1. Background
Cancer is a leading cause of death and the most important barrier to increasing life expectancy in the world in the 21st century (1). The cancer burden rises to 18.1 million new cases and 9.6 million deaths in 2018. It is estimated that cancer would be the first cause of death in 2060 (18.63 million deaths) (2).
Colorectal cancer (CRC) is the third most frequent cancer (1.80 million cases) as well as the second most frequent malignancy in women (0.79 million cases) and the third most frequent in men (0.98 million cases), respectively (2-4).
This cancer is also the third common cancer in men (16.57) and the second in women (11.86) in Iran. The incidence rate of CRC is higher in central parts of Iran due to urbanization and unhealthy lifestyle (5-7). CRC is a multi-factorial disease with wide global patterns and is strongly linked to human development index level, reflecting the adoption of western lifestyles that accompany economic transition and elevate risk. Although the absolute risk of CRC in adults younger than 50 years is low relative to older adults, disease trends in young age groups are a key indicator of recent changes in risk factor exposures and often foreshadow the future cancer burden (3, 8, 9). In general, the incidence of CRC is rising in low-income and middle-income countries but beginning to stabilize or decline in high-income countries, especially those that have implemented screening (10). Regional reports from Iran showed increasing trends in the incidence of CRCs (11, 12). Besides, some studies have shown changes in the epidemiology and morphology trends of the cancers in some countries and Iran (13).
The epidemiology trend of CRC from 2003 to 2008 was reported based on the national cancer registry system in Iran; colon, rectal, rectosigmoid, and anal cancers were diagnosed in 61.83 %, 27.54 %, 7.46 %, and 3.10%, respectively (13). The trend of CRC in young Iranians is rising (14). The annual percentage changes (APC) in age-standardized incidence rate (ASR) increased in both sexes from 2003 to 2008 (8). The 5-year prevalence of CRC in females aged between 55 and 59 years old and males aged older than 75 years was estimated 2.03 times for 2020 than of 2015 (15). Tehran had the highest ASR (20.58 per 100 000 person-years) of CRC in comparison to other Iran provinces (16). Since Tehran is the largest city in Iran with a population of 13 267 637 million (2016 census) and the majority of the population of Tehran consists of immigrants from the different ethnic groups of Iran and diverse socioeconomic status, it is fairly proportional to the total population of each ethnic group in the country. However, the incidence rates and trends are essential to planning because no comprehensive study has been done in the Tehran metropolis for CRC.
2. Objectives
This study aimed at reporting a 10-years (2006 - 2015) trend in epidemiology and morphology of CRC in Tehran metropolis, using the data of the National Cancer Registry.
3. Methods
There are three medical universities in Tehran: Tehran, Iran, and Shahid Beheshti University of Medical Sciences. There is a Secretariat of Cancer Registry in each university that is responsible for the registration of cases with cancer in the area covered by the university. Information of patients with cancer are gathered from regional hospitals, charities, laboratories, and death registration units separately by cancer registry experts and uploaded on Integrated Information Management System of Cancer and after integration of information from three universities, subsequent data processing is applied on the integrated data.
3.1. Data Collection
To ensure the comparability of data, we used a national guideline. This guideline is developed by the National Secretariat of Cancer Registry based on standard protocols and administration programs of international references. According to this guideline, the data of patients with primary tumors were obtained from their primary registration form, which consisted of two sections: mandatory and optional information. Of patients’ residential region is a mandatory item that allows us to determine the precise geographical distribution of disease.
The data were obtained from 3 main sources: pathology reports from pathology centers, clinical/preclinical information, and death certificates. Death certificates are gathered from the Main Death Registration Center of Tehran University of Medical Sciences and also regional statistics of cities covered by three universities.
We tried to precisely classify patients by the method they have been recognized. Some cases with cancer have not been diagnosed or recorded in their lifetime and the method of their recognition is death certificate only (DCO). To find DCO cases, we linked available incidence and death information according to patients’ National Identification codes (ID). To find DCO cases without recorded ID, name, surname, gender, and father’s name were used. Data of cancer registry in each center were collected as electronic files or on paper (according to available resources) and, then, were integrated as Excel files in SECRETARIATS and these files were uploaded on cancer profile system (samaneye-simaye-saratan) after corrections.
