1. Background
Non-communicable diseases (NCDs) are one of the major global health challenges with an upward trend, affecting millions of people and responsible for 74% of deaths worldwide (1). NCDs reduce productivity and economic growth, with the highest impact in less-developed countries. This implies a serious threat to achieving the United Nations' Millennium Development Goals (2, 3). Intelligent and multifaceted responses with continued healthcare programs in a sustainable manner are required from healthcare systems in this regard (4). Maintaining and sustaining NCD prevention and control programs (NCD-PCP) over reasonably long periods is crucial to maximizing the impact of interventions and boosting health-related outcomes, particularly in low- and middle-income countries with fragile health systems and limited resources. Sustainable programs are more effective and result in the proper use of resources, healthier communities, and leadership support (5, 6). Sustainability is "the existence of structures and processes that allow a program to leverage resources to effectively implement and maintain evidence-based policies and activities." Sustainability is a complex concept that includes various aspects such as a solid organizational infrastructure, coordination of different clinical, political, academic, and technological sectors, and commitment and leadership (7).
As a middle-income country, Iran reports that 83.5% of deaths and 78.1% of all morbidity burdens are due to chronic diseases (8, 9). In response, the Iran Ministry of Health and Medical Education (MOHME) has developed several measures, including the National Document on the Prevention and Control of Non-communicable Diseases, the National Committee for the Prevention and Control of Non-communicable Diseases, the National Action Plan for NCDs 2015 - 2020, and the implementation of the WHO Essential Intervention Package (IraPEN) (10-13). Although all the necessary factors for implementing NCD-PCP programs are usually present at the beginning, the process is often delayed or even stopped after a short time due to financial, political, or other underlying factors (14).
2. Objectives
Therefore, it is essential to understand the status and factors related to the sustainability and continuity of such programs. The study aims to determine the sustainability state of NCD prevention and control programs in Iran and identify related challenges in various intra- and inter-organizational domains.
3. Methods
3.1. Context
The National Committee for NCD Prevention and Control in Iran developed a document called the 'National Document for the Prevention and Control of NCDs,' which consists of 13 goals, nine of which were proposed by the WHO based on the country's healthcare system priorities. This document was disseminated to governmental medical universities to develop provincial documents and establish university-based committees focused on preventing and controlling NCDs.
3.2. Study Design
In this mixed-methods study, we used a sustainability assessment tool to evaluate the current state of NCD-PCP sustainability in Iran and to identify challenges in various domains inside and outside of organizations that could impact sustainability. To obtain qualitative data on potential challenges and weaknesses for each domain, we conducted semi-structured interviews in the interviewees' workplaces (six interviews) or via phone calls (40 interviews) in Farsi (Persian) language, each lasting an average of 30 minutes. All interviews were recorded with participants' consent until no further information was provided (1). To enhance the consistency and accuracy of the study results, we applied the four criteria of credibility, confirmability, dependability, and transferability proposed by Guba and Lincoln (15).
3.3. Participants and Sampling
We sent questionnaires to NCD department managers at the provincial level of all universities affiliated with the Iranian MOHME. These managers are responsible for planning and monitoring the provincial action plan for NCDs. The only inclusion criterion was having at least three years of experience as a primary healthcare manager or related executive. The final list included 46 participants out of 56 possible respondents; 10 managers declined to participate.
3.4. Study Tools
The Program Sustainability Assessment Tool (PSAT) was adapted to match the conditions of the healthcare system in Iran (7). The PSAT is a reliable and user-friendly sustainability assessment instrument (16, 17) with forty 7-point Likert scale items in eight domains. Each domain consists of five questions and covers environmental support (ES), funding stability (FS), partnerships, organizational capacity (OC), program evaluation (PE), program adaptation (PA), communication, and strategic planning (SP).
