1. Introduction
Rhabdomyosarcoma (RMS) is a malignancy of skeletal muscle that can occur everywhere in the body (1). Renal tumors comprise a diverse spectrum of neoplastic lesions with patterns that are relatively distinct for children and adults. Tubular epithelium is the most common site, which is involved with various types of benign and malignant tumors (2). RMS rarely occurs in adults and sarcomas of the kidney are rare soft tissue tumors seen in approximately 1% of all primary renal malignancies in adults (3). Accurate diagnosis of most renal tumors is not possible before surgery and histopathologic evaluation. Moreover, currently the gold standard in the treatment of renal tumors is radical or partial nephrectomy. Genitourinary tract rhabdomyosarcoma occurs most commonly in the urinary bladder, prostate, vagina, and uterus as para-testicular disease. Here, we report a case of adult primary renal RMS in a young woman.
2. Case Presentation
A 33-year-old female patient with a history of total gross hematuria for 1 month was referred to Shohada-e-Tajrish hospital. She had a computerized tomography (CT) that showed a heterogeneous solid mass of 5 × 3 cm, protruding from the left renal pelvis. Upper ureter showed some expansions.
Physical examination revealed a mild left flank pain. There was no mass in abdominal examination, no lymphadenopathy, and no other abnormality in her examination. Urinary analysis demonstrated many red blood cells (RBCs) in each high power field; other laboratory examinations were normal. The patient had no history of surgery or medical illness. After admission, abdominal magnetic resonance imaging (MRI) showed a well-defined soft-tissue mass in the left renal pelvis, which was poorly enhanced following contrast medium administration, caused hydronephrosis, and delayed gadolinium excretion of the left kidney. The mass was confined to the left renal pelvis without the evidence of abdominal lymphadenopathy. The primary diagnosis was transitional cell carcinoma and the patient underwent left ureteroscopy (URS) and cold cup biopsy of pelvis mass. In histopathologic examination, superficial transitional mucosa infiltrated by mixed inflammatory cells with necrosis was reported, but no viable neoplastic tissue was observed.
