1. Introduction
A Wolffian tumor is a rare type of tumor that is presumed to originate in mesonephric remnants. It was originally described by Karminejad and Scully in 1973 as FATWO (1, 2). Reproductive organs, including the broad ligament, mesosalpinx fallopian tubes, ovaries, and peritoneum originate from the mesonephric system (Wolffian duct) (2).
FATWO occurs more commonly in the broad ligament as a benign lesion, and it should be considered as a low-grade malignancy. Recurrence and metastasis of FATWO have been reported (2, 3).
Because of the rarity of this tumor, there is no recommendation about its management and treatment. We reported a rare case of FATWO in the broad ligament / paratubal with infiltration of tumor cells at the seromuscular layer of the fallopian tube.
2. Case Presentation
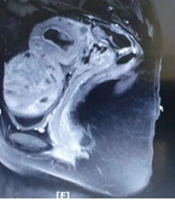
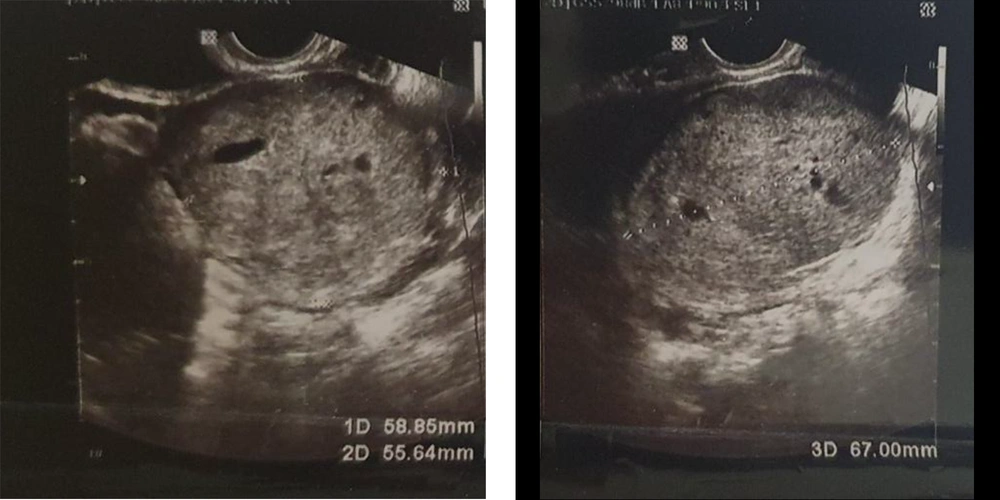
A 32-year-old woman, gravida 4, live 1, and abortion 3 was diagnosed with left ovarian mass and endometrial polyp after evaluation for vaginal discharge by sonography. Her previous gynecological history included a normal vaginal delivery and three spontaneous abortions. In the vaginal examination, there was fullness in the left adnexa, separated from the uterine, mobile, and without tenderness. Transvaginal ultrasound revealed a normal size uterus and echogenic solid mass with dimensions of 14×6 mm in the endometrial cavity, which could be due to endometrial polyp and a well-defined highly echogenic solid mass with a diameter of 60×60 mm adjacent to the left ovary with normal size ovaries (Figure 1). Magnetic resonance imaging (MRI) confirmed this mass. A T1-weighted fat saturation contrast-enhanced MRI showed a 65×65 mm, well-defined mass with heterogeneous enhancement in the left broad ligament that was attached to the lower part of the left ovary (Figure 2). The chest X-ray was unremarkable. Serum tumor markers were Ca125:26 u/mL, CA19-9: 7 u/mL, and CEA: 0.5 ng/mL.
