1. Introduction
Germ cell tumors (GCTs) are rare neoplasms comprising about 3.5% of all pediatric tumors in children younger than 15 years of age; They most commonly arise in testes and ovaries, however, 1 - 5% of all GCTs occur in extragonadal sites and 4% of extragonadal GCTs are recognized in the retroperitoneum (1-3) .
There are very rare cases of the primary retroperitoneal tumor with spinal column invasion and cord compression and most of these cases are observed in children (4, 5).
In this article, a primarily retroperitoneal yolk sac tumors (YST) in a 19-month-old boy with spinal cord compression was presented.
2. Case Presentation
A 20-month-old boy referred to the hospital with limping and irritability which have been progressed over the earlier 10 days. The child had a normal developmental history and was fully immunized.
There was no history of cryptorchidism (Undescended testes), radiation therapy, and hormone therapy.
Clinical examination yielded no significant findings including mass or organomegaly. Blood pressure was within normal range based on age and sex. Cranial nerve testing provided normal results on neurological examination, a paraparesis with 3/5 of normal motor strength and hyperactive deep tendon reflexes were noticed in left lower limb no sensory disorder was distinguished.
Laboratory data showed white blood cell (WBC) 5.3 × 103/uL, hemoglobin 10.4 g/dL, platelet 323 × 103/uL, neutrophils 61%, lymphocytes 31%, monocytes 7%, Eosinophils 1%, erythrocyte sedimentation rate (ESR) 9 mm/h, C-reactive protein (CRP) 9 mg/L, and lactate dehydrogenase (LDH) 470 U/L. Urine analysis was unremarkable.