3.5. Questionnaire Translation
First, the questionnaire in English was translated into Persian (forward translation step), and its accuracy was checked in one session (incorporation step). Next, the Persian version was back-translated by a fluent English speaker (backward translation step). The resulting English version was then compared to the original version, and necessary modifications were made to the final Persian version (comparison step).
3.6. Questionnaire Validation
Ten health professionals, including experts in health care management (2), health policy (2), public health (1), social medicine (1), NCDs (2), epidemiology (1), and general practice (1), were asked to evaluate the items in the final Persian questionnaire. They assessed the necessity, relevance, transparency, and simplicity of the items and provided comments for corrections or changes if needed. Items with a content validity index (CVI) and content validity ratio (CVR) of > 0.62, according to the Lawshe table for 10 expert panelists, were considered acceptable. Based on expert opinions, a new domain titled "law and governance" was added to the questionnaire (see Table 1). The questionnaire's internal consistency was assessed using Cronbach's alpha, and the agreement among interviewees was assessed using the intraclass correlation coefficient (ICC).
| Sustainability Domains | Cronbach’s Alpha | Intraclass Correlation Single | Mean ± SD [Min, Max] | Description |
|---|---|---|---|---|
| Environmental support | 0.86 | 0.61 | 3.38 ± 1.01 [1, 5.25] | An internal and external support climate of the program |
| Funding stability | 0.9 | 0.7 | 2.79 ± 1.03 [1,5.25] | A stable and coherent financial base for the program |
| Partnership | 0.73 | 0.41 | 3.17 ± 0.87 [1,5] | Connections between the program and its stakeholders |
| Organizational capacity | 0.9 | 0.65 | 3.49 ± 1.06 [1,5.8] | Internal support and resources needed to effectively manage the program and its related activities |
| Program evaluation | 0.9 | 0.69 | 4.07 ± 1.15 [1,6] | Program evaluation in different periods in order to identify weaknesses and then record and give feedback on the results |
| Program adaptation | 0.91 | 0.68 | 4.24 ± 1.12 [1,6.4] | Measures to ensure the continued implementation of the program under new conditions |
| Communication | 0.82 | 0.53 | 4.01 ± 1 [1,5.5] | Strategic communication with stakeholders and the public in the program |
| Strategic planning | 0.85 | 0.58 | 3.39 ± 1.15 [1,6.25] | Adoption of a guiding process for the directions, goals, and strategies of the program |
| Law and Governance | 0.86 | 0.57 | 3.27 ± 1.02 [1,5.4] | Internal and external law and political support for the successful implementation of the program |
| Overall Capacity for Sustainability | 0.85 | 0.47 | 3.54 ± 0.86 [1,5.15] | - |
Descriptive Statistics of Sustainability Domains (Each with Five Items)
3.7. Data Collection
The participants were asked to complete the Persian version of the PSAT either in written form via email or by using the provided electronic form of the questionnaire (survey.porsline.ir). Data collection was conducted in May-June 2021.
3.8. Data Analysis
Descriptive statistics were reported as mean ± SD and No. (%), and data analysis was performed using SPSS 27. The managers' qualitative opinions were analyzed using Graneheim and Lundman's approach (18). Immediately after each interview, the recorded contents were transcribed word for word from the audio recorder. The transcripts were then cross-checked with the notes taken during the interview sessions to ensure accuracy. During the data preparation stage, the participants' viewpoints were read several times to better understand the texts. Meaningful units were extracted and condensed into smaller units labeled with codes. The codes were grouped into different categories based on their similarities and differences, independently by two researchers from the research team. Finally, the data were adjusted through discussions and the resolutions of any disagreements during a meeting.