We performed left radical nephrectomy and ureterectomy with cuff cystectomy, based on the pathology report and documented recurrent gross hematuria and patient’s imaging due to the common diagnosis of urothelial carcinoma of the renal pelvis.
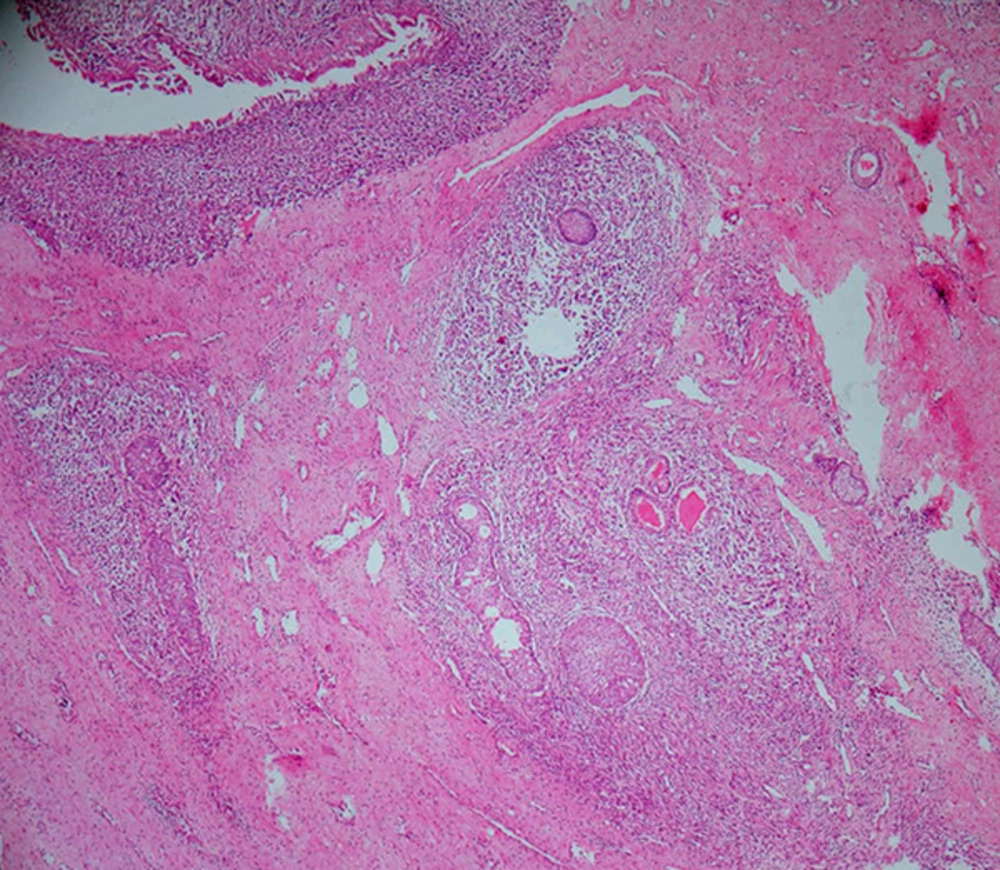
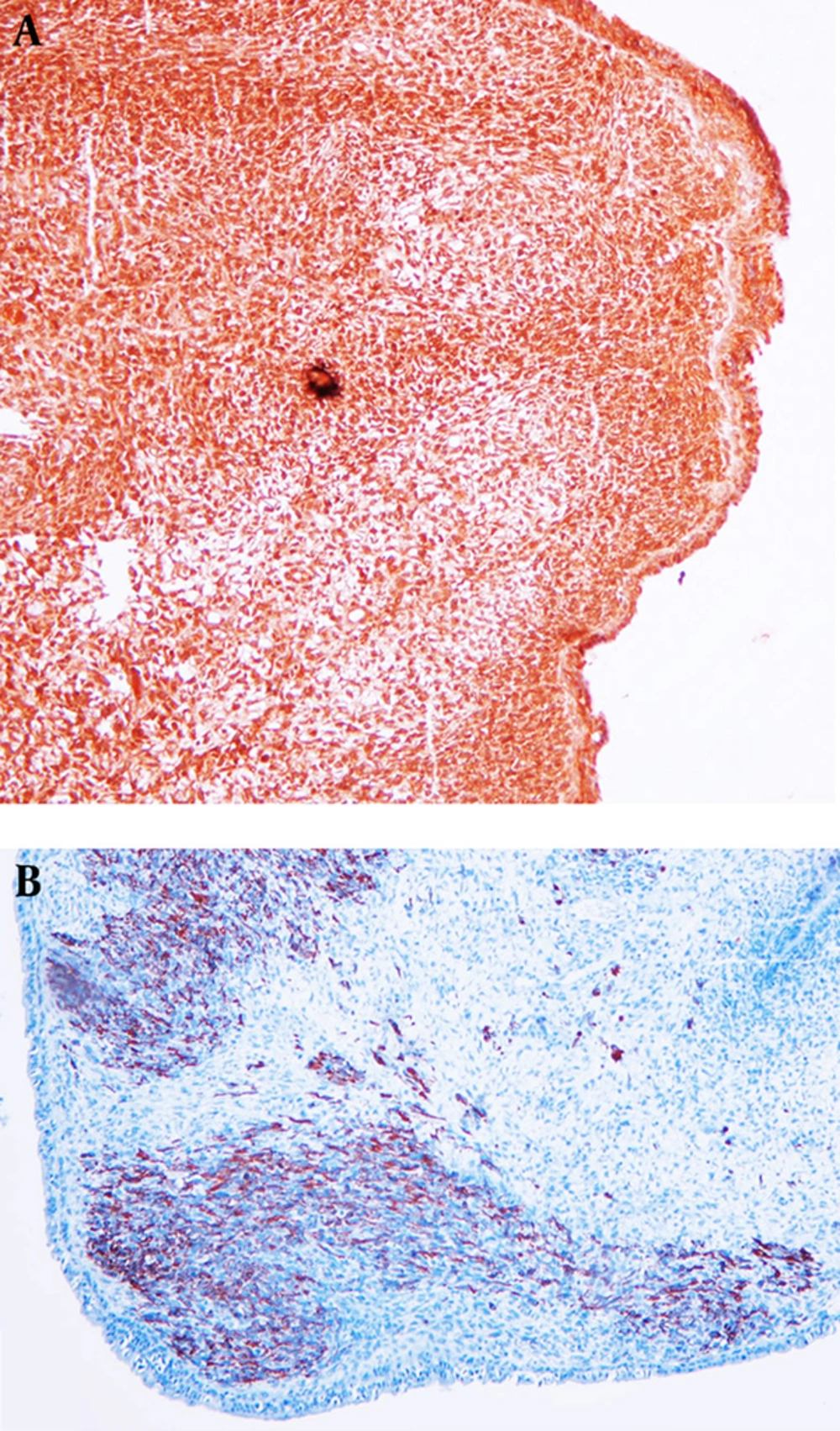
Grossly, the pyelocaliceal system was dilated and there were 2 fleshy pedunculated polypoid masses; one of them was in the left renal pelvis (1.5 × 0.5 × 0.2 cm) and the other one was in upper renal calyx (2 × 1.5 × 1 cm). In microscopic examination, there was a hyper-cellular zone of condensed round to spindle cells with scant cytoplasm and frequent mitoses immediately beneath the atrophic urothelium, known as Nicholson's cambium layer (Figure 1) and a less cellular zone with some differentiating cells in deeper layers. The diagnosis of botryoid type embryonal rhabdomyosarcoma was made. There was an exaggerated von Brunn’s nests hyperplasia, which could be mistaken as urothelial carcinoma, but the bland cytology of these nests made the distinction possible. In immunohistochemistry (IHC) study, the tumor cells were positive for MyoD1 (diffuse), Desmin, and SMA (patchy) and negative for CKAE1/AE3, CK34BE12, EMA, S-100, and WT-1 (Figure 2). The masses had no invasion to obvious renal parenchyma, renal sinus, or renal vein and were completely confined to the kidney.
Post-operatively, the patient showed an unremarkable recovery and was scheduled to begin combination chemotherapy as an outpatient. Ten months after her original diagnosis, she was alive with no evidence of metastatic disease.
2.1. Ethical Considerations
The present research is involved with human participant, who signed the informed consent; the authors did not disclose her personal information.
3. Discussion
RMS is a malignant aggressive soft tissue tumor, which is derived from mesenchymal cells, already committed to become skeletal muscle cells (4). RMS is a common tumor in pediatrics, but not in adults (1). According to the new world health organization (WHO) classification, RMS is divided into 4 groups: Embryonal rhabdomyosarcoma, alveolar rhabdomyosarcoma, pleomorphic rhabdomyosarcoma, and spindle cell/sclerosing rhabdomyosarcoma. Botryoid RMS is a variant of embryonal RMS, considering its grape-like macroscopic appearance. The frequent sub-type with nearly 66% incidence is embryonal (ERMS) with the best prognosis (5). RMS in adults initiated from the large skeletal muscles, while the lower extremity is the most frequent site, followed by the trunk (6). Most RMS tumors express high levels of early inducers of muscle differentiation, such as MyoD1 and myogenin.