Abdominal ultrasonography showed a 52 × 50 mm solid mass surrounded the inferomedial margin of the left kidney suggesting neuroblastoma.
We considered neuroblastoma, Wilms tumor, and germ cell tumor as the most common differential diagnosis for this abdominal mass in the patient.
Based on differential diagnosis, serum tumor markers were studied. The patient’s serum alpha-fetoprotein was elevated (> 500 ng/mL; normal range up to 10 ng/mL) but beta-human chorionic gonadotropin (beta-HCG) and urine vanillylmandelic acid (VMA) were normal.
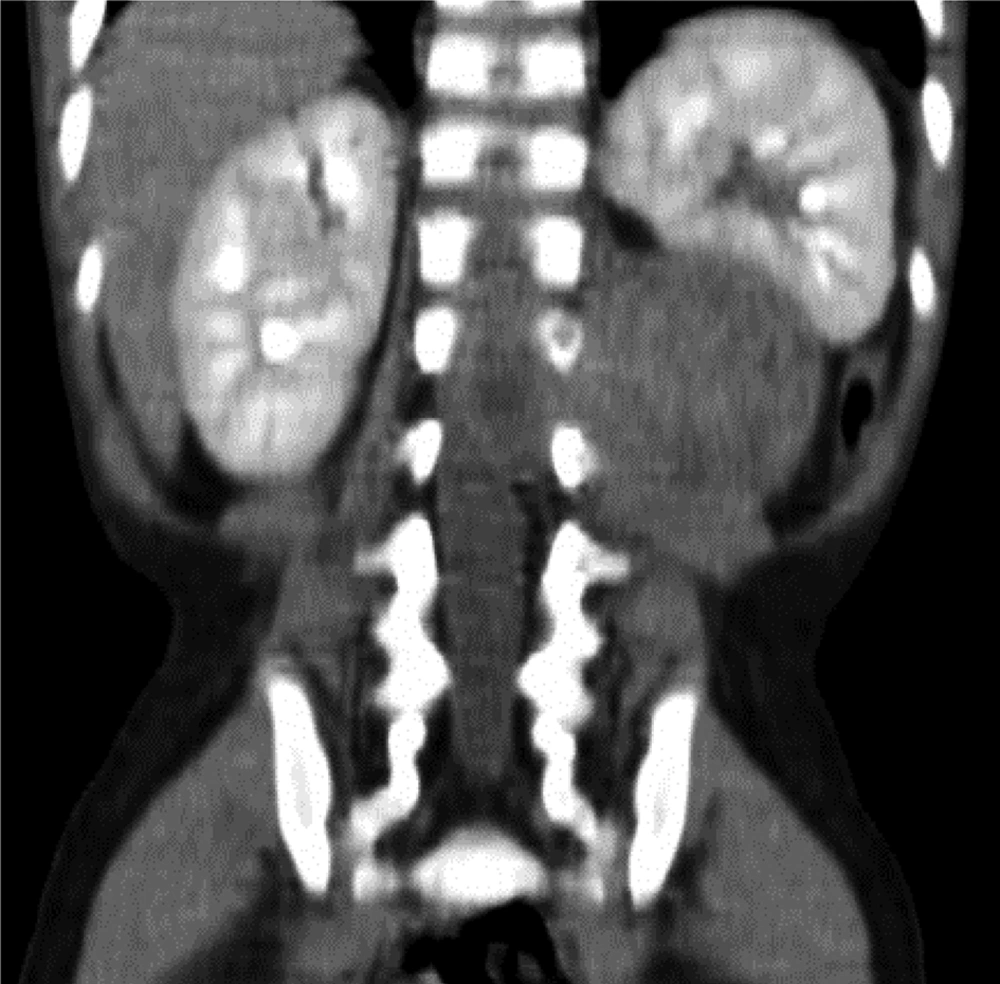
Abdominopelvic computed tomography scan (CT-scan) showed a well-defined lesion with internal heterogeneity. This tumor was also compressing the left kidney and it was extended into the spinal column with spinal cord compression from T12 to L3 (Figure 1). Brain and chest CT-scan revealed no abnormal findings.
The mass was an extra-renal tumor. According to normal urine metanephrines and elevated level of alpha-fetoprotein, germ cell tumor were considered as the main differential diagnosis.
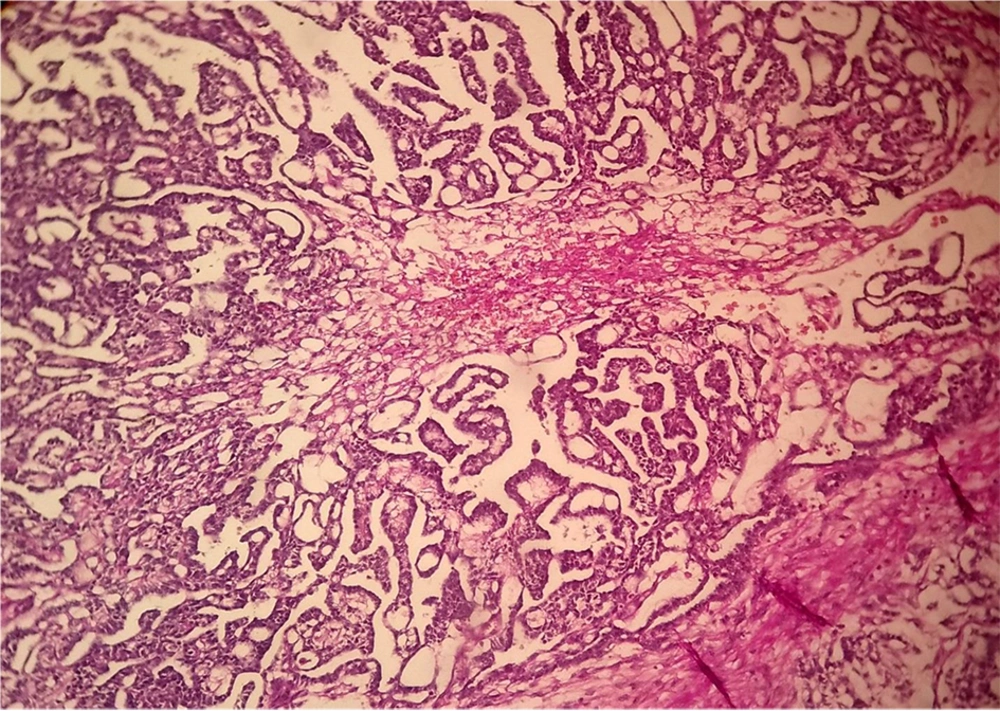
A wide surgical excisional biopsy was performed and pathological examination showed tumor cells arranged in pseudo glandular and trabecular structures and microcystic reticular pattern in favor of YST (Figure 2); subsequent immunohistochemistry (IHC) staining was positive for pan-CK and Alpha- fetoprotein and negative for PLAP, CD 117 and CD30.