4. Results
4.1. Sustainability Evaluation of NCD-PCP
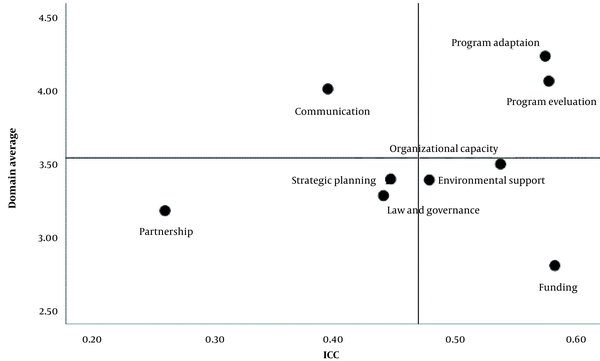
The participants' characteristics are summarized in Table 2. The questionnaire and its domains showed high internal consistency (overall Cronbach's alpha = 0.85, as shown in Table 1). There was acceptable agreement among interviewees, as indicated by the intraclass correlation coefficients in Table 1. The mean score of all nine domains was 3.54 ± 0.86. Among all domains, PA (4.24 ± 1.12) had the highest mean score, while FS (2.79 ± 1.03) had the lowest mean score. The joint ICC values and interviewees' mean scores on each domain are shown in Figure 1, following the interviewees' opinions from the qualitative section (Table 3).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 23 (50) |
| Female | 23 (50) |
| Job experience | |
| ≤ 20 | 19 (41.3) |
| 21 - 25 | 17 (37) |
| > 25 | 10 (21.7) |
| Level of education | |
| BSc. | 5 (10.9) |
| MSc. | 11 (23.9) |
| PhD.MD | 30 (65.3) |
| Occupation | |
| Physician | 29 (63) |
| Non-medical major | 17 (37) |
Managers' Demographic Characteristics (n = 46)
| Domains | Subdomains |
|---|---|
| Program evaluation | Lack of a comprehensive monitoring and evaluation program and shortcomings in the HIM system |
| Strategic planning | Lack of human resources; Negligence in holding joint meetings and providing related reports on the performance of each agency and deputy |
| Communication | Weaknesses in the skills related to using the capacities of the community and NGOs |
| Partnerships | Lack of transparency in the expectations of MHOME; Weaknesses in the skills related to seeking the support of experts and managers in terms of attracting inter-sectoral collaboration |
| Organizational capacity | Lack of skilled and trained human resources; no financial resources to compensate for employees' services along with the related motivational problems; multiple communications of programs; increased staff workload; non-transparency in job descriptions of programs |
| Environmental support | Insufficient support of national and regional policymakers; lack of understanding of policies and goals related to NCDs by senior managers; insufficient political support from the government |
| Law and Governance | Shortcomings in providing reports and feedback about the implementation of the action plan by each deputy |
| Funding stability | Insufficient allocations of specialized budgets for NCDs |
Expert Opinions on Sustainability Domains
4.1.1. Strong Sustainability-High Agreement Domains
The mean scores of the PA and PE domains were higher than those of the total domains. During the qualitative interviews, experts also mentioned:
"The non-communicable disease prevention and control program is somewhat in agreement with the climate of primary health care in Iran " (Expert 9)
The PE domain also had the second-highest mean score (4.07 ± 1.15) and a high ICC. During the qualitative interviews, some participants expressed their beliefs:
"The current evaluation system is not complete …" (Expert 12)
"Owing to the lack of a comprehensive monitoring and evaluation program, risk factors are not well surveyed in the community." (Expert 20)
Some participants also praised the risk-factor monitoring program and added:
"It is necessary to improve the evaluation system for the development of reliable information infrastructure." (Expert 15)
4.1.2. Strong Sustainability-Low Agreement Domains
The communication domain had a mean value of 4.01 ± 1 and ranked third compared to the total mean sustainability score, but there was low agreement among the participants. While some participants considered communication critical for the success and continuity of the program, others disagreed. One participant stated:
"The health deputy has launched loads of advertisements in the field of prevention and control of non-communicable diseases…” (Expert 7)
Some participants also mentioned:
"The lack of a high spirit and how to benefit from the hidden capacities… ". (Expert 14)
4.1.3. Poor Sustainability-Low Agreement Domains
According to the study results, the domain of SP, with a mean value of 3.39 ± 1.15, ranked fifth and was below the total mean score of sustainability. Furthermore, the participants had a low agreement regarding the importance of having an SP. In the qualitative interviews, some participants mentioned that determining the role and responsibilities of each stakeholder and executive agency in preventing and controlling NCDs was necessary for establishing and implementing the program. Problems were reported regarding holding joint meetings at the provincial level and supplying required resources.
