1. Background
Lifestyle practices encompass various characteristics influenced by regional, socioeconomic, cultural, and religious backgrounds, which impact daily attitudes and behaviors and have a comprehensive effect on an individual's overall health (1). Unfortunately, a substantial number of individuals worldwide adopt unhealthy lifestyle practices, leading to a diminished quality of life and an increased prevalence of non-communicable diseases (2). Notably, major contributors to this unhealthy lifestyle include smoking, alcohol consumption, sedentary behavior, and poor dietary habits resulting in weight-related issues (3). These well-established risk factors significantly contribute to the development of various non-communicable diseases, particularly cardiovascular disease (CVD) and other metabolic disorders (4). Cardiovascular disease has remained the primary cause of both mortality and morbidity in Malaysia over the past few decades (5). Based on national statistics, Malaysia witnessed 18,267 deaths attributable to ischemic heart disease in 2019, averaging 50 deaths per day. The escalating number of CVD cases presenting at public and private hospitals is concerning, both in terms of the community's compromised quality of life and the strain it places on the healthcare sector. The 2019 national health and morbidity survey (NHMS) revealed that 50% of the Malaysian population possesses one or more risk factors for CVD. While some drivers of CVD are non-modifiable, such as age, gender, ethnicity, family history of heart disease, and premature death, certain determinants can be controlled and modified to alleviate the burden of CVD. These determinants encompass hypertension, diabetes, and unhealthy lifestyle practices, including smoking, substance abuse, physical inactivity, and obesity (6). Smoking, alcohol consumption, obesity, and physical inactivity are key instigators of numerous clinical conditions that intensify the risk of CVD. These risk factors are significantly widespread within the Malaysian population. Of particular concern is tobacco use, which poses the greatest threat to public health. According to the World Health Organization, approximately 8 million people die each year due to tobacco smoking, with 80% of smokers residing in low- and middle-income countries. Despite the implementation of various primary prevention programs, the prevalence of these risk factors continues to escalate, as evident from reports by NHMS. These risk factors are interrelated, as physical inactivity can potentially contribute to obesity, which in turn is a risk factor for CVD. Additionally, smoking plays a role in the development of atherosclerosis, further increasing the risk of CVD. This study aimed to assess the prevailing lifestyle practices within the Kuala Lumpur community that contribute to an increased risk of CVD, given its status as the leading cause of death in Malaysia (7). The impact of CVD extends across all age groups, major ethnicities, and both genders within the Malaysian population (8).
2. Methods
This research encompasses a descriptive and inferential study that aims to investigate the lifestyle practices prevalent in the Kuala Lumpur community. The focus areas include smoking, alcohol consumption, dietary habits, and physical activity, which have a significant association with the incidence and mortality of CVD. The analysis delved into comprehensive details regarding physical activity, smoking, and alcohol consumption, along with individuals' intentions to adopt healthy practices. Anthropometric measurements were taken to calculate the body mass index (BMI), enabling the identification of the prevalence of overweight and obesity within the survey population (SP). The prevalence of these risk factors was further examined by comparing them across gender, age groups, and ethnic backgrounds.
The study obtained ethical approval from the ethical committee of the Management and Science University in Shah Alam, Malaysia. It was conducted as a cross-sectional survey, with data collected directly from participants. The sampling frame encompassed all eleven districts of Kuala Lumpur city, targeting residents aged 18 and above. Institutionalized individuals were excluded from the study. Considering the estimated population of 1.8 million in Kuala Lumpur, a sample size of 384 was determined with a margin of error of 0.05 and a 95% confidence interval. In the first stage, four districts (Wangsa Maju, Seputeh, Batu Caves, and Bukit Bintang) were randomly selected out of the eleven districts using simple random sampling. Subsequently, stratified random sampling was employed to ensure representation across all sociodemographic subgroups of the Kuala Lumpur community. The population was approached through various community venues. The survey was initiated in September 2019 with the aim of completing the estimated sample. However, due to disruptions caused by the COVID-19 pandemic, data collection was delayed and ultimately concluded with a total of 278 respondents in September 2020, following the prohibition of public gatherings.
