1. Background
Cancer incidence and mortality are rapidly increasing worldwide (1). Breast cancer is one of the most common cancers in the world (2) and the first common cancer in women (3, 4) with over 2 million new cases (1 in 4 cancer cases among women) and about 600 000 deaths in 2018 (1). In Iran, breast cancer is also the most common type of cancer in women (5, 6). In addition,14.2% of all cancer deaths in 2012 were due to breast cancer among Iranian women (7); and the breast cancer mortality rate is increasing in Iran (8).
According to a recent study, the 5-year survival of breast cancer is 89.1% and 88.6% in Japan and the USA, respectively (9). But in Africa, Asia, and Central America, the 5-year age-standardized relative survival (ASRS) for breast cancer was from 76% to 82%, in 2010 (10). The survival of breast cancer in England from 2010 to 2011 at 1, 5, and 10 years was reported 96.0%, 86.7%, and 78.5%, respectively (11). In Iran, a meta-analysis study done in 2016 showed that female breast cancer survival at 1, 3, 5, and 10 years was 95%, 80%, 69%, and 55%, respectively (12).
Early detection helps the successful treatment of breast cancer (13, 14). However, several studies conducted in Iran show that women do not have enough knowledge about breast cancer screening and this is one of the reasons for their delay in seeking prompt medical consultation (15, 16). Meanwhile, clinicians need to know about their patient’s prognosis and survival. Among the most important factors related to breast cancer survival is age (17, 18), stage and grade at diagnosis (19, 20), pathologic type of tumor (21), hormonal and human epidermal growth factor receptors (19, 22), tumor size (19), race (22, 23), and secondary metastasis (24). The results of the research indicate that some of the effective factors vary from population to population.
2. Objectives
The present study aimed at investigating the survival of females with breast cancer diagnosed over 14 years and its related factors in Kerman Province.
3. Methods
3.1. Study Population and Data Collection
This is a longitudinal study. Information about females diagnosed with breast cancer was inquired from the Cancer Registry of Kerman University of Medical Sciences from March 2001 to March 2015. Death dates and causes of death were inquired from the Death Registration at Kerman University of Medical Sciences. Other information was collected by contacting the patient or her family.
Variables including age at diagnosis, date of diagnosis, residential location, stage and grade at diagnosis, pathologic type, metastases status, menopausal status, type of treatment, Estrogen and Progesterone hormone receptors status (ER and PR), Human epidermal growth factor receptor 2 (HER2), the existence of other diseases (heart failure, diabetes, and hypertension), and the status of being alive or not were extracted. To calculate survival time (from diagnosis to death), all diagnosed patients during 14 years (from March 2001 to March 2015) were investigated up to the end of 2017 and overall survival was calculated for 1, 3, 5, 10, and 15 years. Hospital medical records were also used to complete the information. Only female patients who lived in Kerman Province were included and alive patients or patients with missing data about their status (dead/alive) were considered censored.
3.2. Statistical Analysis
Kaplan-Meier survival curves were used to calculate the overall survival, and parametric models were used to examine the relationship between the variables and survival. The defaults were checked and the Akaike information criterion (AIC) was used to select the appropriate parametric model from different models such as exponential, log-logistic, Weibull, and Gompertz. The graph ln
4. Results
4.1. Demographic Characteristics
Totally, 2851 women diagnosed with breast cancer in Kerman Province, from March 2001 to March 2015, were enrolled in the present study. The mean and median age of the patients was 49.52 ± 12.87 and 48.00, respectively. More than half of the patients were from urban areas.
Few patients had a history of heart failure (1.9%), diabetes (5.1%), and hypertension (5.8%). More than one-third of the patients were menopause at diagnosis and their mean age of menopause was 47.62 ± 5.08. More than 15% of patients had a positive family history of cancer, 7.9% of whom had a family history of breast cancer and 7.4% had a family history of other cancers (Table 1).