Iranian Health Ministry has developed a special population-based national program for communication of cancer data named cancer profile system (samaneye-simaye-saratan). A unique username and password are dedicated to each medical university to access its dashboard on this system. Data can be uploaded as a form (personal information) or as a panel (for classified data such as Excel forms) on the system.
Classification and coding of tumors were based on international standards. We used the 3rd edition of the international classification of diseases for oncology (ICD-O) for coding tumors, which is based on tumor characteristics (topography, morphology, behavior, and grade of tumor).
3.2. Data Processing and Quality Control
Data processing and quality control were conducted by the administrator of the secretariat and included recognition of duplications by searching names, matching morphology and topography of tumors, matching tumor type with patient’s sex, matching death and incidence rates, and control of internal validity of data. During date processing and quality control, problematic records were detected by the administrator of quality control at the level of province and these records were sent back to regional experts of the cancer registry for corrections/revisions. After revision/correction of data and quality assurance, the data were analyzed.
3.3. Statistical Analysis
Descriptive statistics including frequency (mean age ± standard deviation (SD) of age) were used to summarize the cancer distribution in each topography code such as cecum, appendix, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon sigmoid colon, overlapping sites of the colon, rectosigmoid, rectum and colon unspecified during 2006 to 2010 and 2011 to 2015. The frequency ratio and mean age difference in the second period (2011-2015) compared to the first period (2006 - 2010) were described in each male and female. ASRs were calculated, using the direct standardization method and the new world health organization (WHO) standard population in 2001 per 100 000 person-years for each sex, year, topography types, and morphology groups from 2006 to 2015 (17). Also, the 95% confidence interval (CI) was obtained for all ASRs based on the direct method (18). The standardized rate ratio (SRR) and the 95% CI was calculated to represent the relative risk of incidence from 2011 to 2015 compared to 2006 to 2010 and male compared to female using the Smith method (19). The average annual percentage change (AAPC) with one joinpoint was presented for males and females in patients with age < 50 and age ≥ 50 years (20). All analyses were performed, using IBM SPSS, version 26 and Joinpoint 4.7.0.0 and the P-value less than 0.05 was considered significant. The Ethics Committee of Shahid Beheshti University of Medical Sciences approved this study.
4. Results
Demographic and tumor characteristics of CRC diagnosed from March 20, 2006, to March 20, 2015, in Tehran metropolis (the capital city of Iran) were expressed and summarized in Table 1. Out of 1 6280 enrolled patients with CRC, 9 257 (56.86%) cases were male and 7 023 (43.14%) were female. Through male and female patients, 5 768 (63.38%) and 4 340 (61.80%) were diagnosed in the second 5 years (2011 - 2015) of the study period, respectively (Table 1).
| Topography | Frequency (Mean Age ± Standard Deviation of Age) | Comparison Between 2011 - 2015 and 2006 - 2010 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2006 - 2010 | 2011-2015 | Ratio of Frequency (Mean Differences of Age) | |||||||
