1. Background
Health organizations have been formed to maintain and promote public health. These organizations are a perfect example of social systems (1). So, the development of the health system will be possible along with socioeconomic development. Nowadays, by strengthening civic institutions, the leading health systems rely on public participation in many countries, thereby exploiting social potential (2-4). Public participation also provides the basis for making the government accountable in the health field (5).
The concept of public participation in the planning, delivery, and evaluation of healthcare services was first introduced by the World Health Organization (WHO) during the Alma Ata Conference in 1978 as one of the principles for achieving primary healthcare (6). According to the statement of this conference, the community has been viewed as a framework for planning, organizing, implementing, and controlling primary healthcare (7, 8). Decades after the conference, public participation is still one of the main effective and efficient strategies for progressing healthcare programs (7, 9).
As one of the fundamental rights associated with society, public participation refers to the process by which people take responsibility for a particular matter logically and consciously (10). During public participation, individuals try individually or in groups to satisfy the spiritual and psychological needs of themselves and others, and given the available facilities and limitations, they make efforts and cooperation to achieve the predetermined goals for a specific program (4, 9).
Health, as an index, is the axis and goal of community development, and without it, sustainable development will not be possible (11). Furthermore, health is a multidimensional concept influenced by various factors such as socioeconomic environment, physical environment, lifestyle, and heredity and, thus, is not merely affected by the health system and healthcare (12). Accordingly, providing and promoting health requires the participation of each individual in the community, and all development sectors, institutions, and related organs (13).
Nowadays, countries face complex healthcare challenges that challenge the capacity and flexibility of health systems, so it is important to focus on community participation (2, 9, 13). Public participation in health programs creates the opportunity to distribute health knowledge in the community and institutionalize health-related skills. Through participation, it is possible to provide more resources, reduce cost burden, and organize distributed resources at the community level, leading to strengthening the access of all individuals in the society, and basically, the realization of justice in health owes to the realization of the culture of participation (14). Therefore, over the past decades, governments have increasingly supported public participation as an essential tool for increasing health system accountability (2).
Community participation is a tool for working with the community to help create interventions related to local knowledge, needs, and priorities (12). Numerous studies conducted internationally on public participation during COVID-19 epidemic have indicated the effectiveness of this participation and its beneficial consequences (2, 4, 7, 9). In Iran, also, some studies on public participation and related institutions in the health field have shown the positive effects of this participation (13, 15, 16).
Effective public participation in the health system requires the identification and consideration of appropriate grounds and contexts, as well as necessary facilities and conditions for achieving participation. Lack of necessities, such as sufficient knowledge of the nature of the concept of social participation, a theoretical and operational definition for it, and an appropriate framework in this regard, confront participatory programs with major problems (8, 17). Evidence in Iran indicates the existence of some obstacles and challenges on the way to achieving public participation in the health system (17-19). In this regard, Gholamzadeh Nikjoo et al. concluded that charities need sustainable financial resources for better and more effective participation in healthcare, and coordination between them and government organizations needs to be strengthened (20). Nevertheless, the need for strengthening public participation in the health field in the upstream documents and long-term plans has been clearly emphasized. However, no study has been done in this field so far, and the lack of relevant evidence is quite noticeable.
2. Objectives
The present study was conducted to develop a model for attracting public participation in the country’s health system.
3. Method
This mixed research (quantitative-qualitative) was conducted from May 2019 to July 2020. The study steps included a comparative study, tool design and validation, and the development and finalization of the participation framework.
The comparative study was performed on the documents of five selected countries, including the United Kingdom, Mexico, Norway, Singapore, and Iran. These countries were selected because they were pioneers in the field of public participation in the health system and also the availability of the required information. Iran was also purposefully selected to identify the status of the research setting and the possibility of performing a comparative study. The required texts were obtained through a comprehensive search in the databases of PubMed, Scopus, Web of Science, and the Google Scholar search engine using keywords such as “public participation”, “social participation”, “community participation”, “model”, and “framework”. The Persian language databases such as SID, Irandoc, and Magiran were also searched for research evidence in Iran with the Persian equivalents of the mentioned keywords. All searches were performed with no time limit. Also, a manual search was performed to find relevant reports and documents both in Persian and English.