A validated questionnaire, administered in person, was utilized as a tool in this study. The questionnaire collected information on the demographic characteristics of the survey participants, smoking history, height and weight for BMI calculation, and lifestyle practices. The questionnaire was available in both English and Bahasa Malaysia. The practice items pertaining to the prevention of CVD risk factors and intentions related to physical activity, healthy dietary habits, smoking, and alcohol consumption, were derived from the ABCD Risk Questionnaire developed by the national health services (NHS) in the United Kingdom (9). Participants rated their agreement with 15 statements using a Likert scale ranging from 0 to 4, where 0 represented "not applicable," and the scale progressed from "strongly disagree" to "strongly agree." Negative statements were reverse-coded. Higher sum scores indicated a greater perceived readiness to change specific behaviors. The practice items demonstrated good internal consistency, with a Cronbach's Alpha value of 0.854.
Anthropometric measurements, including height and weight, were taken using the SECA 213 stadiometer for mobile height measurement and the SECA 803 Digital Floor Scale, respectively. Height and weight values were rounded to the nearest tenth. The World Health Organization (WHO) criteria were employed to categorize BMI, where a BMI below 18.5 kg/m2 indicated underweight, a BMI ranging from 18.5 to 24.9 kg/m2 indicated a normal BMI, a BMI between 25 and 29.9 kg/m2 indicated overweight, and a BMI equal to or above 30 kg/m2 indicated obesity (10).
Descriptive and inferential analyses were conducted using SPSS software. The demographic characteristics of the SP were examined, and frequencies for smoking, BMI, and alcohol consumption were determined using a 95% confidence interval (CI). To compare lifestyle practices across gender, ethnic groups, and age groups, the chi-square test of independence was employed. Additionally, the chi-square test of goodness of fit was utilized to assess the disparities between the observed sample distribution and the expected probability distribution for smoking, alcohol consumption, and BMI prevalence.
The study encountered several limitations that are noteworthy. Due to the pandemic restrictions imposed after March 2020, accessing subjects through community camps became challenging. It should be acknowledged that the information obtained through surveys may not always be comprehensive and complete. There is a possibility of courtesy bias and social bias, as respondents may manipulate their responses. Quantifying attitudes remains a topic of controversy. Furthermore, in surveys conducted among multilingual and multicultural communities, linguistic challenges and potential misinterpretation of concepts may arise, which could potentially distort the data.
3. Results
A total of 278 adults were included in the study. Table 1 presents the socio-demographic characteristics of the SP, including gender, age, and ethnicity. Approximately half of the SP was in the 18 to 29-year-old age group (51.4%), and the majority belonged to the Malay ethnic group (52.5%).
| Demographic Groups and Sub-categories | No. (%) |
|---|---|
| Age | |
| 18 - 29 | 143 (51.4) |
| 30 - 39 | 55 (19.8) |
| 40 - 49 | 34 (12.2) |
| 50 - 59 | 28 (10.1) |
| > 60 | 18 (6.5) |
| Gender | |
| Male | 163 (58.6) |
| Female | 115 (41.4) |
| Ethnicity | |
| Malay | 146 (52.5) |
| Chinese | 22 (7.9) |
| Indian | 55 (19.8) |
| Other | 55 (19.8) |
Demographic Features of the Survey Population (n = 278)
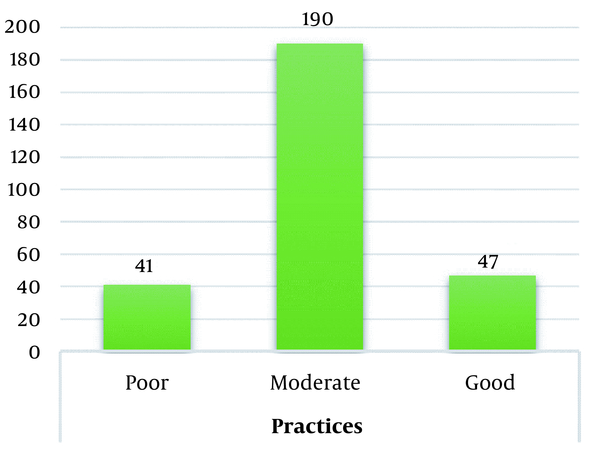
The mean score and standard deviation for the practice items were 29.32 and 10.65, respectively, out of a maximum achievable score of 60. The results indicated that the majority of the SP had a moderate intention towards adopting healthy lifestyle practices and minimizing CVD risk factors. Out of the 278 respondents, 190 (68%) scored between 20 and 40 for the practice items, indicating a moderate intention. Only 47 (16%) achieved a score above 40, indicating a high intention to adhere to a healthy lifestyle. Conversely, 41 (15%) scored below 20, suggesting a very low intention to change. These findings are illustrated in Figure 1.
