1. Background
Chronic kidney disease (CKD) is a progressive, irreversible condition in which the body's ability to maintain fluid and electrolyte balance is compromised, leading to uremia and azotemia (1). According to data from the centers for disease control (CDC), approximately 52% of advanced CKD patients undergo hemodialysis (2). In Iran, the prevalence of diagnosed CKD patients is about 253 per million population (3). Hemodialysis patients suffer from various issues, including sleep disturbances, with prevalence rates ranging between 20% and 80% (4). Insomnia significantly impacts individuals' quality of life, leading to substantial declines in daily functioning across emotional, social, and physical domains (5). Using pharmaceutical drugs to improve sleep quality may pose additional risks for patients. Therefore, adopting alternative strategies is essential (6). Studies emphasize the effectiveness of massage and therapeutic touch in promoting relaxation and reducing emotional distress (7, 8). One such technique is slow stroke back massage (SSBM) (3). The SSBM promotes lymphatic drainage, increases blood circulation, stimulates veins, improves muscle metabolism, and reduces sympathetic activity, inducing patient relaxation (9).
A study by Lubbna et al. demonstrated that SSBM positively affects sleep quality and anxiety levels in elderly stroke patients (10). In contrast, Unal and Balci Akpinar concluded that the effectiveness of SSBM in patients remains controversial, requiring further studies (11). The time of back massage in various studies is mostly mentioned as occurring during the night and before the patient sleeps. It is thought that there is a need for studies that evaluate the effect of massage earlier (12). On the other hand, some studies determined that there was no statistically significant relationship between back massage and sleep (11). Also, in the study by Harris and Richards, in which light pressure was applied and the session duration was the shortest at 3 minutes, it was found that back massage did not improve sleep quality (13). There is no common view on the duration of back massage, but it seems that the longer the duration of massage, the more effective it is.
These uncertainties within medical communities highlight the need for robust research backing to integrate these complementary therapies into nursing practices. Therefore, this study evaluates the effect of back massage on sleep quality.
2. Objectives
The SSBM is a simple, cost-effective, non-invasive, and safe technique without side effects (11). Therefore, this study aims to determine the impact of SSBM on sleep quality in hemodialysis patients, as well as sleep quality over time after the intervention.
3. Methods
3.1. Study Design and Setting
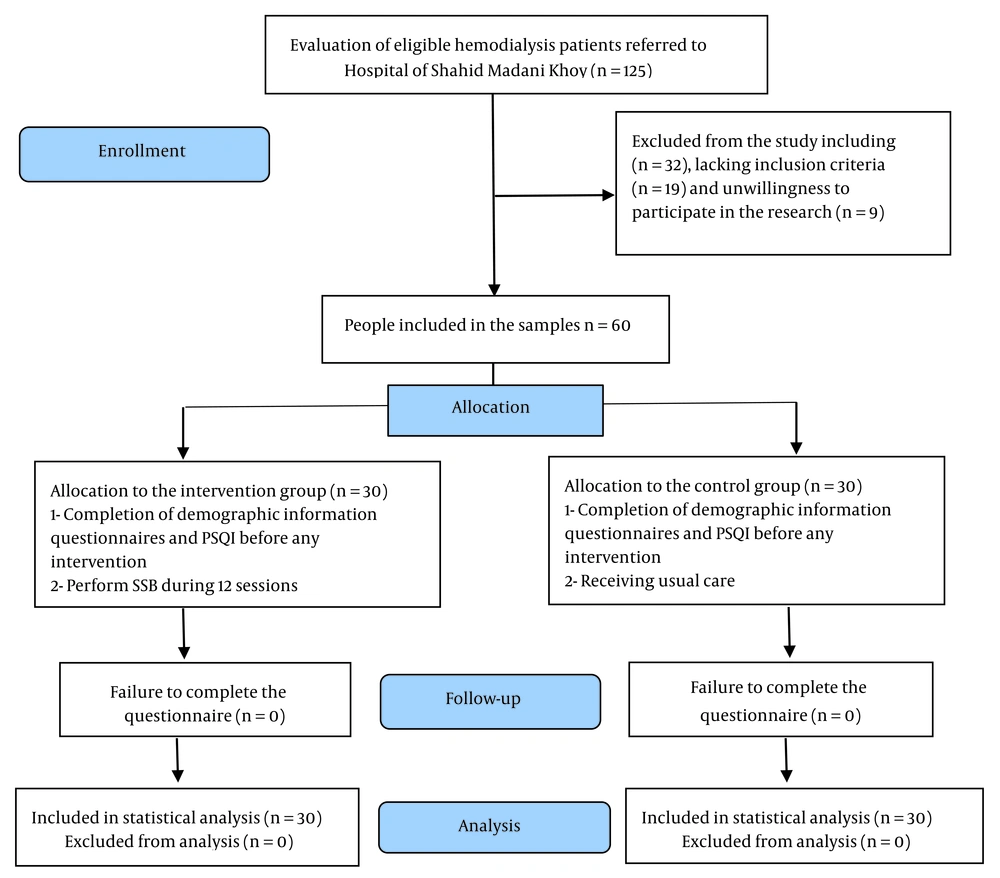
This study was a randomized controlled clinical trial (IRCT20231122060139N1) conducted at Shahid Madani Hospital in Khoy, Iran. The sample size, considering (β = 85%), (α = 0.05), (SD of the sleep quality = 4.24), the mean difference of sleep quality (d = 2.4) (14), and with a consideration of 10% attrition (3), was calculated to be 60.