The required information was extracted from the obtained documents by the content analysis method. Accordingly, the effective factors in attracting public participation in the health system were classified by the research team into eight primary components, including information technology, organizational factors, economic factors, political-legal factors, social-humanitarian factors, psychological factors, cultural-religious factors, and contextual factors (Figure 1).
Using the findings of this stage and after holding an expert panel with expert individuals (6 people), a questionnaire consisting of 64 questions was developed. Inclusion criteria for individuals’ participation in the expert panel were having two of the following conditions: (1) conscious consent to participate in the panel; (2) having a Ph.D. degree in healthcare management and health policymaking; (3) a public participation-related executive position in the health system; and (4) public participation-related research activity in the health system. The designed questionnaire was then provided to 20 experts (second expert panel), including the faculty members in the field of health management and policy (9 people), health policymakers (5 people), and health system managers (6 people) to determine the validity.
The face validity of the questionnaire regarding the structure, appearance, and method of writing the questionnaire questions was examined and confirmed by making some corrections. Based on the results of the content validity, 16 questions were removed, and the writing of ten questions was reviewed. Finally, the questionnaire containing 48 questions was confirmed by calculating the content validity ratio (CVR) at the rate of 0.53 and the content validity index (CVI) at the rate of 0.85. Judgment regarding confirming validity according to the obtained criteria is based on the number of participants in the survey, which was equal to 20 individuals in this study (21). The reliability of the questionnaire was also confirmed by calculating Cronbach’s alpha equal to 0.81.
The field test of the public participation questionnaire was used to finalize the scale using exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The study population included all managers and employees in the Ministry of Health and the Universities of Medical Sciences. Inclusion criteria included having an associate’s degree or higher and having at least three years of executive or research experience (regarding public participation). Sampling was performed using the snowball sampling method in the Ministry of Health, as well as Tehran, Ahvaz, Mashhad, Isfahan, Tabriz, Sistan and Baluchestan, and Mazandaran Universities of Medical Sciences. The number of samples required for factor analysis is between 3 - 20 samples per variable of the questionnaire (22). In this study, the sample size was determined to be six times the number of questionnaire variables and equal to 288 people. Thirty questionnaires were copied on paper, and the rest of the questionnaires were distributed and collected electronically through email. Out of 288 distributed questionnaires, 283 questionnaires were completed and collected (response rate = 98.3%).
Using SPSS-v26 and AMOS-v26 software, EFA and CFA were performed to finalize the public participation model. Before performing the analysis, the normality of the distribution of variables was evaluated using the Kolmogorov-Smirnov test, and the normality of the data was confirmed (P < 0.05). To measure the suitability of the variables for EFA, the Pearson correlation matrix was calculated for the data, and factor sharing and extraction were estimated. The results of the Kruit-Bartlett test were statistically significant (P < 0.001). Therefore, according to the results of the mentioned test, it can be inferred that the implementation of factor analysis based on the obtained correlation matrix is explainable, and the amount of available data, based on the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy, was able to perform factor analysis (23).
Three indices were considered to determine that the measurement tool under review has been saturated with how many factors: (1) eigenvalue; (2) the ratio of variance explained by each factor; and (3) a rotated diagram of eigenvalue called Scree. To extract the appropriate factors in harmony with the cultural and social structure of the sample, factor analysis was performed several times with different solutions. Finally, it was found that the 8-factor solution was more adequate, and this solution was applied. Fit indices obtained from the implementation of this method include estimating the chi-square test (χ2), the chi-square ratio to the degree of freedom (χ2/df), the goodness-of-fit index (GFI), the adjusted goodness-of-fit index (AGFI), the comparative fit index (CFI), and the root mean square error of approximation (RMSEA), as well as T-values (24). By measuring the regression coefficients of the CFA model, it was observed that all coefficients were significant at the 5% level. Therefore, with the use of the CFA model, the study validation and final model were confirmed, and thus the effective factors in attracting public participation in the Iranian health system and the impact rate of each factor were determined.