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| Cecum | 214 (61.04 ± 14.07) | 121 (61.05 ± 13.90) | 93 (61.02 ± 14.36) | 726 (61.91 ± 14.41) | 417 (61.72 ± 15.43) | 309 (62.18 ± 12.93) | 3.39 (0.88) | 3.45 (0.67) | 3.32 (1.16) |
| Appendix | 34 (50.88 ± 20.43) | 15 (52.40 ± 18.81) | 19 (49.68 ± 22.05) | 65 (44.20 ± 19.11) | 25 (41.24 ± 21.39) | 40 (46.05 ± 17.58) | 1.91 (-6.68) | 1.67 (-11.16) | 2.11 (-3.63) |
| Ascending colon | 212 (60.16 ± 13.58) | 123 (60.75 ± 13.16) | 89 (59.34 ± 14.17) | 626 (61.78 ± 14.49) | 368 (61.73 ± 15.16) | 258 (61.84 ± 13.49) | 2.95 (1.62) | 2.99 (0.99) | 2.90 (2.50) |
| Hepatic flexure | 52 (61.04 ± 13.26) | 27 (61.74 ± 12.98) | 25 (60.28 ± 13.79) | 160 (62.41 ± 14.72) | 98 (61.05 ± 14.61) | 62 (64.55 ± 14.74) | 3.08 (1.37) | 3.63 (-0.69) | 2.48 (4.27) |
| Transverse colon | 153 (57.54 ± 14.16) | 86 (57.20 ± 14.49) | 67 (57.99 ± 13.82) | 327 (61.40 ± 15.01) | 206 (61.11 ± 15.33) | 121 (61.89 ± 14.51) | 2.14 (3.86a) | 2.40 (3.91a) | 1.81 (3.91) |
| Splenic flexure | 84 (59.96 ± 14.30) | 48 (62.44 ± 12.12) | 36 (56.67 ± 16.38) | 121 (62.61 ± 14.34) | 60 (61.92 ± 15.29) | 61 (63.30 ± 13.45) | 1.44 (2.65) | 1.25 (-0.52) | 1.69 (6.63a) |
| Descending colon | 182 (60.34 ± 14.03) | 97 (61.49 ± 13.59) | 85 (59.01 ± 14.48) | 412 (62.04 ± 14.44) | 226 (63.14 ± 15.06) | 186 (60.71 ± 13.58) | 2.26 (1.71) | 2.33 (1.65) | 2.19 (1.70) |
| Sigmoid colon | 1017 (62.04 ± 13.44) | 574 (63.66 ± 12.99) | 443 (59.95 ± 13.73) | 1790 (62.17 ± 13.97) | 958 (62.82 ± 14.22) | 832 (61.42 ± 13.64) | 1.76 (0.13) | 1.67 (-0.83) | 1.88 (1.47) |
| Overlapping sites of colon | 45 (62.22 ± 11.72) | 24 (60.17 ± 12.09) | 21 (64.57 ± 11.11) | 48 (59.23 ± 14.59) | 27 (59.30 ± 13.85) | 21 (59.14 ± 15.84) | 1.07 (-2.99) | 1.13 (-0.87) | 1.00 (-5.43) |
| Colon, unspecified | 2017 (60.18 ± 14.55) | 1139 (60.90 ± 14.68) | 878 (59.24 ± 14.34) | 2511 (62.98 ± 14.94) | 1385 (63.57 ± 15.17) | 1126 (62.26 ± 14.61) | 1.24 (2.80a) | 1.22 (2.67a) | 1.28 (3.01)a |
| Rectosigmoid | 612 (60.04 ± 14.06) | 338 (61.38 ± 13.39) | 274 (58.38 ± 14.70) | 839 (60.41 ± 14.24) | 502 (62.05 ± 14.43) | 337 (57.96 ± 13.61) | 1.37 (0.37) | 1.49 (0.66) | 1.23 (-0.41) |
| Rectum | 1550 (59.57 ± 14.92) | 897 (60.57 ± 14.96) | 653 (58.18 ± 14.75) | 2483 (60.10 ± 14.92) | 1496 (61.04 ± 14.80) | 987 (58.67 ± 15.00) | 1.60 (0.54) | 1.67 (0.47) | 1.51 (0.50) |
| Total | 6172 (60.25 ± 14.39) | 3489 (61.23 ± 14.26) | 2683 (58.99 ± 14.46) | 10108 (61.52 ± 14.75) | 5768 (62.13 ± 14.98) | 4340 (60.73 ± 14.39) | 1.64 (1.27) | 1.65 (0.90) | 1.62 (1.74) |
a The difference in mean age between 2011 and 2015 and 2006 and 2010 with level of significance < 0.05
According to the results, there were 12 topography categories with total malignant frequency (mean age) of 6 172 (60.25 years) from 2006 to 2010 and 10 108 (61.52 years) from 2011 to 2015. Among all topographies, the unspecified colon, rectum, and sigmoid colon had the 3 highest frequencies of CRC with the values of 2017, 1 550, and 1 017 cases from 2006 to 2010 and 2 511, 2 438, and 1 790 cases from 2011 to 2015, respectively. Besides, the mean age of the mentioned categories were 60.18/62.98, 59.57/60.10, and 62.04/62.17 years in 2006-2010/2011-2015, respectively. The malignant neoplasm of overlapping sites of the colon was the rarest type of CRC topography with 45 new cases from 2006 to 2010 and 48 new cases from 2011 to 2015. Although the total mean age in the transverse colon and unspecified colon were significantly higher from 2011 to 2015 compared to 2005 to 2010, other topography categories did not have significantly different mean ages in these two periods (Table 1).