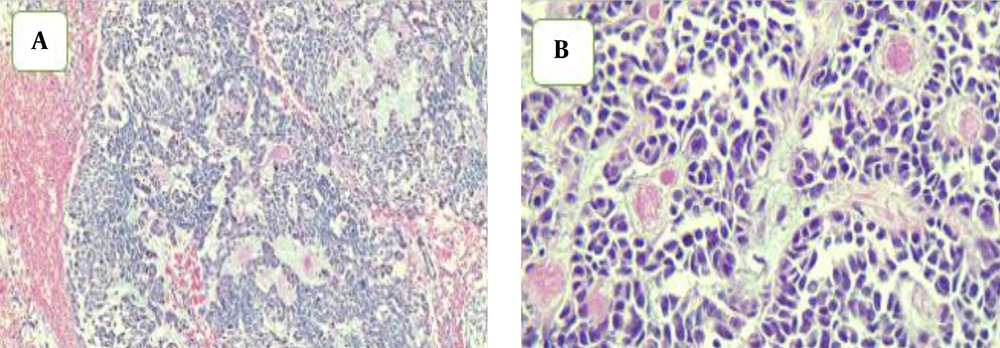
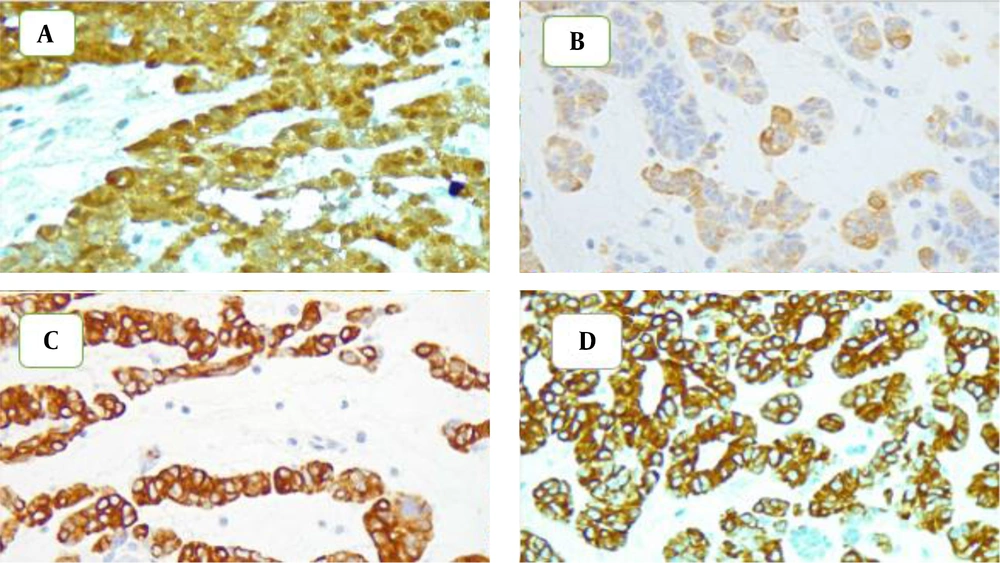
First, to exclude endometrial pathology, the patient underwent hysteroscopy curettage and polyp resection with the histopathologic finding being endometrial polyp with secretory changes. After this evaluation, laparotomy was intraoperatively performed, and two fleshy well-defined solid masse with the size of 10×10 cm and 2×3 cm were found in the left paratubal, broad ligament, distinct from the left ovary and near the left fallopian tube (Figures 3 and 4). There were no macroscopic intra-abdominal lesions. Both masses were removed and examined with a frozen section, and Sertoli cell tumors were considered. However, due to the location of the tumor in the broad ligament and the normal ovary, the Wolffian duct tumor was more probable. Therefore, only left salpingectomy and mass resection were performed, and the patient was discharged without any complication. Grossly, this mass was 10×8×4 cm, and cut sections showed a solid homogeneous friable surface with small cysts; however, the small mass was 3×3×2 cm resembling a large mass. Microscopically, the small mass had sieve-like and tubulocystic appearances with intraluminal bright eosinophilic secretions and necrosis. Mitosis count was 5 per 10 high power fields in hot spot areas. Infiltration of tumor cells existed at the serosal surface and muscular layer of the left fallopian tube near this mass. Immunohistochemically, the tumor cells were positive for calretinin, inhibin, vimentin, CD56, WT1, and cytokeratins (CK) 7 and 19, but negative for epithelial membrane antigen (EMA), CD10, AFP, and Glypican-3. FATWO was confirmed based on this pathologic finding. Twenty months after conservative surgery, evidence of recurrence was not observed during close follow-up by sonography. It should be noted that informed consent was obtained from the patient for this report.