Patients were selected through convenience sampling and then assigned to two groups using simple random sampling. Using a simple randomization method, each of the selected patients was randomly assigned a number, and their name was written on envelopes given to someone unaware of the study objectives. All the sealed envelopes were placed in a container, and based on chance, the first 30 numbers taken out were assigned to the intervention group, and the second 30 numbers were assigned to the control group. In this way, neither the researcher nor the participant knew who was in which group.
Inclusion criteria were a Pittsburgh Sleep Quality Index (PSQI) score of 5 or higher, at least 3 months of dialysis history, and healthy skin in the massage area. Exclusion criteria were the use of complementary therapies in the past three months, use of sleeping pills, severe neuropathy, hospitalization, and inability to attend massage sessions.
3.2. Intervention
After obtaining ethical approval and patient consent, an initial session was held to explain the study's objectives to participants. In the intervention group, a research assistant provided the SSBM thrice weekly for 10 minutes per session. Sleep quality was assessed in both groups using the PSQI before the intervention and again at two and four weeks post-intervention (Figure 1). Massages were conducted between 3 and 7 PM in a designated dialysis unit room free of other patients (15). Meanwhile, the control group received standard care and remained unaware of the intervention group's massage therapy.
To learn massage, the researcher was first taught SSBM by a physiotherapist, and after several practice sessions and repetitions, the researcher, under the supervision and approval of the physiotherapist, began performing the intervention. The stages of SSBM are as follows: The patient lies on a hard bed, and 20 small circular movements are made with the thumbs for 1 minute on the neck. Then the lumbar spine is massaged from the base of the skull to the sacrum with the palm of one hand, and this process is repeated on the other side of the spine with the palm of the other hand, while the first hand is moved towards the base of the skull. The number of movements was 60 times within 4 minutes. After that, 20 strokes are made with the thumb along the shoulder blades for 30 seconds. Strokes with the thumbs are made on both sides of the spine from the shoulder to the lower back for 1 minute. Then, sweeping strokes are made with both hands from the neck to near the sacrum with 40 movements within 3.5 minutes (15).
3.3. Data Collection and Analysis
The data collection tool was the PSQI, developed by Buysse et al. It includes 18 items with a 4-point Likert scale ranging from none = 0 to severe = 3, and seven subscales. The total score of the tool ranges from 0 to 21, with higher scores indicating poorer sleep quality. A score of 5 is the cut-off for distinguishing between good and poor sleep (16).
Data analysis was performed using SPSS software version 16, with P values less than 0.05 considered significant. The analysis utilized descriptive statistics, repeated measures tests, paired t-tests, and independent t-tests.