In the next step, we calculated the ASR (95% CI) of Adenocarcinoma and other morphology types for each of the years of 2006 to 2015 among males and females. The result showed that the ASR of adenocarcinoma and other morphology types was higher in males than females for all 10 years. The highest and lowest overall ASR (95% CI) were reported in 2013 and 2006 with the value of 22.46 (95% CI: 21.58-23.35) and 5.55 (95% CI: 5.04 - 6.07) per 100 000 person-years, respectively. Among Adenocarcinoma, the total ASR was 14.67 (95% CI: 14.44 - 14.91) per 100 000 person-years, while other morphology types had the ASR of 0.91 (95% CI: 0.85 - 0.97) per 100 000 person-years. The estimated AAPC indicates that from 2006 to 2015, the overall ASR had a statistically upward trend with the value of 15.0 (95% CI: 1.80 - 30.00) in total CRC patients. Also, the AAPC of adenocarcinoma type in males and females was 15.6 (95% CI: 1.10 - 32.20) and 12.9 (95% CI: 0.60-26.60) over the study period, respectively, which showed a significant upward trend (Table 2).
| Years | ASR (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Adenocarcinoma | Others | Total | |||||||
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| 2006 | 5.36 (4.86-5.87) | 5.67 (4.93-6.40) | 5.03 (4.34-5.73) | 0.19 (0.10-0.28) | 0.23 (0.11-0.36) | 0.14 (0.01-0.26) | 5.55 (5.04-6.07) | 5.90 (5.16-6.64) | 5.17 (4.47-5.88) |
| 2007 | 8.35 (7.74-8.96) | 9.01 (8.11-9.91) | 7.69 (6.86-8.52) | 0.26 (0.15-0.37) | 0.27 (0.12-0.42) | 0.24 (0.09-0.39) | 8.61 (7.99-9.23) | 9.28 (8.37-10.19) | 7.93 (7.09-8.78) |
| 2008 | 17.29 (16.44-18.14) | 20.00 (18.70-21.29) | 14.56 (13.46-15.66) | 0.75 (0.58-0.93) | 0.94 (0.67-1.22) | 0.56 (0.35-0.78) | 18.04 (17.18-18.91) | 20.94 (19.61-22.27) | 15.12 (14.00-16.24) |
| 2009 | 15.09 (14.31-15.87) | 16.58 (15.41-17.74) | 13.61 (12.57-14.66) | 0.74 (0.57-0.91) | 0.95 (0.68-1.21) | 0.53 (0.33-0.73) | 15.83 (15.03-16.63) | 17.52 (16.33-18.72) | 14.14 (13.07-15.21) |
| 2010 | 14.40 (13.65-15.14) | 16.90 (15.74-18.06) | 11.91 (10.95-12.86) | 0.79 (0.62-0.96) | 0.88 (0.63-1.14) | 0.69 (0.47-0.92) | 15.18 (14.41-15.95) | 17.79 (16.60-18.97) | 12.60 (11.62-13.58) |
| 2011 | 12.21 (11.53-12.89) | 14.22 (13.17-15.28) | 10.25 (9.38-11.13) | 0.64 (0.49-0.80) | 0.80 (0.55-1.04) | 0.48 (0.29-0.68) | 12.85 (12.15-13.55) | 15.02 (13.94-16.10) | 10.74 (9.84-11.63) |
| 2012 | 14.80 (14.07-15.54) | 16.33 (15.23-17.43) | 13.33 (12.35-14.31) | 0.72 (0.56-0.88) | 0.76 (0.53-1.00) | 0.69 (0.47-0.91) | 15.53 (14.77-16.28) | 17.09 (15.97-18.22) | 14.02 (13.02-15.02) |
