1. Background
A high-risk pregnancy is any situation that has a potential risk for the mother or fetus (1). One in four women with risk factors of high-risk pregnancies is prone to maternal or neonatal complications; however, in those with low-risk pregnancies, it is only 10% (2). Regarding labor and delivery, optimizing maternal and neonatal outcomes is the most important obstetrical care milestone. The World Health Organization has developed the standards for the improvement of the quality of maternal and newborn care (3). Based on this guideline, labor induction by augmentation should be used only in the facilities capable of close, regular monitoring of the fetal heart rate (FHR) and the pattern of uterus contraction and can manage the adverse effects (3).
Hypoxia during labor might be due to the compression of the umbilical cord or decreased placental perfusion during the contraction of the uterus, which is evident in the late decelerations (4). These changes are identified by cardiotocography (CTG) that should be documented for at least 30 minutes before the administration of oxytocin. Continuous CTG is advised in the time that oxytocin is used up to delivery (5). With a nonreassuring CTG pattern, the midwife or obstetrician indicated urgent clinical assessment that is the first step in reducing or stopping the oxytocin administration (5).
Continuous electronic fetal monitoring during childbirth is challenging. However, healthy women without complications would be considered low-risk and can use intermittent auscultation. The indications for continuous monitoring are preeclampsia, suspected intrauterine fetal growth restriction, diabetes, and preterm labor (6). A routine admission CTG in clinical use, especially in low-risk pregnancy, increases unnecessary cesarean delivery without the improvement of neonatal outcomes (7).
The National Institute for Health and Care Excellence (NICE) (8) has categorized CTG into reassuring, nonreassuring, and abnormal forms. The initial management of nonreassuring features includes the modification of any underlying reasons, such as hypotension or uterine hyperstimulation (8). Monitoring indications in low-risk and high-risk pregnancies and their effects on neonatal outcomes have been investigated in previous studies; nevertheless, insufficient information on the differences in fetal distress with nonreassuring CTG has been investigated that is believed to help make decisions faster and reduce neonatal complications.
2. Objectives
This study aimed to evaluate arterial cord blood gases, Apgar scores, and admission to the neonatal intensive care unit (NICU) in high-risk and low-risk pregnancies with nonreassuring CTG 30 minutes before delivery to see if high pregnancies need different or more care or not.
3. Methods
3.1. Study Setting
This retrospective cohort study was carried out in the Labor Department of Yas Hospital, an academic center affiliated with Tehran University of Medical Sciences, Tehran, Iran, within October 2017 and January 2020. This study was approved by the Institutional Ethical Board of Tehran University of Medical Sciences (reference code: 22496).
3.2. Eligibility Criteria
The inclusion criteria were singleton term pregnancy with nonreassuring CTG in the last 30 minutes before delivery. Patients whose fetuses or newborns had structural or genetic abnormality were excluded from the study. The women who were admitted for scheduled cesarean delivery, noncephalic presentation, and missed data of neonatal outcome were also excluded.
3.3. Participants
The participants were divided into high-risk and low-risk pregnancies. High-risk pregnancies were defined as preeclampsia (mild or severe), eclampsia, insulin-dependent diabetes, placenta abruption, oligohydramnios, intrauterine growth restriction, maternal fever due to chorioamnionitis, and preterm and postterm labors. All FHRs were recorded with an electronic fetal monitoring machine (EDAN, China). All tracings were reviewed by three obstetricians, who were blinded to neonatal outcomes. The results were checked, and any conflicts were solved by discussion. The demographic and obstetrical data and the different types of nonreassuring CTG were described in a questionnaire. The intraobserver and interobserver reliability of this questionnaire was higher than 90% and 85%, respectively.
3.4. CTG Categories
The NICE has categorized CTG into reassuring, nonreassuring, and abnormal forms. Nonreassuring features include 100 - 109/161 - 180 beats/minutes as baseline beat, less than 5 beats/minutes variability for 30 - 50 minutes/variability more than 25 beats/minutes for 15 - 25 minutes, variable decelerations for 90 minutes or more/variable decelerations with any concerning characteristics in up to 50% of contractions for 30 minutes or more/variable decelerations with any concerning characteristics in over 50% of contractions for less than 30 minutes/late decelerations in over 50% of contractions for less than 30 minutes, with no maternal or fetal clinical risk factors, such as vaginal bleeding or significant meconium (8). The overshoot, shoulder, tachycardia, and slow return to base patterns as the suspicious variants of CTG were also evaluated in this study.
3.5. Neonatal Outcomes
Neonatal outcomes were defined as umbilical cord pH < 7.1 at birth, Apgar score < 7 at the 1st and 5th minutes, and admission to the NICU. Immediately after delivery, the cord clamping was performed for all fetuses by an obstetrician resident. While the placenta was still in situ, the cord was double clamped at a minimum length of 10 cm, and the artery was sampled in 2 cc preheparinized syringes and analyzed within 10 minutes.
3.6. Statistical Analysis
Categorical variables were presented as absolute frequencies and percentages. Proportions were compared using the chi-square test or Fisher’s exact test. Statistical analysis was carried out by SPSS software (version 20). A P-value less than 0.05 was considered statistically significant.
4. Results
Among 622 patients who were included in the study, 322 women met the criteria for high-risk pregnancy, and the remaining 300 women were categorized as the low-risk group. Table 1 shows the demographic and delivery characteristics of the participants.
| Maternal Age (y) | Fetal Weight (g) | Gravid | Gestational Age in Delivery (Week) | Bloody AF | Meconium AF | Vaginal Delivery | Cesarean Section |
|---|---|---|---|---|---|---|---|
| 28.7 ± 5.7 | 3067 ± 64.7 | 2.0 ± 1.3 | 38.3 ± 2.1 | 27 (4.5) | 97 (15.5) | 427 (69.4) | 188 (30.6) |
Abbreviation: AF, amniotic fluid.
a Values are expressed as mean ± SD or No. (%).