Written informed consent was obtained from all participants. Also, the information obtained from the participants was kept confidential and used only for the research aims. Other ethical considerations were also considered, including non-bias in the selection of samples, as well as in the analysis and interpretation of the findings.
4. Results
The status of the participants’ demographic variables is presented in Table 1. According to the findings presented, most of the participants (35.3%) were in the age range of 31 - 40 years, 55.7% were male, and 61.2% were married. Also, most of the participants (37.1%) had a master’s degree and 31.1% were employees.
| Variables | No. (%) |
|---|---|
| Age (y) | |
| 20 - 30 | 67 (23.8) |
| 31 - 40 | 100 (35.3) |
| 41 - 50 | 81 (28.6) |
| > 50 | 35 (12.3) |
| Gender | |
| Male | 125 (44.3) |
| Female | 158 (55.7) |
| Marital status | |
| Single | 82 (29.2) |
| Married | 174 (61.2) |
| Others | 27 (9.6) |
| Level of education | |
| Bachelor of Science | 73 (25.4) |
| Master of Science | 105 (37.1) |
| Medical Doctor | 71 (25.0) |
| Doctor of Philosophy | 34 (12.5) |
| Job | |
| Clerk | 88 (31.1) |
| Manager | 63 (22.2) |
| Student | 62 (21.9) |
| Faculty member | 45 (15.9) |
| Retired | 20 (7.1) |
| Others | 5 (1.8) |
Socio-demographic Characteristics of the Participants
The participants completed the final questionnaire with 48 questions reported in Table 2.
| Factors | Number of Questions | Questions |
|---|---|---|
| Citizenship rights and customer orientation | 16 | To what extent does people’s pride in having healthy people lead to public participation? |
| To what extent does organizational decentralization in the health system lead to public participation? | ||
| To what extent does providing at-home services lead to public participation? | ||
| To what extent does the emphasis of national health system policies on people’s participation lead to public participation? | ||
| To what extent does the response of authorities to people’s complaints about the performance of the health system lead to public participation? | ||
| To what extent does the provision of social care for adults lead to public participation? | ||
| To what extent does the mutual feedback between the participants and the health system lead to public participation? | ||
| To what extent does people’s confidence in the quality of health services lead to public participation? | ||
| To what extent does the use of community-oriented approaches in providing services lead to public participation? | ||
| To what extent does the removal of taxes from healthcare services lead to public participation? | ||
| To what extent does allocating financial and human resources for people’s participation in the health system lead to public participation? | ||
| To what extent does the creation of spaces for people’s participation, such as "participation houses" lead to public participation? | ||
| To what extent does the proper communication between health system authorities and charitable and voluntary organizations lead to public participation? | ||
| To what extent does supporting health ambassadors and liaisons lead to public participation? | ||
| To what extent does the existence of people’s and patients’ representatives on the board of directors of healthcare service providers lead to public participation? | ||
| To what extent does the reduction of tenure of the Ministry of Health (MoH) lead to public participation? | ||
| Social and economic factors | 14 | To what extent does the proper communication between medical staff and patients lead to public participation? |
| To what extent does responsibility based on cultural indicators lead to public participation? | ||
| To what extent does the appropriate response of the health system to emergency situations and disasters lead to public participation? | ||
| To what extent does the use of various information channels to inform people about health conditions lead to public participation? | ||
| To what extent does encouraging people to participate in altruistic issues lead to public participation? | ||
| To what extent does health service providers’ compassion with people lead to public participation? | ||
| To what extent does improving school health lead to public participation? | ||
| To what extent does the existence of the organization in charge of attracting people’s participation in the structure of the health system lead to public participation? | ||
| To what extent does attracting people’s financial aid in special diseases lead to public participation? | ||
| To what extent does “collective participation” as one of the organizational goals lead to public participation? | ||
| To what extent does the government grant subsidies to NGOs lead to public participation? | ||
| To what extent does creating appropriate processes for participation lead to public participation? | ||