| 2013 | 21.19 (20.33-22.06) | 24.98 (23.65-26.32) | 17.44 (16.34-18.54) | 1.27 (1.06-1.48) | 1.38 (1.08-1.69) | 1.15 (0.87-1.44) | 22.46 (21.58-23.35) | 26.37 (25.00-27.74) | 18.60 (17.46-19.73) |
| 2014 | 19.98 (19.16-20.80) | 23.92 (22.64-25.20) | 16.09 (15.05-17.12) | 1.75 (1.51-1.99) | 2.00 (1.64-2.36) | 1.50 (1.19-1.81) | 21.73 (20.87-22.59) | 25.91 (24.59-27.24) | 17.59 (16.51-18.67) |
| 2015 | 15.44 (14.73-16.15) | 17.34 (16.27-18.41) | 13.57 (12.63-14.50) | 1.62 (1.40-1.85) | 1.80 (1.46-2.14) | 1.45 (1.14-1.75) | 17.07 (16.32-17.81) | 19.14 (18.02-20.26) | 15.02 (14.03-16.00) |
| Total | 14.67 (14.44-14.91) | 16.76 (16.41-17.12) | 12.58 (12.28-12.89) | 0.91 (0.85-0.97) | 1.04 (0.95-1.12) | 0.78 (0.70-0.86) | 15.58 (15.34-15.83) | 17.80 (17.43-18.17) | 13.36 (13.05-13.68) |
| AAPC | 14.4 (1.10-29.4) | 15.6 (1.10-32.20) | 12.9 (0.60-26.60) | 23.7 (13.50-34.70) | 22.6 (11.40-34.90) | 25.8 (16.30-36.00) | 15.0 (1.80-30.00) | 16.2 (1.80-32.60) | 13.7 (13.30-27.50) |
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
In a more complete table, we summarized ASR by sex, morphology type, topography type, and study period. According to the results, among male adenocarcinoma cases, the 3 highest ASRs from 2006 to 2010 were for unspecified colon, rectum, and sigmoid colon with the values of 4.42, 3.46, and 2.38 per 100 000 person-years, respectively. However, rectum, unspecified colon, and sigmoid were the 3 highest ASRs from 2011 to 2015 with values of 4.79, 4.72, and 3.41 per 100 000, respectively. Among females adenocarcinoma, the 3 highest ASRs were observed in the unspecified colon, rectum, and sigmoid from 2006 to 2010 (with the values of 3.44, 2.57, and 1.82 per 100 000, respectively) and 2011 to 2015 (with the values of 3.74, 2.92, and 2.88 per 100 000, respectively). In other morphology types, no ASR above 0.6 per 100 000 person-years was reported in males and females, which indicates a rare incidence for this group in the current study (Table 3).
| C Group | Frequency | 2006 - 2010 | 2011 - 2015 | SRR (2006 -2010 to 2011 - 2015) | 2006 - 2015 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | 95% CI | SRR | ||||||||||
| Both | Male | Female | Both | Male | Female | Both | Male | Female | Both | Male | Female | M to F | ||
| M Group: Adenocarcinoma | ||||||||||||||
| Cecum | 863 | 0.42 (0.36-0.49) | 0.47 (0.38-0.56) | 0.38 (0.30-0.46) | 1.19 (1.10-1.28) | 1.38 (1.24-1.52) | 1.01 (0.89-1.13) | 2.80 (2.42-3.25) | 2.91 (2.40-3.55) | 2.67 (2.14-3.35) | 0.84 (0.78-0.90) | 0.95 (0.87-1.04) | 0.72 (0.65-0.80) | 1.32 (1.15-1.51) |