For example, the participants said:
"The existing human resources do not meet the defined programs and goals." (Expert1)
The domain of law and governance (3.27 ± 1.02) was also in the seventh rank. In the qualitative interviews, it was reiterated as follows:
"In preparing the document and the action plan for the 13 goals of the national document at the provincial level, various university deputies and provincial organizations and agencies have been managed to cooperate, and even some roles and responsibilities have been assigned to each one." (Expert 3)
Furthermore, the domain of partnerships, with a mean value of 3.17 ± 0.87, ranked eighth and had the lowest level of agreement among the participants compared to the total mean sustainability score. In the interviews, the participants also mentioned:
"… the expectations of the Ministry of Health and Medical Education have not been clearly stated, and managers and experts in this field do not have the skills to seek support from other fields." (Expert 22)
4.1.4. Poor Sustainability-High Agreement Domains
There were three domains (organizational capacity, environmental support, and funding stability) with poor sustainability scores that experts had low agreements upon, as shown in Table 3. The following is a part of the participant's opinion on the domain of environmental support (ES).
"University presidents are indifferent to the non-communicable disease …." (Expert 10)
"Some programs have not received enough political support from the government due to conflicts of interest with the economy." (Expert 17)
Finally, the domain with the lowest mean score among sustainability domains was FS, with a mean score of 2.79 ± 1.03 and a very high level of agreement among participants. All participants agreed:
"We have faced a lack of sustainable funding for the non-communicable disease prevention and control program, and no specific budget has been thus far allocated to them." (Expert 5)
5. Discussion
In this study, we investigated the current state of the sustainability of NCD prevention and control programs and their challenges in various domains inside and outside the organization affecting sustainability. The overall sustainability was moderate, with the PA and FS domains having the highest and lowest sustainability, respectively. PA and FS are among the prominent domains of sustainability of every public health program (7). In Iran, integrating the NCD-PCP with the primary health care system has facilitated the adaptation of the program concerning cost-effectiveness and evidence-based interventions (19, 20). Previous studies in East Azerbaijan have reported offering integrated healthcare services to a specific population within a defined geographic area through health complexes (19, 21).
Funding is one of the major challenges for the sustainability of any program, especially in low- and middle-income countries (22). Almost all participants in the present study agreed that there was a severe shortage of financial resources and no clear sustainable financing plan. In Iran, the primary care system is completely funded by the government, and the treatment budget usually takes precedence due to the early returns (23). The NCD-PCP does not have a specific budget line, and despite the increase in the total share of health from the GDP, the disproportionate share of NCDs from the health budget has resulted in funding instability (24). In a study by Azizatunnisa, the health budget was allocated only to treatment and hospital facilities due to the local government's negligence of preventive measures and inadequate infrastructure in primary healthcare, which affected the sustainability of the vaccination program (25).
The participants identified some challenges to the sustainability of the low-scored 'PE' domain. Evidence suggests that setting appropriate, specific, and measurable goals and monitoring and evaluating them are necessary for the success and continuity of a healthcare program (26). Despite designing the goals of NCD-PCP in the form of national and provincial documents, the priorities are not well expressed, and the indicators are still scattered and incompatible (27, 28). The STEPwise approach to surveillance (STEPS) is among the measures developed to circumvent these issues (29). This project was designed to collect data continuously for decision-making and policymaking in the community (30). However, the centralized policymaking mechanism in the scope of NCDs limits the results provided by STEPS. Furthermore, the low quality of data collection and recording, especially regarding disease information, hinders effective evaluation and monitoring (27, 28). A properly designed and implemented national health information system could generate reliable data to help policymakers, managers, and researchers with evidence-based decision-making (31).