| To what extent does the decentralization of financial responsibilities lead to public participation? | ||
| To what extent does promoting the culture of participation lead to public participation? | ||
| Communication with people and non-governmental organizations | 6 | To what extent does active participation in the health field to gain spiritual status lead to public participation? |
| To what extent does paying attention to people’s mental health lead to public participation? | ||
| To what extent does access to services by the middle and lower classes of society lead to public participation? | ||
| To what extent does the continuous improvement of the quality of health services technologies lead to public participation? | ||
| To what extent does the creation of comprehensive databases of participants lead to public participation? | ||
| To what extent does patient-centered care lead to public participation? | ||
| Research and technology factors | 7 | To what extent does the observance of patients’ rights lead to public participation? |
| To what extent does paying attention to public demands in participatory plans lead to public participation? | ||
| To what extent does the monitoring and evaluation of public participation process lead to public participation? | ||
| To what extent does providing health announcements in public places lead to public participation? | ||
| To what extent does the expansion of primary health care coverage lead to public participation? | ||
| To what extent does improving the level of health literacy in the society lead to public participation? | ||
| To what extent does research based on people’s participation in the health system lead to people’s participation? | ||
| Managerial and organizational factors | 5 | To what extent does the observance of the principles of democracy at the community level lead to public participation? |
| To what extent does the raising of health-related issues by influential and famous people (celebrities) lead to public participation? | ||
| To what extent does awareness of social and citizenship rights lead to public participation? | ||
| To what extent does determining the ways of communication between NGOs and governmental organizations and legislators lead to public participation? | ||
| To what extent does the prioritization of public participation by its authorities in the health system lead to public participation? |
Factors, Number of Questions per Factor, and Questions
The KMO index, which indicates the adequacy of the sample size for factor analysis, was measured at the rate of 0.932 and in the desired range. Factors were extracted using principal component analysis by varimax rotation. The obtained results showed that the first five factors, with a factor loading of higher than one, explained the highest variability of the variables’ variance and more than 80% of the variance of the variables related to the study aim. Then, after consulting the experts, the five identified factors were named as follows (Table 3).
| Factors | Mean ± SD | Cronbach’s Alpha |
|---|---|---|
| Citizenship rights and customer orientation | 38.58 ± 16.91 | 0.96 |
| Social and economic factors | 34.97 ± 14.98 | 0.90 |
| Communication with people and non-governmental organizations | 15.01 ± 6.84 | 0.94 |
| Research and technology factors | 15.94 ± 7.42 | 0.84 |
| Managerial and organizational factors | 11.28 ± 5.16 | 0.92 |
Descriptive Statistics and Cronbach’s Alpha of Factors Extracted from Exploratory Factor Analysis
The inter-correlation of factors was investigated using Pearson correlation coefficients among the five factors, which gave a correlation coefficient higher than 0.8 and a significance level of less than 5%. The results showed a high and significant correlation among factors (Table 4).
| Factors | Citizenship Rights and Customer Orientation | Social and Economic Factors | Communication with People and Non-governmental Organizations | Research and Technology Factors | Managerial and Organizational Factors |
|---|---|---|---|---|---|
| Citizenship rights and customer orientation | 81.091 | 110.804 | 106.715 | 218.086 | 286.010 |
| Social and economic factors | 68.014 | 97.454 | 91.080 | 224.677 | 218.086 |
| Communication with people and non-governmental organizations | 31.224 | 45.411 | 46.812 | 91.080 | 106.715 |
| Research and technology factors | 34.920 | 55.076 | 45.411 | 97.454 | 110.804 |
| Managerial and organizational factors | 26.637 | 34.920 | 31.224 | 68.014 | 81.093 |
The Results of Correlation Analysis Between Factors
To show that the data correlation matrix in the population is not zero, the Kruit-Bartlett test was used, and the obtained results were statistically significant (P < 0.001). Therefore, based on the results of the mentioned test, it can be found that the implementation of factor analysis based on the obtained correlation matrix is explainable (Table 5).