| Appendix | 59 | 0.05 (0.03-0.07) | 0.04 (0.01-0.07) | 0.05 (0.02-0.08) | 0.06 (0.04-0.08) | 0.05 (0.02-0.07) | 0.08 (0.05-0.11) | 1.32 (0.78-2.24) | 1.15 (0.49-2.70) | 1.44 (0.73-2.84) | 0.05 (0.04-0.07) | 0.04 (0.02-0.06) | 0.07 (0.04-0.09) | 0.65 (0.38-1.10) |
| Ascending colon | 807 | 0.43 (0.37-0.49) | 0.50 (0.41-0.59) | 0.36 (0.28-0.44) | 1.08 (0.99-1.17) | 1.27 (1.14-1.41) | 0.89 (0.78-1.00) | 2.51 (2.16-2.92) | 2.55 (2.09-3.10) | 2.47 (1.96-3.12) | 0.78 (0.73-0.84) | 0.91 (0.83-1.00) | 0.65 (0.58-0.72) | 1.41 (1.22-1.62) |
| Hepatic flexure | 201 | 0.10 (0.07-0.13) | 0.10 (0.06-0.14) | 0.10 (0.06-0.14) | 0.28 (0.23-0.32) | 0.34 (0.27-0.41) | 0.21 (0.16-0.27) | 2.71 (2.00-3.68) | 3.31 (2.19-4.99) | 2.11 (1.34-3.34) | 0.19 (0.17-0.22) | 0.23 (0.18-0.27) | 0.16 (0.13-0.20) | 1.37 (1.03-1.82) |
| Transverse colon | 467 | 0.29 (0.24 -0.34) | 0.32 (0.25 -0.39) | 0.26 (0.20-0.33) | 0.57 (0.50-0.63) | 0.72 (0.62-0.82) | 0.42 (0.34-0.49) | 1.95 (1.61-2.36) | 2.27 (1.77-2.92) | 1.59 (1.18-2.15) | 0.44 (0.40-0.48) | 0.53 (0.47-0.60) | 0.35 (0.29-0.40) | 1.55 (1.28-1.87) |
| Splenic flexure | 198 | 0.17 (0.13 -0.21) | 0.19 (0.14 -0.25) | 0.14 (0.09 -0.19) | 0.21 (0.17 -0.25) | 0.20 (0.15 -0.26) | 0.22 (0.16-0.27) | 1.26 (0.95-1.68) | 1.07 (0.72-1.58) | 1.53 (1.01-2.32) | 0.19 (0.16-0.22) | 0.20 (0.16-0.24) | 0.18 (0.15-0.22) | 1.07 (0.81-1.42) |
| Descending colon | 577 | 0.38 (0.33-0.44) | 0.41 (0.32-0.49) | 0.36 (0.28-0.44) | 0.71 (0.64-0.78) | 0.78 (0.67-0.88) | 0.64 (0.55-0.73) | 1.85 (1.56-2.19) | 1.90 (1.50-2.41) | 1.78 (1.39-2.29) | 0.56 (0.51-0.60) | 0.60 (0.53-0.67) | 0.51 (0.45-0.57) | 1.18 (1.00-1.39) |
| Sigmoid colon | 2731 | 2.10 (1.97-2.24) | 2.38 (2.18-2.59) | 1.82 (1.64-2.00) | 3.14 (2.99-3.29) | 3.41 (3.19-3.63) | 2.88 (2.68-3.08) | 1.50 (1.38-1.62) | 1.43 (1.29-1.59) | 1.58 (1.41-1.78) | 2.66 (2.56-2.76) | 2.92 (2.77-3.07) | 2.40 (2.27-2.54) | 1.22 (1.13-1.31) |
| Overlapping sites of colon | 89 | 0.10 (0.07-0.13) | 0.10 (0.06-0.14) | 0.10 (0.05-0.14) | 0.08 (0.05-0.10) | 0.09 (0.05-0.12) | 0.07 (0.04-0.10) | 0.79 (0.51-1.21) | 0.85 (0.47-1.51) | 0.72 (0.38-1.36) | 0.09 (0.07-0.10) | 0.09 (0.07-0.12) | 0.08 (0.06-0.11) | 1.15 (0.75-1.75) |
| Colon, unspecified | 4237 | 3.93 (3.75-4.11) | 4.42 (4.14-4.69) | 3.44 (3.20-3.68) | 4.22 (4.05-4.39) | 4.72 (4.46-4.98) | 3.74 (3.51-3.97) | 1.07 (1.01-1.14) | 1.07 (0.98-1.16) | 1.09 (0.99-1.19) | 4.09 (3.96-4.21) | 4.58 (4.39-4.76) | 3.60 (3.44-3.77) | 1.27 (1.19-1.35) |