Base on surgery report and imaging studies, the patient categorized as stage III and chemotherapy regimen consisting of bleomycin (15 units/m2 day 3), etoposide (120 mg/m2 /IV days 1 to 3), and carboplatin (600 mg/m2 /IV day 1) was initiated for the patient. Due to the young age of the patient and more complications of cisplatin (including ototoxicity and nephrotoxicity) we preferred to use carboplatin (JEB regimen). The treatment was administered every 3 weeks, for 4 cycles followed by surgery. After 2 cycles of chemotherapy, abdominal sonography was done and there was no obvious mass on the tumor location.
Four months later, at the end of chemotherapy, the patient’s serum alpha-fetoprotein level was found within normal limits (5.13 ng/mL) and subsequent magnetic resonance imaging (MRI) imaging did not show any pathologic findings (Figure 3).
The patient has been followed up for 2 years and so far there is no evidence of tumor recurrence.
Written informed consent was obtained from the patients’ parents for publication of this case report.
3. Discussion
Germ cell tumors constitute a group of benign and malignant tumors with histopathologic heterogeneity and account for approximately 2% to 3% of pediatric malignancies. (6, 7).
YST is the most common histologic subtype of GCTs in young children; testis and ovary are the most common sites of involvement in children older than 2 years old and adolescents (5).
In rare cases, these tumors may develop in extragonadal locations, including mediastinum, intracranium, retroperitoneum, uterine, and sacrococcygeal region (8).
It has been claimed that extragonadal GCTs originate from primordial germ cells, which their migration has been arrested during embryogenesis (5).
The most common pathologic pattern seen in YST tumor is microcystic structure, which is characterized by the presence of a spider-web like network shaped by vacuolated cytoplasm of tumor cells. In addition to Alpha- fetoprotein, the main tumor marker for YST, Cytokeratin is present in almost all the cases, and vimentin and placental alkaline phosphatase (PLAP) can be positive in several different subtypes of germ cell tumors (5, 9).
There are many reports of primary retroperitoneal YST, but 2 cases of primary YST with spinal cord compression that have been reported in the previous studies are more similar to our patient. One case was reported by Guzel et al. and involved a 31-year-old male patient with primary paraspinal YST. He presented with back pain and gait difficulty. A chemotherapy regimen consisting of bleomycin, etoposide, and cisplatin was started. However, the patient died due to sepsis (as a side effect of the chemotherapy?) despite antibiotic therapy(4) . The second case described a 21-month-old boy with a complaint of back pain that was eventually found to be as a result of primary paraspinal YST. Although vincristine, actinomycin- D, and cyclophosphamide were prescribed as medication, the patient died for no reason (8).
In the presented case, the location and behavioral characteristics of the lesion suggested a diagnosis of neuroblastoma. However, elevated levels of beta-HCG and alfa-FP indicated a tumor with germ cell origin.
Both abdominal computed tomography scan (CT-scan) and lumbar magnetic resonance imaging (MRI) are the preferred radiological examinations in the diagnosis of these types of tumors (4). Histologic examination of the surgical specimen confirmed the definitive diagnosis of YST. Since no other lesions were found, the primary tumor appeared to be responsible for symptoms.
The treatment of OGCTs in the progressive tumor generally includes debulking surgery of tumors followed by adjuvant chemotherapy (5, 9). Before the introduction of novel therapeutic regimens in the 1970s, YST was a poor-prognosis malignancy but implementing Platinum-based chemotherapy elevates the 5-year survival rate up to 90% (5, 7). Currently, a multidrug chemotherapy regimen comprising bleomycin, etoposide, and cisplatin or carboplatin are used as the first-line treatment option and have remarkably increased the prolonged survival of patients (9).
To evaluate the effectiveness of treatment, serum alfa-FP levels should be assessed before each chemotherapy cycle, at the end of treatment, and up to 2 years after the end of treatment (10).
3.1. Conclusions
Our case highlights that primary YSTs may have unusual presentations and should be considered as a differential diagnosis of pediatric abdominal mass. Variation in the histological and behavioral features of the yolk sac tumor and its overlap with other somatic tumors make diagnosis a challenge for physicians. Although YST is an uncommon malignancy, it can be cured. As a result, it would be crucial to differentiate YST from other somatic tumors which tend to imitate its behavioral characteristics.