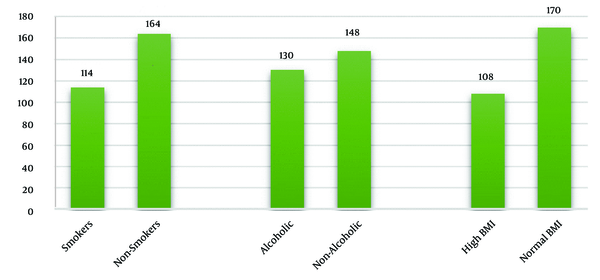
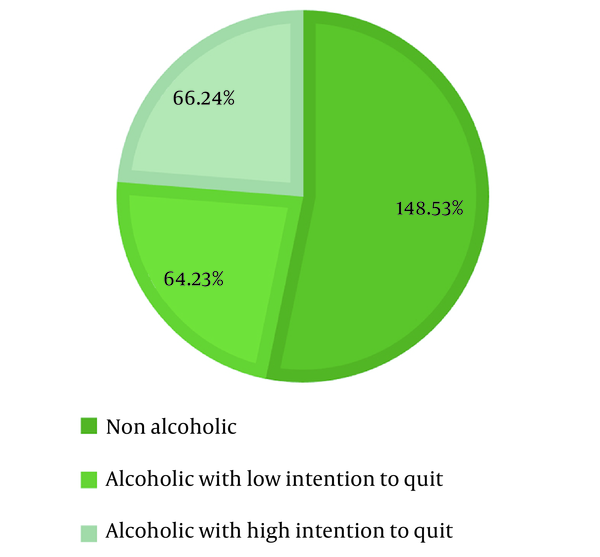
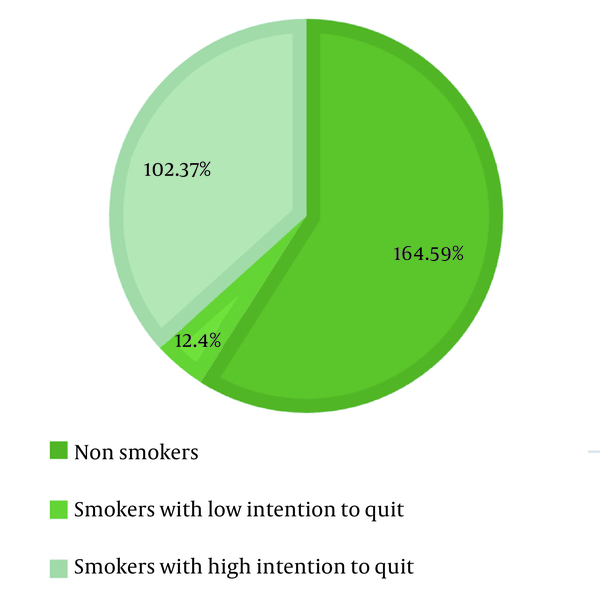
Among the 278 respondents, 114 (41%) were identified as smokers, 130 (46.8%) were found to consume alcohol, and 108 (38.8%) had a high BMI, as depicted in Figure 2. The chi-square test for goodness of fit conducted on BMI indicated that the prevalence of high BMI (39%) among the SP was lower than the prevalence (50%) reported in previous national health surveys.