| Variable | No. (%) |
|---|---|
| Age | |
| < 40 | 691 (24.2) |
| 40 - 55 | 1248 (43.8) |
| > 55 | 809 (28.4) |
| Unknown | 103 (3.6) |
| Location | |
| Urban | 1677 (58.8) |
| Rural | 439 (15.4) |
| Unknown | 735 (25.8) |
| Heart failure | |
| Yes | 54 (1.9) |
| No | 1369 (48.0) |
| Unknown | 1428 (50.1) |
| Diabetes | |
| Yes | 144 (5.1) |
| No | 1274 (44.7) |
| Unknown | 1433 (50.3) |
| Hypertension | |
| Yes | 156 (5.8) |
| No | 1258 (44.1) |
| Unknown | 1428 (50.1) |
| Menopause status | |
| Pre-menopause | 967 (33.9) |
| Post-menopause | 530 (18.6) |
| Unknown | 1353 (47.5) |
| Family history of cancer | |
| Yes | 435 (15.3) |
| No | 541 (19.0) |
| Unknown | 1921 (67.4) |
| Family history of breast cancer | |
| Yes | 225 (7.9) |
| No | 694 (24.3) |
| Unknown | 1932 (67.8) |
| Year of diagnosis | |
| 2001 - 2004 | 428 (15.0) |
| 2005 - 2007 | 603 (21.2) |
| 2008 - 2010 | 686 (24.1) |
| 2011 - 2014 | 1064 (37.3) |
| Unknown | 70 (2.4) |
| Place of residence | |
| Kerman | 1412 (49.5) |
| Others | 1099 (38.5) |
| Unknown | 340 (12.0) |
In the present study, most patients were diagnosed at stage II (19.9%) and grade II (31.3%) and the common pathologic type was invasive ductal carcinoma (70.9%). Patients received surgical treatment (41.7%), chemotherapy (43.2%), radiotherapy (26.7%), and hormone therapy (28.8%), and among patients who had surgery, modified radical mastectomy (33.8%) was the most common type. Some patients were positive for hormonal receptors of estrogen (25.7%), progesterone (23.9%), and epidermal human growth factor (26%); and 6.6% of patients had secondary metastasis at diagnosis (Table 2).
| Variable | No. (%) |
|---|---|
| Grade at diagnosis | |
| I | 290 (10.2) |
| II | 893 (31.3) |
| III | 402 (14.1) |
| Unknown | 1266 (44.4) |
| Stage at diagnosis | |
| 0 | 15 (0.5) |
| I | 135 (4.7) |
| II | 567 (19.8) |
| III | 395 (17.0) |
| IV | 89 (3.1) |
| Unknown | 1651 (57.9) |
| Pathologic type | |
| Invasive ductal | 2022 (70.9) |
| Others | 674 (23.8) |
| Unknown | 155 (5.3) |
| Chemotherapy | |
| Yes | 1231 (43.2) |
| No | 30 (1.1) |
| Unknown | 1590 (55.8) |
| Hormonotherapy | |
| Yes | 821 (26.7) |
| No | 391 (13.7) |
| Unknown | 1639 (58.6) |
| Radiotherapy | |
| Yes | 762 (26.7) |
| No | 419 (14.7) |
| Unknown | 1670 (58.6) |
| Herceptin therapy | |
| Yes | 133 (4.7) |
| No | 1059 (37.1) |
| Unknown | 1659 (58.2) |
| Surgery | |
| None | 55 (1.9) |
| BCT | 226 (7.9) |
| MRM | 963 (33.8) |
| Unknown | 1607 (56.4) |
| Estrogen receptor status | |
| Positive | 734 (25.7) |
| Negative | 506 (17.7) |
| Unknown | 1611 (56.5) |
| Progesterone receptor status | |
| Positive | 681 (23.9) |
| Negative | 491 (17.2) |
| Unknown | 1679 (58.9) |
| Status of human epidermal growth factor receptor 2 | |
| Positive | 742 (26.0) |
| Negative | 457 (16.0) |
| Unknown | 1652 (57.9) |
Abbreviations: BCT, breast conventional therapy; MRM, modified radical mastectomy.