| Tests | Results |
|---|---|
| Kaiser-Meyer-Olkin | 0.932 |
| Bartlett’s test | |
| Approx. chi-Square | 4004.977 |
| df | 28 |
| Sig. | 0.000 |
The Results of Kaiser-Meyer-Olkin and Bartlett’s Test
The CFA was used to confirm the model extracted from the EFA. Findings of the CFA showed that the five factors, including citizenship rights and customer orientation, socioeconomic factors, communication with people and non-governmental organizations (NGOs), research and technology, and managerial and organizational factors, significantly affected the formation of public participation in the Iranian health system. Among these five factors, citizenship rights and customer orientation with a factor loading of 0.967 had the most impact, and research and technology, with a factor loading of 0.944 had the least impact. Also, communication with people and NGOs, managerial and organizational factors, and socioeconomic factors had factor loadings of 0.957, 0.955, and 0.951, respectively.
The model fit was measured using the χ2/df index less than the recommended value, which indicated the model suitability. The RMSE index was lower than the allowable limit (< 0.08) and in the desired size. In addition, GFI, NFI, and CFI indices were measured more than the allowable limit (< 0.9) and at the rate of 1 (Table 6).
| Fit Indexes | Optimal Amounts | Results |
|---|---|---|
| χ2/df | < 3 | 2.219 |
| RMSE | < 0.08 | 0.071 |
| RMR | < 0.05 | 0.00 |
| GFI | > 0.9 | 1 |
| NFI | > 0.9 | 1 |
| CFI | > 0.9 | 1 |
The Results of Kaiser-Meyer-Olkin and Bartlett’s Test
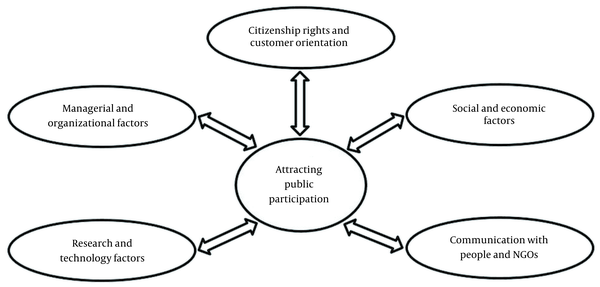
According to the findings of CFA, the final framework of public participation in the Iranian health system was developed in the form of the five main factors (Figure 2).
5. Discussion
This research was performed to develop a framework consisting of the effective factors in attracting public participation in the Iranian health system. The five factors, including citizenship rights and customer orientation, socioeconomic factors, communication with people and NGOs, research and technology, and managerial and organizational factors, significantly affected the formation of public participation in the Iranian health system. Citizenship rights and customer orientation was recognized as the most effective factor in attracting public participation in the health system. Ensuring citizenship rights and customer orientation and attention to it in the current age is very important when we see high levels of development in the communities (25). Nowadays, due to the continuous efforts of civil institutions and human rights organizations, the indices of citizenship rights have been developed, and the raise of public awareness has also forced the government to observe these rights and has changed into a public demand. Accordingly, attention to citizenship rights and customer orientation is viewed as one of the main pillars of the success of organizations in the social context (26).
In a study, Keshavarz Mohammadi and Bahreini emphasized the role of the government’s political commitment to the successful implementation of programs and justification of the people and all stakeholders in the effective promotion and continuation of the program and the use of indigenous forces, as well as entrusting executive and managerial responsibilities to the main stakeholders on community participation in health promotion programs (27). The findings of the mentioned study are consistent with the findings of the present study concerning the importance of satisfying the people and the necessity of justifying them as a citizenship right in the implementation of health promotion programs. Also, similar to the findings of the present study, a study conducted in the UK healthcare system showed that observing citizenship rights and paying attention to citizens as the main stakeholders in the health field were among requirements of community participation in the healthcare domain (28).