The diagnosis of primary renal sarcoma in specific RMS is very difficult, both clinically and radiographically. Imaging characteristics of most sarcomas are indistinguishable from renal cell carcinoma. In our case, although we performed CT, URS, and MRI, we finally found the correct diagnosis after radical nephrectomy.
Renal RMS in adults is extremely rare, while in the literature, only 11 cases were reported (5, 7). The evaluations of the present study showed that she had fulfilled the criteria. She did not have a history of sarcoma elsewhere, and metastatic disease was excluded. Imaging results confirmed our premise, and the pathologic results verified the origin of the tumor site in renal parenchyma and no invasion from outside the kidney. Final evaluation after surgical nephrectomy in microscopic examination also excluded a sarcomatoid renal cell carcinoma.
Fang et al. (1) presented a similar case with flank pain, gross hematuria, and complain of nausea and vomiting. Fanous et al. (8) reported a different manifestation, a 37-year-old woman with a progressive 6-month history of lethargy, weight loss, right flank pain, and hematuria. Gurel et al. (9) also reported a 50-year-old woman with a large rhabdomyosarcoma of the left kidney and associated adrenal cortical adenoma. Meir et al. (7) described the case of a 39-year-old woman with a large rhabdomyosarcoma of the left kidney serendipitously discovered with ultrasound evaluations. The majority of cases in the literature were female, similar to our case, which should be considered for more evaluation.
Here, we reported a rare case of primary RMS of the kidney in an adult woman. We performed a radical nephrectomy as an effective therapeutic option for localized renal disease; adjuvant chemotherapy may reduce the risk of recurrence. While many suggest treatment as per pediatric protocols, there is growing evidence that the progression and prognosis of adult disease is unlike pediatric disease. Although the prognosis of adult renal RMS is generally very poor, we reported the survival of our patient after treatment in the follow ups. For better evaluation and treatment of future cases, further studies are required.