The chi-square test of independence was used to analyze the differences in the prevalence rates of smoking, alcohol consumption, and high BMI among demographic subgroups in the Kuala Lumpur community. Significant differences were observed among ethnic groups for alcohol consumption (P < 0.005; χ2 = 12.8) and smoking (P < 0.0001; χ2 = 26.63). Malays had the lowest involvement in smoking and alcohol consumption compared to the Chinese and Indian groups. Significant differences in BMI were found based on gender (P < 0.046; χ2 = 0.3.8) and across different age groups (P < 0.000; χ2 = 21.7). However, negligible differences were observed across gender and age groups for smoking and alcohol consumption. Males had higher BMI than females, and older adults had a higher prevalence of overweight and obesity compared to younger age groups. No disparities in BMI were found among ethnic groups.
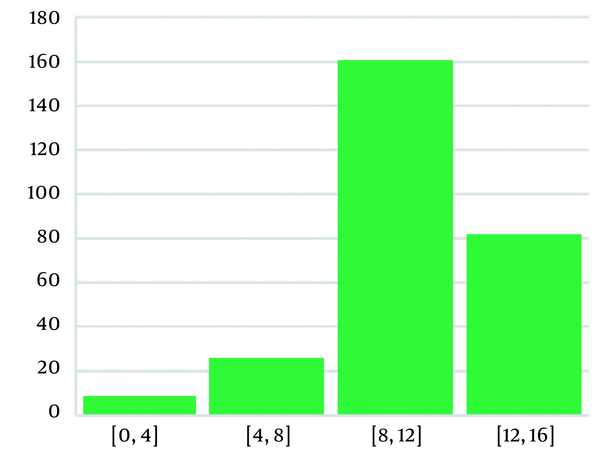
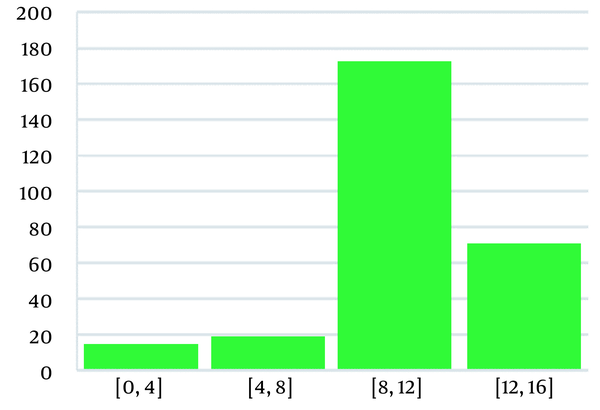
Four domains of lifestyle practices were assessed, including smoking practice and intention to quit smoking, alcohol consumption and intention to reduce and/or quit alcohol, dietary habits and intention to have a balanced WHO-recommended diet, and physical activity and intentions to perform an exercise. The results were formulated individually for each of the dimensions and shown by the graphs in Figures 3, 4, 5 and 6. The intention to practice a particular domain was assessed based on the score achieved. Higher scores indicate a high intention to engage in healthy practices regarding physical activity, healthy diet, smoking, and alcohol consumption.
The majority (90%) of smokers expressed an intention to quit smoking, while only 50% of alcohol consumers agreed to reduce their drinking. Approximately 35% of the survey participants strongly agreed with the WHO-recommended level of physical activity, and 40% strongly agreed with the importance of consuming a healthy diet rich in vegetables and fruits. On the other hand, 60% of the participants had moderate intentions regarding healthy diet and exercise.