4. Results
Comparison of demographic characteristics before the intervention shows that there was no significant difference between the two groups (Table 1).
| Demographic Variables | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Sex | 0.59 | ||
| Female | 15 (50) | 14 (46.6) | |
| Male | 15 (50) | 16 (53.3) | |
| Education | 0.33 | ||
| Illiterate | 6 (20) | 5 (16.6) | |
| Elementary | 5 (16.6) | 7 (23.3) | |
| Diploma | 17 (56.6) | 15 (50) | |
| Bachelor and above | 2 (6.6) | 3 (10) | |
| Marital | 0.38 | ||
| Single | 4 (13.3) | 5 (16.6) | |
| Married | 19 (63.3) | 20 (66.6) | |
| Widow | 7 (23.3) | 5 (16.6) | |
| Income | 0.46 | ||
| Sufficiency | 11 (36.6) | 13 (43.3) | |
| Insufficiency | 19 (63.6) | 17 (56.6) | |
| Employment | 0.79 | ||
| Employed | 14 (13.3) | 13 (43.3) | |
| Unemployed | 16 (53.3) | 17 (56.6) | |
| Hemodialysis sessions | 0.55 | ||
| Twice a week | 18 (60) | 16 (53.3) | |
| Three times a week | 12 (40) | 14 (46.6) | |
| Hours of hemodialysis | 0.32 | ||
| Three hours | 21 (70) | 19 (63.3) | |
| More than three hours | 9 (30) | 11 (36.6) | |
| Age | 48.14 ± 12.33 | 47.88 ± 12.33 | 0.89 |
Comparison of Demographic Characteristics Between the Two Groups Before the Intervention a
The sleep quality in both groups showed no significant difference before the intervention (P = 0.156). The mean scores for all PSQI domains, except for daytime dysfunction, significantly decreased after the intervention compared to baseline and on the 15th and 30th days (P < 0.05) (Table 2).
| Sleep Quality Domain | Control Group | Day 15th | Day 30th |
|---|---|---|---|
| Subjective sleep quality | |||
| Before intervention | 1.51 ± 0.85 | 1.48 ± 1.06 | 1.45 ± 0.85 |
| After intervention | 1.38 ± 0.84 | 1.36 ± 0.74 | 1.35 ± 0.98 |
| Paired t-test | 0.1 | 0.004 | 0.001 |
| Cohen's d | 0.23 | 0.16 | 0.11 |
| Sleep latency | |||
| Before intervention | 2.29 ± 0.86 | 2.03 ± 0.91 | 2.25 ± 0.93 |
| After intervention | 2.23 ± 0.88 | 1.68 ± 0.9 | 1.78 ± 0.81 |
| Paired t-test | 0.3 | 0.03 | 0.001 |
| Cohen's d | 0.06 | 0.38 | 0.58 |
| Sleep duration | |||