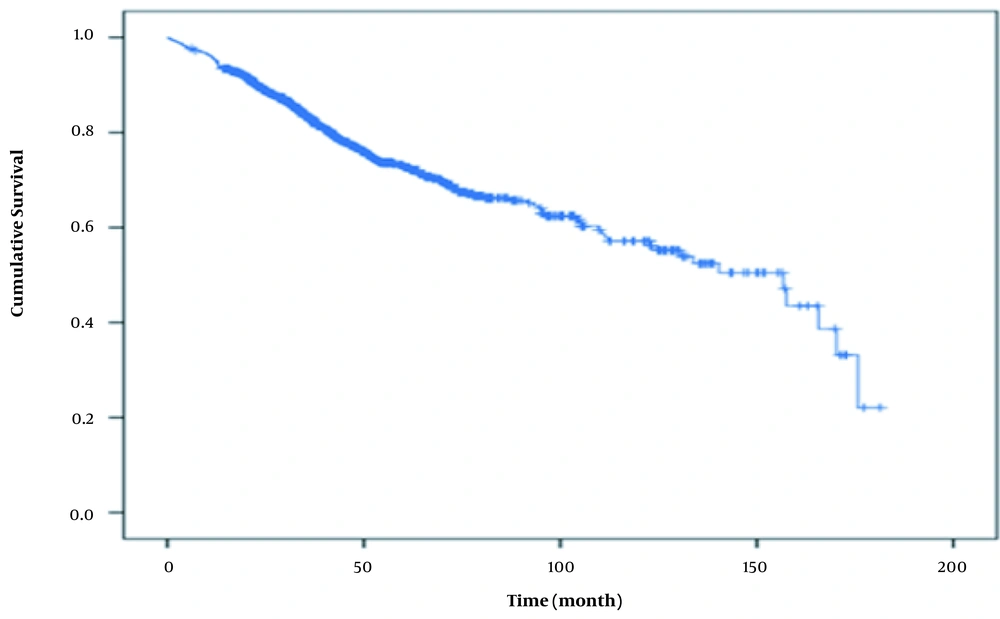
4.2. Survival Analysis
The median survival time was 157 months. The overall survival of patients after 1, 3, 5, 10 and 15 years was 0.95 (CI 95% = 0.93 - 0.96), 0.83 (CI 95% = 0.80 - 0.85), 0.73 (CI 95% = 0.69 - 0.76), 0.57 (CI 95% = 0.51 - 0.62), and 0.25 (CI 95% = 0.06 - 0.44), respectively (Figure 1).
Unadjusted survival analysis was performed and the AIC of the log-logistic method was lower than other methods and, therefore, the log-logistic method was a better fit (Table 3). In addition, the plots were parallel straight lines and, hence, the log-logistic PO and AFT assumptions were reasonable.
| Model | LL (Model) | df | AIC | BIC |
|---|---|---|---|---|
| Exponential | -192.0823 | 3 | 714.7506 | 728.7553 |
| Weibull | -184.3718 | 7 | 382.7436 | 412.5607 |
| Log-logistic | -132.241 | 10 | 284.482 | 325.5966 |
| Gompertz | -188.6736 | 7 | 391.3471 | 421.1642 |
Abbreviations: AIC, Akaike information criterion; BIC, Bayesian information criterion; df, degrees of freedom; LL, log-likelihood of the full model
A total of 1109 patients had complete data for diagnosis date and status of being alive or not; 239 of all patients had complete data for all variables, including diagnosis date, status, age, year of diagnosis, stage, grade, the status of chemotherapy, hormonotherapy, radiotherapy, surgery, HER2, ER, PR, location, city, family history of cancer, family history of breast cancer, the status of secondary metastasis, the status of chronic diseases (heart failure, blood pressure, and diabetes), and menopause status.
The results of unadjusted and adjusted parametric regression analysis with the log-logistic distribution showed stage and grade at diagnosis, hormone therapy, metastasis, and menopause status had a significant relation with the survival of females with breast cancer in Kerman Province from March 2001 to March 2015 (Table 4).
| Variable | Time Ratio | CI 95% | Crude P-Value | Time Ratio | CI 95% | Adjusted P-Value |
|---|---|---|---|---|---|---|
| Location | 0.330 | - | ||||
| Urban | 1 | - | - | - | - | |
| Rural | 1.05 | 0.75 - 1.47 | - | - | ||
| Age | ||||||
| < 40 | 1 | - | - | 1 | - | - |
| 40 - 55 | 1.17 | 0.86 - 1.61 | 0.298 | 0.01 | 0.32 - 1.80 | 0.575 |
| > 55 | 0.65 | 0.47 - 0.89 | 0.008 | 0.47 | 0.76 - 3.38 | 0.216 |
| Grade at diagnosis | ||||||
| I | 1 | - | - | 1 | - | - |
| II | 0.80 | 0.54 - 1.18 | 0.268 | 0.82 | 0.50 - 1.36 | 0.450 |
| III | 0.53 | 0.34 - 0.83 | 0.005 | 0.51 | 0.29 - 0.88 | 0.016 |
| Stage at diagnosis | ||||||
| 0 and I | 1 | - | - | 1 | - | - |
| II | 0.68 | 0.30 - 1.50 | 0.341 | 0.95 | 0.40 - 2.20 | 0.901 |
| III | 0.29 | 0.13 - 0.65 | 0.003 | 0.63 | 0.28 - 1.44 | 0.281 |
| IV | 0.09 | 0.04 - 0.22 | < 0.001 | 0.11 | 0.04 - 0.29 | < 0.001 |
| Chemotherapy | 0.832 | - | ||||
| No | 1 | - | - | - | ||
| Yes | 1.10 | 0.41 - 2.97 | - | - | ||
