | 0.000 |
. Path Coefficients and Significance of the Structural Model of Factors Related to the Quality of Care of Type 2 Diabetic Patients
5. Discussion
The quality of diabetes care is influenced by various factors, and it is not possible to include all of them in a single study. However, in the present study, by reviewing previous research conducted in this field, an effort was made to extract and examine the most effective and important variables. Ultimately, a structural model based on relevant theoretical concepts was developed and tested. The results of the present study showed that, overall, the quality of care for diabetic patients was not optimal according to existing standards, with less than 30% of the studied patients receiving good quality care. These findings are consistent with national and regional studies conducted in Iran (19, 24). In the present study, patients who, in addition to diabetes, suffered from other diseases such as hypertension and hyperlipidemia were found to have poorer quality of care. It appears that comorbidity creates additional challenges in maintaining blood sugar levels within the normal range. In the study by Hussain and Chowdhury, controlling blood sugar in the presence of comorbidities and managing drug therapies was identified as one of the serious challenges in the care of diabetic patients (25). Similarly, a family history of diabetes — which seems to be influenced by both lifestyle and genetic factors — was also associated with difficulties in maintaining normal blood glucose levels. In the study by Xiong et al., it was reported that failure to control blood sugar within the optimal range was significantly associated with the development of late-stage complications of diabetes, including diabetic foot. Notably, the number of diabetics within a family was significantly correlated with the risk of developing such complications (26).
In the study by Broome et al. (27), family history was identified as one of the factors influencing diabetes control. Since most diabetic patients are diagnosed at an advanced age and often have additional medical problems at the time of diagnosis, many are unable to engage in intense physical activities. Therefore, it is recommended that moderate physical activities such as walking, swimming, and cycling be encouraged, as they yield more favorable outcomes. In the study by Sigal et al., moderate physical activity was evaluated as beneficial for elderly patients and diabetic patients with specific medical conditions.
In the present study, a significant relationship was observed between moderate physical activity and the quality of diabetes care (28). Additionally, a significant relationship was found between marital status and the quality of care, which may be attributed to the better QOL often reported among married individuals. Improved QOL, in turn, contributes to better quality of care. This finding is consistent with the study by Han et al., which also observed a significant relationship between marital status and QOL (29). Furthermore, based on the results of the present study, individuals with higher psychological distress scores were found to have a poorer quality of care, highlighting the importance of the psychological dimension in diabetes management. Similar findings were reported in the study by Ataei et al., where patients with higher psychological distress scores on the K10 Questionnaire had lower quality of care (18). In the present study, a significant relationship was also observed between certain dimensions of QOL and the quality of care for diabetic patients. This aligns with findings from other research. For example, in the study by Pera (30), individuals who achieved higher scores on the HRQOL Questionnaire — indicating better HRQOL — also demonstrated better quality of diabetes care. Although there is limited historical data specifically on the quality of care for diabetic patients in this population, it appears that the spread of the coronavirus pandemic contributed to a decline in care quality. Key reasons for this include the redeployment of health personnel to pandemic-related duties and reduced patient attendance for routine care. This decline in care quality has also been documented at the global level (31, 32).
5.1. Conclusions
The present study highlights the unfavorable quality of care for patients with diabetes, a situation that requires special attention due to the chronic complications associated with the disease. Strengthening care programs for diabetic patients — particularly within the framework of the IraPEN program, which includes psychosocial interventions — can help improve the quality of care for individuals with type 2 diabetes.
5.2. Limitations
The impossibility of examining all the patients with low literacy levels or the illiteracy of some patients, which made the interview process difficult, and the impossibility of examining some variables were among the limitations of this study.