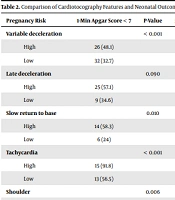
The neonatal outcomes, such as NICU admission, low Apgar scores in the 1st and 5th minutes, and pH < 7.1, were significantly different between high-risk and low-risk mothers with variable deceleration, tachycardia, and overshoot pattern (Table 2). High- and low-risk pregnancies with late deceleration had only significantly different Apgar scores in the 5th minute (P = 0.048). In the slow return to base features, the Apgar scores in the 1st and 5th minutes and NICU admission were significantly different in high- and low-risk groups. Moreover, NICU admission and low Apgar score in the 1st minute were higher in high-risk women in shoulder patterns (Table 2). As observed in Table 2, All adverse neonatal outcomes were more common in high-risk mothers with variable deceleration, slow return to base patterns, and shoulder patterns, except pH < 7.1 at birth.
| Pregnancy Risk | 1-Min Apgar Score < 7 | P-Value | 5-Min Apgar Score < 7 | P-Value | NICU Admission | P-value | pH < 7.1 | P-Value |
|---|---|---|---|---|---|---|---|---|
| Variable deceleration | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||
| High | 26 (48.1) | 14 (25.9) | 35 (64.8) | 20 (37) | ||||
| Low | 32 (32.7) | 3 (3.1) | 15 (15.3) | 10 (10.2) | ||||
| Late deceleration | 0.090 | 0.048 | 0.005 | 0.070 | ||||
| High | 25 (57.1) | 99 (28.6) | 26 (67.9) | 19 (46.4) | ||||
| Low | 9 (34.6) | 2 (7.7) | 11 (42.3) | 6 (26.1) | ||||
| Slow return to base | 0.010 | 0.049 | < 0.001 | 0.450 | ||||
| High | 14 (58.3) | 6 (25) | 18 (75) | 7 (29.2) | ||||
| Low | 6 (24) | 1 (4) | 6 (24) | 5 (20) | ||||
| Tachycardia | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||
| High | 15 (91.8) | 7 (43.8) | 16 (100) | 13 (81.3) | ||||
| Low | 13 (56.5) | 3 (13) | 21 (91.3) | 3 (13) | ||||
| Shoulder | 0.006 | 0.300 | < 0.001 | 0.200 | ||||
| High | 2 (100) | 0 | 2 (100) | 0 | ||||
| Low | 6 (18.2) | 0 | 1 (3) | 0 | ||||
| Overshoot | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||
| High | 4 (100) | 4 (100) | 4 (100) | 4 (100) | ||||
| Low | 2 (33.3) | 0 | 2 (33.3) | 1 (16) |
Abbreviations: min, minutes; NICU, neonatal intensive care unit.
a Values are expressed as No. (%).
5. Discussion
The results of the present study showed the existence of a significant higher proportion of neonatal adverse outcomes in high-risk pregnancies using nonreassuring CTG. Other studies have shown that variable deceleration and tachycardia were associated with fetal acidosis and thereby might develop fetal asphyxia. In addition, Dellinger et al. showed normal tracings were only 5.1% of Apgar scores < 7 at the 1st minute and 1.0% of Apgar scores < 7 at the 5th minute (9). Only 5.6% of the neonates in this group were admitted to the NICU. None of the neonates in this group was considered hypoxic.
Another study evaluated the relationship between the time spent in each FHR category during the last 2 hours before delivery and short-term neonatal outcomes. The results showed an increased chance of adverse short-term outcomes with increasing time in category II FHR patterns (10). Wood et al. showed the association of fetal acidemia and depth of variable decelerations. They reported that deeper variable decelerations are attributed to less fetal pH (11).
The current study showed that the cases with shoulder patterns and slow return to base had a higher frequency of Apgar scores < 7 at the 1st and 5th minutes and NICU admission; nevertheless, the present analysis failed to demonstrate a relationship between the aforementioned two patterns and pH < 7.1. Similarly, Cahill et al., in a retrospective cohort study, indicated that there was no association between shoulder patterns and acidemia (12).
In addition, Hamilton et al. compared fetal heart monitoring patterns of normal neonates with two groups with metabolic acidosis and no evidence of encephalopathy with acidosis and encephalopathy. They reported no association between atypical features of FHR and neonatal metabolic acidosis (13).
An important aspect of the current study is the comparison of neonatal outcomes and nonreassuring CTG regarding high-risk and low-risk pregnancies considering both mother’s condition and FHR tracing are vital for an appropriate decision to terminate the pregnancy. Another strength of the present study was the interpretation of FHR tracing by four independent obstetricians who were blinded to all clinical factors and outcome data.
There is a potential limitation in the current study. Part of the samples was related to retrospective recorded data that affected the precision of information. However, it was tried to conduct a supervised data collection. Despite this potential limitation, it is believed that the present study’s results contribute to the recent existing literature associating fetal heart monitoring type II with fetal acidemia and other birth outcomes in high-risk pregnancies.
5.1. Conclusions
Nonreassuring CTG near delivery might be accompanied by more fetal distress in high-risk pregnancies. Therefore, the nonreassuring features of CTG in high-risk pregnancies should be considered more important and might need prompt and timely action to decrease the adverse outcomes.