In contrast to results from other studies conducted in different countries, the NC-PCP in Iran faces issues with the communication domain (32). This domain was mainly affected by raising awareness and showing the program's values to the community. As mentioned in the qualitative interviews, various awareness-raising programs have been implemented in Iran to prevent and combat NCDs (33, 34). These programs include the food labeling campaign, the national campaign to control blood pressure, provincial and regional campaigns to increase physical activity, encourage dairy consumption, reduce salt, sugar, and oil use, quit smoking, and control anxiety (19, 35). However, managers and experts in charge of implementing these programs and campaigns need more knowledge and skills in involving and utilizing the capacities of the community and other institutions and insist on relying on limited governmental resources (36). In this regard, the UN General Assembly High-Level Meeting encourages identifying and mobilizing coordination and resources from non-governmental organizations (NGOs) and charities to reduce the burden of chronic diseases (37).
In regards to organizational capacity, the participants identified several commonly reported problems (32), including "lack of skilled and trained human resources," "no financial resources to compensate for employees' services along with related motivational problems," "communication of multiple simultaneous programs," "increased staff workload," and "non-transparent duty declaration." Efforts have been made to develop and build the capacity of human resources for NCD prevention and control. For instance, some health complexes in East Azerbaijan have implemented a program that has shown notable results in employee empowerment regarding prevention, lifestyle improvement, and the assignment of technical, professional, and managerial duties (19).
The experts regarding SP identified several obstacles. This included areas for improvement in involving intersectoral cooperation, holding joint meetings, and providing related reports. The Iranian High Council of Health and Food Safety evaluation indicated that a significant part of its intersectoral approvals still needs to be fully implemented (38-40). Evidence suggests minimal practice and poor participation of related departments in implementing the approvals by the provincial-level specialized working groups on health and food safety in the field of NCDs (41, 42). Incomplete infrastructure and a need for a transparent vision and comprehensive plans regarding the health duties and roles of other organizations and agencies have also resulted in unclear health-related expectations. Part of the reluctance from the organizations and agencies involved in health-related programs could be attributed to the improper appreciation of their efforts.
ES refers to a supportive climate within and outside the organization, including organizational procedures, policies, political and governmental support, and community members and leaders. We have discussed the internal aspects in previous domains to some extent. From an external perspective, non-professional and non-technical expectations of local political officials, who neglect health priorities and focus more on treatment, result in significant problems in primary health care and hinder the effective implementation of NCD-PCP (22, 43).
Experts in the law and governance domain have reported that reporting and feedback by participating agencies and deputies is a low-to-moderate problem. There are numerous laws, upstream documents, and national policies in the field of NCDs, including Articles 32 and 37 of the Fifth Development Plan in the Constitution of Iran, the National Non-communicable Disease Document, the National Health Reform Plan 2012, and the Macro Health Policies announced by the Supreme Leader of the Islamic Republic of Iran, among others. However, the coherence and coordination between them are not apparent, and the priorities of the NCD care system are not well-defined. The poor feedback on the performance and achievements of the organizations and agencies involved in NCD-PCP is attributed, at least in part, to the lack of appropriate indicators (27).
5.1. Limitations
One of the main limitations of this study was the widespread prevalence of COVID-19 during the study period. This prevented some top managers from participating in in-person interviews, so the interviews were conducted via phone instead.
5.2. Conclusions
Regarding the Iranian NCD-PCP, it is crucial to maintain and reinforce the current acceptable state of physical activity (PA) and physical education (PE). Funding instability is a barrier to the sustainability of any NCD-PCP, which could bring the whole program to a standstill, despite its sustainability in other domains. The possibility of shortages in financial resources should be acknowledged, and more cost-effective and efficient interventions should be adopted from the beginning of the program.