| Rectosigmoid | 1393 | 1.22 (1.11-1.32) | 1.33 (1.18-1.48) | 1.10 (0.96-1.23) | 1.42 (1.32-1.52) | 1.73 (1.57-1.89) | 1.12 (1.00-1.25) | 1.17 (1.05-1.30) | 1.30 (1.13-1.50) | 1.02 (0.87-1.21) | 1.33 (1.25-1.40) | 1.54 (1.43-1.65) | 1.11 (1.02-1.20) | 1.39 (1.25-1.55) |
| Rectum | 3657 | 3.02 (2.86-3.17) | 3.46 (3.22-3.70) | 2.57 (2.36-2.77) | 3.85 (3.69-4.01) | 4.79 (4.53-5.05) | 2.92 (2.72-3.12) | 1.28 (1.19-1.36) | 1.39 (1.27-1.51) | 1.14 (1.02-1.26) | 3.46 (3.34-3.57) | 4.16 (3.98-4.34) | 2.75 (2.61-2.89) | 1.51 (1.42-1.62) |
| Total | 15279 | 12.21 (11.89-12.53) | 13.72 (13.23-14.20) | 10.67 (10.25-11.10) | 16.81 (16.47-17.15) | 19.46 (18.94-19.99) | 14.19 (13.75-14.64) | 1.38 (1.33-1.42) | 1.42 (1.36-1.48) | 1.33 (1.27-1.40) | 14.67 (14.44-14.91) | 16.76 (16.41-17.12) | 12.58 (12.28-12.89) | 1.33 (1.29-1.38) |
| M Group: Others | ||||||||||||||
| Cecum | 77 | 0.03 (0.01-0.04) | 0.03 (0.01-0.05) | 0.02 (0.00-0.04) | 0.11 (0.08-0.14) | 0.12 (0.08-0.16) | 0.10 (0.06-0.13) | 4.13 (2.42-7.05) | 4.09 (2.00-8.39) | 4.19 (1.88-9.35) | 0.07 (0.05-0.08) | 0.07 (0.05-0.10) | 0.06 (0.04-0.08) | 1.18 (0.75-1.87) |
| Appendix | 40 | 0.02 (0.01-0.03) | 0.02 (0.00-0.03) | 0.02 (0.00-0.04) | 0.04 (0.03-0.06) | 0.03 (0.01-0.05) | 0.05 (0.02-0.07) | 2.15 (1.09-4.24) | 1.78 (0.66-4.83) | 2.58 (1.02-6.51) | 0.03 (0.02-0.04) | 0.03 (0.01-0.04) | 0.03 (0.02-0.05) | 0.75 (0.39-1.42) |
| Ascending colon | 31 | 0.01 (0.00-0.02) | 0.00 (0.00-0.01) | 0.01 (0.00-0.02) | 0.04 (0.03-0.06) | 0.06 (0.03-0.08) | 0.03 (0.01-0.05) | 5.62 (2.31-13.65) | 13.05 (3.18-53.55) | 2.93 (0.87-9.83) | 0.03 (0.02-0.04) | 0.03 (0.02-0.05) | 0.02 (0.01-0.04) | 1.39 (0.67-2.89) |
| Hepatic flexure | 11 | 0.01 (0.00-0.01) | 0.01 (0.00-0.02) | 0.00 (0.00-0.01) | 0.01 (0.00-0.02) | 0.01 (0.00-0.03) | 0.01 (0.00-0.02) | 1.64 (0.48-5.61) | 1.09 (0.24-4.95) | 3.82 (0.40-36.52) | 0.01 (0.00-0.02) | 0.01 (0.00-0.02) | 0.01 (0.00-0.02) | 1.54 (0.45-5.27) |
| Transverse colon | 13 | 0.01 (0.00-0.02) | 0.01 (0.00-0.02) | 0.01 (0.00-0.02) | 0.01 (0.00-0.02) | 0.01 (0.00-0.03) | 0.01 (0.00-0.03) | 1.39 (0.45-4.28) | 1.45 (0.34-6.11) | 1.27 (0.22-7.46) | 0.01 (0.01-0.02) | 0.01 (0.00-0.02) | 0.01 (0.00-0.02) | 1.13 (0.37-3.45) |
| Splenic flexure | 7 | 0.01 (0.00-0.02) | 0.01 (-0.01-0.03) | 0.00 (0.00-0.01) | 0.01 (0.00-0.01) | 0.01 (0.00-0.02) | 0.00 (0.00-0.01) | 0.90 (0.19-4.21) | 0.95 (0.15-5.93) | 0.66 (0.04-11.64) | 0.01 (0.00-0.01) | 0.01 (0.00-0.02) | 0.00 (0.00-0.01) | 3.15 (0.60-16.68) |