| Before intervention | 1.71 ± 0.99 | 2.16 ± 0.86 | 1.93 ± 0.96 |
| After intervention | 1.67 ± 1.04 | 1.75 ± 0.88 | 1.51 ± 0.84 |
| Paired t-test | 0.3 | 0.002 | 0.001 |
| Cohen's d | 0.04 | 0.47 | 0.5 |
| Sleep efficiency | |||
| Before intervention | 2 ± 1.06 | 2.35 ± 0.98 | 2 ± 0.1 |
| After intervention | 2.06 ± 1.06 | 1.92 ± 1.05 | 1.74 ± 1.05 |
| Paired t-test | 0.3 | 0.02 | 0.03 |
| Cohen's d | 0.05 | 0.43 | 0.26 |
| Sleep disturbances | |||
| Before intervention | 1.53 ± 0.61 | 1.54 ± 0.67 | 1.67 ± 0.54 |
| After intervention | 1.58 ± 0.67 | 1.42 ± 0.67 | 1.51 ± 0.58 |
| Paired t-test | 0.9 | 0.04 | 0.04 |
| Cohen's d | 0.08 | 0.17 | 0.29 |
| Sedative medication use | |||
| Before intervention | 1.48 ± 1.18 | 2 ± 0.1 | 1.67 ± 1.16 |
| After intervention | 1.45 ± 1.15 | 1.57 ± 1.03 | 1.48 ± 0.97 |
| Paired t-test | 0.3 | 0.001 | 0.003 |
| Cohen's d | 0.02 | 0.43 | 0.19 |
| Daily functioning impairment | |||
| Before intervention | 1.32 ± 0.7 | 1.54 ± 0.67 | 1.58 ± 0.76 |
| After intervention | 1.45 ± 0.72 | 1.39 ± 0.68 | 1.33 ± 0.62 |
| Paired t-test | 0.1 | 0.2 | 0.04 |
| Cohen's d | 0.18 | 0.22 | 0.40 |
. Comparison of the Mean Scores of Components of Pittsburgh Sleep Quality Index Before and After the Intervention a
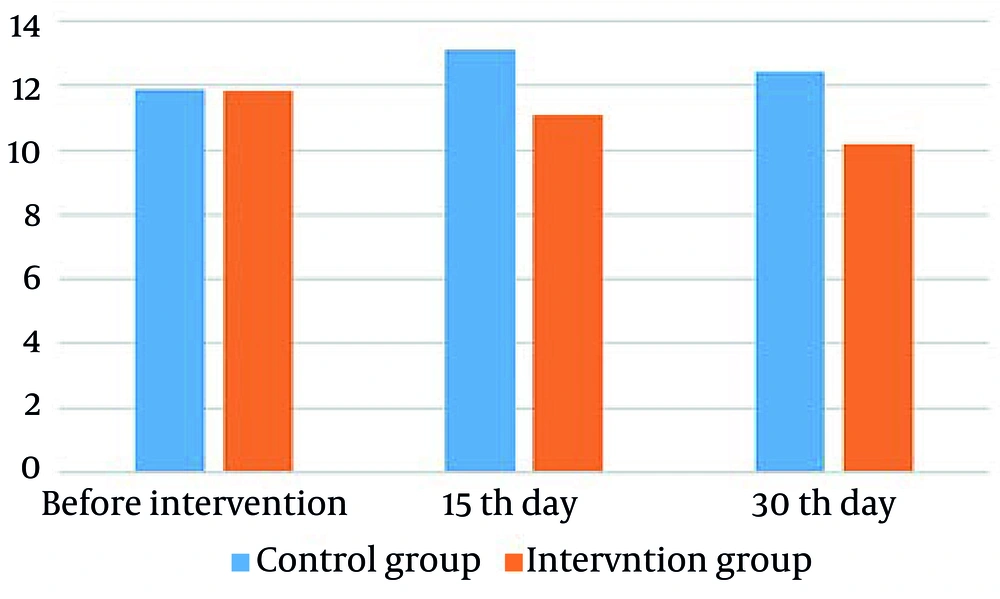
The results showed that the mean PSQI before the intervention in the intervention and control groups was 11.82 ± 6.36 and 11.89 ± 6.32, respectively. On the 15th day after the intervention, the mean PSQI in the intervention and control groups was 11.09 ± 5.95 and 13.1 ± 6.15, respectively. On the 30th day, the mean PSQI in the intervention and control groups was 10.19 ± 5.39 and 12.55 ± 6.2, respectively. The repeated measures test showed that SSBM significantly improved the sleep quality of patients (P < 0.001) compared to before the intervention, and on the 15th and 30th days in the intervention group. Although the sleep quality of the control group worsened on the 15th day, this change was not statistically significant (P > 0.05) and may have been due to other underlying factors such as stress that were beyond the researcher's control (Table 3).