3. Discussion
FATWO originates in mesonephric remnants and presents as an expansible homogeneous tumor suspended in the broad ligament (2).
Some adnexal tumors are close to the ovary, and this is the reason why this type of tumor is reported as ovarian masses (4). FATWO is an uncommon tumor presented at different ages with different ranges of size (5, 6). Patients with large FATWO may present with abdominal pain, but many patients remain asymptomatic and are diagnosed incidentally (3, 4). Microscopically, FATWO exhibits different features from solid with spindled cells to various degrees of tubule formation and cystic structures (2, 3). Diagnosing FATWO was supported by the immunohistochemical profile, and staining should be positive for calretinin, CK7, CK8, CK10, and vimentin, but negative for EMA, the carcinoembryonic antigen (CEA), and CK20 (2, 7, 8). Molecular alterations in FATWO are still unclear (3). There are no specific serum biomarkers for this tumor. Moreover, there are no specific radiologic findings in the Wolffian duct tumor. A computed tomography scan is more accurate than ultrasound in determining the tumor origin, and it is heterogeneously enhanced in CTS (3, 7).
Due to cystic denegation in the Wolffian duct tumor and since it is slightly hyperintense, it is difficult to differentiate between subserosal myoma and the thecomas with FATWO in MRI (9). This tumor has benign behavior, but some recurrent and metastatic cases have been reported (10). It is reported that the size above 10 cm, necrosis, capsular invasion, a high number of mitosis, positive staining for CD117, and overexpression of ki-67 are correlated with malignant behavior (4, 11). Therefore, FATWO should be considered as a low-grade malignancy, and the patient should be closely monitored after tumor resection (2). Pathologically, the Wolffian duct tumor has some differential diagnoses, such as systolic Leydig cell tumor, endometriosis carcinoma of the fallopian tube, clear cell carcinoma, and granulosa cell tumor (2, 12, 13). Immunohistochemistry may help exclude these tumors from FATWO. Negative EMA is an advantage in epithelial neoplasms, and positive CD10 staining is helpful to sex cord-stromal tumors. Moreover, FATWO is extra tubal, whereas FATWO-like tumors are intramural masses (8, 14). However, it is difficult to differentiate FATWO from these tumors and we should pay attention to all the characteristics of these tumors. In our patient, due to the lack of androgenic symptoms, location of the tumor on the base of the paratubal, broad ligament, extraluminal infiltration of the fallopian tube, and pathologic and immunohistochemical findings, the Wolffian duct tumor was recommended. We performed conservative surgery due to a frozen section pathology report. The patient was disease-free after a 20-month follow-up. Patients who were treated with tumor resection alone have the most recurrent FATWO within two years (15). In the pathology of our patient, there was an infiltration of tumor cells in the sermuscular layer of the left fallopian tube; it is an invasive feature that should be considered by clinicians. FATWO is a low-grade malignancy, and patients should be closely monitored after its removal (2).
3.1. Conclusions
Although FATWO has benign behavior, it may have malignant features, and there is no clear recommendation regarding its optimal treatment and surveillance. Therefore, based on the literature, pathologists are recommended to utilize a wide array of immunohistochemical stainings to help appropriately diagnose the disease. Therefore, optimal surgery is performed, and patients should be followed up for a long-term period until we have enough knowledge in the field.