| Radiotherapy | 0.820 | - | ||||
| No | 1 | - | - | - | ||
| Yes | 1.03 | 0.75 - 1.41 | - | - | ||
| Hormonotherapy | 0.008 | 0.013 | ||||
| No | 1 | - | 1 | - | ||
| Yes | 1.50 | 1.10 - 2.05 | 1.52 | 1.09 - 2.13 | ||
| Herceptin therapy | 0.074 | 0.176 | ||||
| No | 1 | - | 1 | - | ||
| Yes | 0.67 | 0.43 - 1.03 | 1.61 | 0.81 - 3.28 | ||
| Secondary metastasis | < 0.001 | < 0.001 | ||||
| No | 1 | - | 1 | - | ||
| Yes | 0.29 | 0.19 - 0.42 | 0.22 | 0.13 - 0.34 | ||
| Surgery | ||||||
| BCT | 1 | - | - | 1 | - | - |
| MRM | 0.71 | 0.44 - 1.17 | 0.186 | 0.99 | 0.58 - 1.64 | 0.947 |
| No | 0.21 | 0.10 - 0.44 | < 0.001 | 0.59 | 0.27 - 1.28 | 0.188 |
| ER status | 0.148 | 0.805 | ||||
| Negative | 1 | - | 1 | - | ||
| Positive | 1.25 | 0.92 - 1.73 | 1.09 | 0.51 - 2.36 | ||
| PR status | 0.002 | 0.795 | ||||
| Negative | 1 | - | 1 | - | ||
| Positive | 1.66 | 1.19 - 2.29 | 0.93 | 0.51 - 1.66 | ||
| HER2 status | 0.424 | - | ||||
| Negative | 1 | - | - | - | ||
| Positive | 0.86 | 0.61 - 1.22 | - | - | 0.887 | |
| Diabetes | 0.090 | |||||
| No | 1 | - | 1 | - | ||
| Yes | 1.64 | 0.93 - 2.97 | 0.74 | 0.30 - 1.80 | ||
| Heart failure | 0.949 | - | ||||
| No | 1 | - | - | - | ||
| Yes | 0.98 | 0.41 - 2.29 | - | - | ||
| Hypertension | 0.004 | 0.509 | ||||
| No | 1 | - | 1 | - | ||
| Yes | 5.64 | 1.75 - 18.17 | 0.74 | 0.30 - 1.80 | ||
| Family history of cancer | 0.424 | - | ||||
| No | 1 | - | - | - | ||
| Yes | 0.77 | 0.40 - 1.46 | - | - | ||
| Family history of breast cancer | 0.354 | - | ||||
| No | 1 | - | - | - | ||
| Yes | 1.49 | 0.63 - 3.52 | - | - | ||
| Menopause status | 0.173 | 0.014 | ||||
| Pre-menopause | 1 | - | 1 | - | ||
| Post-menopause | 0.79 | 0.57 - 1.10 | 0.65 | 0.46 - 0.92 | ||
| Pathologic type of tumor | < 0.001 | 0.369 | ||||
| Ductal | 1 | - | 1 | - | ||
| Others | 0.51 | 0.37 - 0.70 | 0.70 | 0.32 - 1.50 | ||
| Year of diagnosis | ||||||
| 2001 - 2004 | 1 | - | - | 1 | - | - |
| 2005 - 2007 | 1.75 | 1.01 - 3.12 | 0.055 | 0.45 | 0.69 - 3.59 | 0.280 |
| 2008 - 2010 | 0.90 | 0.55 - 1.46 | 0.671 | 0.48 | 0.72 - 3.63 | 0.238 |
| 2011 - 2014 | 0.10 | 0.69 - 1.78 | 0.678 | 0.95 | 0.44 - 1.99 | 0.883 |
| Place of residence | 0.012 | 0.235 | ||||
| Kerman | 1 | - | 1 | - | ||
| Others | 0.71 | 0.54 - 0.93 | 0.79 | 0.53 - 1.16 |
The median survival time among patients with grade 3 at diagnosis was 0.51 of patients with grade 1 (P = 0.016). The median survival time among patients with stage 4 at diagnosis was 0.11 of patients with stages 0 and 1 (P < 0.001). The median survival time among post-menopause patients at diagnosis was 0.65 of pre-menopause patients (P = 0.014). The median survival time among patients with secondary metastasis was 0.22 of patients without secondary metastasis (P < 0.001) and the median survival time among patients with hormone therapy was 1.52 of patients without this treatment (P = 0.013).