| Variables | Intervention Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD Changes | Repeated Measures Test | Mean ± SD | Mean ± SD Changes | Repeated Measures Test | |
| Time point | F = 7.1, P > 0.001, Df = 2 | F = 4.2, P > 0.131, Df = 2 | ||||
| Before intervention | 11.82 ± 6.36 | - | 11.89 ± 6.32 | - | ||
| Day 15th | 11.09 ± 5.95 | 0.73 ± 4.2 | 13.1 ± 6.15 | 1.21 ± 5.9 | ||
| Day 30th | 10.19 ± 5.39 | 1.63 ± 3.9 | 12.55 ± 6.2 | 0.66 ± 5.4 | ||
Mean and Difference in Sleep Quality Scores of Hemodialysis Patients in Intervention and Control Groups
The independent t-test revealed that the sleep quality of patients in the intervention group was significantly better than that in the control group at the end of the 15th and 30th days (P < 0.05) (Figure 2). Sleep quality in the SSBM group significantly improved (P < 0.001) (Table 4).
| Variables | Mean Differences | SE | Degrees of Freedom | t | P-Value |
|---|---|---|---|---|---|
| Before intervention | 0.03 | 0.421 | 58 | 0.523 | 0.156 |
| Day 15th | 4.99 | 0.365 | 58 | 0.385 | 0.023 |
| Day 30th | 3.64 | 0.657 | 58 | 0.374 | 0.026 |
Comparison of Mean Sleep Quality Scores of Hemodialysis Patients Between the Intervention and Control Groups
5. Discussion
The findings indicated that SSBM improved sleep quality in all domains, except for daytime dysfunction. A study by Mirawati revealed a significant difference in four components of sleep quality: Subjective sleep quality, sleep latency, sleep efficiency, and daytime dysfunction, as well as the overall sleep quality score in elderly individuals after massage. However, no differences were observed in three domains: Use of sleep medications, sleep disturbances, and sleep duration (17). The discrepancy between results could be attributed to the fact that Mirawati focused on an elderly population that generally experiences more sleep problems, and perhaps a more extended intervention would be needed.
A study by Hojat Ansari et al. showed improvement in sleep quality in SSBM or hot stone massage groups. However, no difference was found between the two intervention groups with increasing massage durations (18). Unlike this study, the current research did not use two intervention groups. However, it only assessed the effect of massage on sleep quality in one group at two time points, with significant results. The results confirmed that SSBM improved sleep quality in the intervention group compared to before the intervention and on the 15th and 30th days.
Studies by Sihaloho et al. and Oshvandi et al. indicated that the time to fall asleep or return to sleep after waking up significantly decreased following massage (19, 20), which aligns with the results of the current study.
Studies by Naderi et al., Cecen and Lafci, and Doner and Tasci showed improved sleep quality, depression, stress, anxiety, pain, fatigue, and quality of life between two groups during all follow-up weeks after the intervention (21-23). Contrary to the results of the present study, Williamson et al. showed there was no difference between sleep adequacy scores in the massage therapy and control groups (24). The lack of consistency may be attributed to the study population, as the research by Williamson focused on postmenopausal women, and the physiological and psychological changes during this period can affect sleep in women. Additionally, massage in cancer patients did not show a significant decrease in fatigue, pain, and discomfort (25). One of the main reasons for this could be that fatigue, pain, and discomfort in cancer patients are often chronic, so massage interventions may need to be applied over a more extended period.
Considering the effect of massage on patients' sleep quality, it is suggested that future studies compare the effect of massage with other complementary medicine methods on patients' sleep quality. Also, the effect of the amount of pressure applied during massage, the duration of massage, and different times of massage on patients' sleep should be investigated.
In terms of research limitations, given that sleep quality is a subjective phenomenon, many factors such as individual factors, family problems, and cultural and social differences affect it, which could not be controlled by the researchers. Additionally, the need for patients to go to the dialysis department in the afternoon can also be one of the possible factors affecting the results, as most of the patients had dialysis in the morning shift. One of the strengths of this study is that it effectively improved sleep quality in patients, such as increasing sleep duration, falling asleep faster, and sleeping better without any side effects.
5.1. Conclusions
Based on the results, implementing massage therapy programs can improve patients' psychological symptoms and sleep quality. This is because massage therapy can be applied in various settings without specific equipment or the side effects associated with medications. The findings of this study can be utilized by health policymakers, nurses, and healthcare providers in hemodialysis units and other medical groups to incorporate non-pharmacological methods into the treatment and care plans for patients.