Communication with the people and NGOs was recognized as the second effective factor in attracting public participation in the Iranian health system. Mutual and comprehensive communication is necessary to fully understand the social context. Also, due to their social status, NGOs have a high potential for alignment with the community in a certain direction (29, 30). Non-governmental organizations in the health field can provide the basis for mobilizing public resources and actions in a specific domain (30). In their study, den Broeder et al. also showed that the relationships between communities and local organizations, policymakers, and professionals, as well as the empowerment of community members, can be one of the effective factors in public participation in health programs (31). In Iran, the findings of Akhavan Behbahani et al.’s study have also shown that communication with society, especially NGOs as representatives of the community, is one of the pillars of public participation in health legislation (32). According to the findings of the mentioned study, today, poor communication with the people and the lack of a context for NGOs’ participation are among the major challenges in this regard (32).
The managerial and organizational factors were identified as another effective factor in attracting public participation in the health system. Attracting public participation in the health field and managing this process requires numerous capacities in the managerial and organizational fields. Without the existence of these capacities, the health system will not be able to benefit from the potential of public participation effectively and efficiently, and mismanagement in this area may even lead to wasting resources and people refusing to participate (8, 13, 19). Rock et al. concluded that creating structures and organizations, that facilitate social participation through planning and policymaking can lead to community participation in health promotion (33). The findings of a study by Khodayari-Zarnaq et al. in Iran showed that from the perspective of NGO managers, it is necessary to create organizational and managerial infrastructures to improve the participation of these organizations in health policy making (19), which is consistent with the findings of the present study regarding the importance of managerial and organizational factors.
The socioeconomic factors were the fourth important factor affecting public participation in the health system. The socioeconomic status of any society determines the degree of desire and ability of that society to actively participate in the health field. The socio-macroeconomic status of each country affects the ability of the government to attract public participation (34). In a study, Howard-Grabman et al. introduced supportive and financial policies as key facilitators in healthcare participation (35). They have suggested that through financial support, policymakers should provide the basis for participatory mechanisms in primary healthcare (35). In addition, the results of a review study by Matos and Serapioni on the evidence obtained in southern European countries, including Spain, Italy, Portugal, and Greece showed that public participation in the health field was an entirely social process (36). They also found that the economic situation of the people had a significant impact on their participation in the health field (36).
The research and technology factors were identified as the final effective factors in attracting public participation in the health system. Kilewo and Frumence have suggested poor communication and information sharing, as well as the lack of awareness of health programs, as factors preventing community participation in health (37). Azmal et al. also specified communication and information as important outcome variables regarding patient and community participation in the Iranian health system and stated that it was necessary to share accurate, timely, and useful information among health actors (38).
This is the first study, to our knowledge, to determine the dimensions of attracting public participation in the Iranian health system. Evidence from this study can be the basis for evidence-based decision-making to determine strategies to improve public participation. Despite its strengths, this study has some limitations. The most important of which was not benefiting from the opinions of experts in other fields as well as health actors (NGOs and charities) in explaining the dimensions for attracting public participation.
5.1. Conclusions
The findings of this study, by a scientific method and using the available evidence and experiences and also an opinion poll of health professionals of the country, have provided a framework for public participation in the health field. The final model presented in this research shows that paying attention to citizenship rights and customer orientation, developing quantitative and qualitative communication with people and NGOs, promoting managerial and organizational tools and structures, applying and strengthening socioeconomic factors at the level of society and the health system, and finally, using communication and information technology devices and developing and promoting applied research, make it is possible to help develop public participation in the country’s health system and consequently promote the health level of key stakeholders of the health system, namely the people. Using this framework, healthcare policymakers can adopt the best strategies for engaging public participation and improving the effectiveness of decisions through evidence-informed policymaking.