5. Discussion
In the present study, the mean and median survival time of patients was 119 and 157 months. Karimi et al. (24) in Kurdistan, Iran investigated 313 females with breast cancer from 2006 to 2014, and showed that their median survival time was 81 months; and the median survival time in Abdullah et al.’s study (25) conducted on 10 230 Malaysian females with breast cancer diagnosed from 2001 to 2005 was 68.1 months. The higher median survival time in the present study in comparison with studies of Karimi et al. (24) and Abdullah et al. (25) may be due to population differences.
In the present study, survival after 1, 5, 10, and 15 years was 95%, 73%, 57%, and 25%, respectively. Movahedi et al. (26) investigated 6 147 patients with breast cancer from 2001 to 2006 in Tehran and showed that their 5-year survival time was 71% (26). Meanwhile, in Payandeh et al.’s study (4), 3-, 5-, and 10-year survival rates for 950 Kurdish women with invasive ductal carcinoma and triple-negative breast cancer from 2001 to 2014 in Iran were 82%, 72%, and 64%, respectively (4). The 5- and 10-year survival rate of patients in the present study was longer than the Kermanshah study and similar to the study done in Tehran. However, the length of follow-up and the number and type of variables in these studies were less and different from the present study.
Abdullah et al.’s study (25) from Malaysia showed that the 5-year survival rate for 10 230 patients with breast cancer diagnosed from 2001 to 2005 was 49%. Meanwhile, in Park et al.’s study (27) in Korea, the 5-year survival rate was 89.8% for 294 patients with breast cancer diagnosed at stages I and II from 2000 to 2005. Also, in England from 2010 to 2011, the 1-, 5-, and 10-year survival rate of females with breast cancer was 96.0%, 86.7%, and 78.5%, respectively (11), which shows a higher rate of breast cancer survival in developed countries.
In the present study, the median survival time among patients with grade 3 and stage 4 at diagnosis was significantly lower than patients with grade 1 and stages 0 and 1, respectively. The results of a study by Yaghmaei et al. (28) from Semnan showed that the survival of patients with breast cancer with stages 1 and 2 at diagnosis was similar, but for patients with stages, 3 and 4 at diagnosis was lower. Moghadami Fard et al. (29) showed, grade at diagnosis is a risk factor and can influence the disease-free survival of patients with breast cancer.
In the present study, the median survival time among patients with secondary metastasis was significantly lower than patients without it. Cetin et al. (30) in Denmark investigated 2427 females with breast cancer with bone metastasis and showed the time from breast cancer diagnosis to bone metastasis diagnosis and stage at diagnosis were important prognostic factors for the survival of these patients. In addition, Rahimzadeh et al. (31) in Tehran, Iran showed metastasis affects disease-free survival of patients with breast cancer and was a critical factor for cure rates in these patients. Also, the results of a study done by Kalantari Khandani et al. (32) in Kerman, Iran about metastasis and its related factors showed stage at diagnosis and residential location of patients with breast cancer were related to secondary metastasis, which can affect the treatment and survival of these patients.
In the present study, the median survival time among patients with hormonotherapy was significantly more than patients without this treatment. Atashgar et al.’s study (33) investigated 499 patients with breast cancer in Iran from 2010 to 2015 and showed that patients with hormone therapy had a much lower risk of death than patients, who did not receive this treatment.
There was no significant relationship between residential location and survival of patients in the present study. However, a systematic review showed that the survival of females with breast cancer from non-metropolitan areas was less than others (34).
In the present study, there was no relationship between survival and age, tumor size at diagnosis, and the pathologic type of tumor. Vostakolaei et al. (35) also showed that after adjusting for stage, grade, the status of estrogen and progesterone receptors, and residential location, the mortality risk of breast cancer was similar in different groups; and young and old women had the same mortality risk, which is similar to the present study.
Although Kalantari-Khandani et al. (36) showed that the triple-positive (ER+, PR+, and HER2+) was more frequent among females with breast cancer in Kerman, Iran, in the present study, there was no significant relationship between the status of estrogen and progesterone receptors and HER2 with the survival of patients. However, Kongsiang et al. (37) investigated 272 patients with breast cancer with radiotherapy from 1999 to 2014 in Thailand and showed that the 5-year survival rate was lowest among HER2-enriched females. In addition, Ibrahim et al.’s study on 868 patients in Malaysia from 2005 to 2009 showed that the ER+/PR+ female patients had a significantly higher survival rate than ER-/PR- and the patients with HER2+ had a significantly lower survival rate than HER2- (38).
In this study, after about 15 years, about a quarter of patients were alive. Stage and grade at diagnosis and secondary metastasis were factors influencing the survival of patients. Therefore, early diagnosis and proper treatment can improve patients’ survival. Periodic examinations especially in menopause ages are recommended. Hormonotherapy improved survival significantly.
An important limitation of this study was its missing data and difficulty in data collection.