4. Discussion
According to the latest Malaysian health and morbidity survey (7), the prevalence of smoking among Malaysian adults is reported to be 20%, while alcohol consumption stands at 11.8%. However, in the current study, these values were found to be significantly higher, potentially due to the demographic characteristics of the surveyed population. The majority of respondents were younger individuals, including university students, and previous research conducted both locally and internationally has indicated a higher prevalence of substance abuse in this age group (11). Notably, there has been a rising incidence of CVD among younger adults aged 20 to 40, with smoking identified as a major risk factor in over two-thirds of cases (12). Smoking has been linked to premature deaths and contributes significantly to disability-adjusted life years in the Malaysian population (13). Both conventional cigarettes and e-cigarettes are commonly used among Malaysian adults, and a substantial portion of the population is exposed to secondhand smoke (7). Previous surveys have reported a higher prevalence of smoking in rural areas compared to urban areas, with Malays exhibiting a higher engagement in smoking practices (14). However, in the current study, smoking was found to be more prevalent among the Chinese and Indian groups. Alcohol consumption is also a growing concern in both Western and Asian countries. Alcohol sales in the Asian region have increased by 176% over the past decade, with the younger population being the most affected (15). Similarly, in the United States, 16.6% of adults consume alcohol, with the age group of 18 - 34 being the most involved (16).The current study found that the prevalence of BMI (39%) among the SP was lower than the prevalence of 50% reported in the latest national health survey (7). The World Health Organization defines overweight and obesity as the abnormal or excessive accumulation of fat that poses health risks. High BMI, including overweight and obesity, has become a widespread issue, and it is crucial to address it due to its strong association with the burden of CVD (17, 18). Malaysia is also experiencing a similar trend of increasing obesity due to urbanization and industrialization. Ahmad et al. compared BMI prevalence rates across all national health surveys in Malaysia. They found a significant association between high BMI and CVD morbidity and mortality among younger adults (19). Dietary practices, such as energy consumption, and physical activity, such as energy expenditure, play a role in determining BMI and are indirectly linked to the risk of hypertension and other cardiovascular events (20, 21). The study examined the variations in the prevalence rates of smoking, alcohol consumption, and high BMI among different demographic subgroups of the Kuala Lumpur community. Significant differences were observed among ethnic groups in terms of alcohol consumption and smoking practices. Malays exhibited the lowest rates of smoking and alcohol consumption compared to other ethnic groups. Regarding BMI, significant differences were found across gender and age groups. However, there were negligible differences across gender and age groups for smoking and alcohol consumption. Males had a higher BMI than females, and older adults were more likely to be affected by overweight and obesity than younger age groups. No significant disparity in BMI was found among ethnic groups. These findings align with local and international research highlighting disparities in health beliefs and health-seeking behaviors among different ethnicities (22, 23). A survey conducted in Nepal also reported variations in smoking, alcohol consumption, and obesity prevalence across ethnicity and gender (24). Similarly, a study in the southeastern region found significant differences across gender in terms of increased BMI, physical activity, tobacco use, binge drinking, and unhealthy diet consumption (25). Various factors contribute to these disparities, including socioeconomic status, stress levels, cultural beliefs and practices, dietary habits, awareness levels, and literacy rates (26).The findings of this research align with other studies conducted in Malaysia and elsewhere on the awareness and practices to prevent CVD by avoiding risk factors (27, 28), while another researcher found good practices related to diet and physical activity among university students (29). Dietary habits play a crucial role in controlling hypertension by reducing sodium intake and managing dyslipidemia/atherosclerosis by avoiding unhealthy and oily foods. These factors strongly influence CVD, making the regulation of diet a prime focus in primary prevention (30). To achieve a healthy body composition, the WHO recommends consuming fruits, vegetables, nuts, animal proteins, and whole grains. Similarly, the American Heart Association advises consuming three or more servings of vegetables daily, which can lower blood cholesterol levels and reduce the risk of atherosclerotic cardiovascular disease by 5% (31, 32).
4.1. Conclusions
Based on the current study, it can be concluded that the lifestyle practices in the Kuala Lumpur community do not align with WHO recommendations. Smoking, alcohol consumption, and increased BMI are significantly prevalent in the community, indicating a lack of healthy dietary practices and adherence to physical activity recommendations. Smoking and alcohol habits vary among ethnic groups, but both genders and all age groups engage in these practices equally. Males and older age groups are more prone to increased BMI, which correlates with a higher burden of CVD risk. Controlling CVD is crucial for improving community health and addressing the high rates of disability and mortality. Nationwide health strategies have been planned to tackle this critical issue. The findings emphasize the need to expand public knowledge about healthy lifestyles and their impact on reducing the potential risk of CVD. It is imperative to improve and raise awareness of lifestyle practices within the Kuala Lumpur community to promote overall health and enhance the quality of life.