| Descending colon | 17 | 0.00 (0.00-0.01) | 0.00 (0.00-0.01) | 0.00 (0.00-0.00) | 0.03 (0.01-0.04) | 0.05 (0.02-0.07) | 0.01 (0.00-0.02) | 11.90 (2.89-48.91) | 10.02 (2.24-44.84) | --- | 0.02 (0.01-0.02) | 0.03 (0.01-0.04) | 0.01 (0.00-0.01) | 4.72 (1.49-14.93) |
| Sigmoid colon | 76 | 0.06 (0.04-0.08) | 0.08 (0.04-0.11) | 0.04 (0.01-0.06) | 0.07 (0.05-0.09) | 0.09 (0.05-0.12) | 0.06 (0.03-0.09) | 1.27 (0.80-2.01) | 1.13 (0.64-1.99) | 1.60 (0.72-3.54) | 0.07 (0.05-0.08) | 0.08 (0.06-0.11) | 0.05 (0.03-0.07) | 1.73 (1.08-2.78) |
| Overlapping sites of colon | 4 | 0.00 (0.00-0.00) | 0.00 (0.00-0.00) | 0.00 (0.00-0.00) | 0.01 (0.00-0.01) | 0.01 (0.00-0.02) | 0.00 (0.00-0.01) | --- | --- | --- | 0.00 (0.00-0.01) | 0.00 (0.00-0.01) | 0.00 (0.00-0.01) | 2.10 (0.26-17.28) |
| Colon, unspecified | 291 | 0.23 (0.18-0.27) | 0.26 (0.19-0.32) | 0.20 (0.14-0.25) | 0.31 (0.26-0.35) | 0.34 (0.27-0.41) | 0.28 (0.21-0.34) | 1.35 (1.07-1.72) | 1.32 (0.96-1.81) | 1.40 (0.98-2.01) | 0.27 (0.24-0.30) | 0.30 (0.25-0.35) | 0.24 (0.20-0.28) | 1.25 (0.99-1.59) |
| Rectosigmoid | 58 | 0.04 (0.02-0.06) | 0.05 (0.02-0.08) | 0.03 (0.01-0.05) | 0.06 (0.04-0.08) | 0.08 (0.05-0.12) | 0.04 (0.02-0.06) | 1.60 (0.94-2.73) | 1.66 (0.86-3.21) | 1.54 (0.62-3.80) | 0.05 (0.04-0.07) | 0.07 (0.05-0.09) | 0.04 (0.02-0.05) | 1.97 (1.15-3.40) |
| Rectum | 376 | 0.15 (0.11-0.18) | 0.19 (0.13-0.24) | 0.10 (0.06-0.14) | 0.52 (0.46-0.58) | 0.56 (0.47-0.65) | 0.48 (0.40-0.56) | 3.58 (2.83-4.51) | 3.02 (2.23-4.08) | 4.62 (3.19-6.69) | 0.35 (0.31-0.38) | 0.38 (0.33-0.44) | 0.31 (0.26-0.36) | 1.25 (1.02-1.54) |
| Total | 1001 | 0.55 (0.48-0.62) | 0.66 (0.56-0.76) | 0.43 (0.35-0.52) | 1.22 (1.13-1.32) | 1.37 (1.24-1.51) | 1.08 (0.95-1.20) | 2.23 (1.95-2.54) | 2.07 (1.74-2.47) | 2.47 (2.01-3.04) | 0.91 (0.85-0.97) | 1.04 (0.95-1.12) | 0.78 (0.70-0.86) | 1.33 (1.17-1.51) |
| M Group: Total | ||||||||||||||
| Cecum | 940 | 0.45 (0.39-0.51) | 0.50 (0.41-0.59) | 0.40 (0.32-0.48) | 1.30 (1.20-1.39) | 1.49 (1.35-1.64) | 1.10 (0.98-1.23) | 2.88 (2.50-3.32) | 2.98 (2.47-3.61) | 2.76 (2.23-3.43) | 0.91 (0.85-0.97) | 1.03 (0.94-1.12) | 0.79 (0.71-0.86) | 1.31 (1.15-1.49) |
| Appendix | 99 | 0.07 (0.04-0.09) | 0.06 (0.03-0.09) | 0.07 (0.04-0.11) | 0.10 (0.08-0.13) | 0.08 (0.05-0.11) | 0.13 (0.09-0.17) | 1.56 (1.03-2.36) | 1.35 (0.71-2.58) | 1.73 (1.00-2.99) | 0.08 (0.07-0.10) | 0.07 (0.05-0.09) | 0.10 (0.07-0.13) | 0.68 (0.45-1.03) |
| Ascending colon | 838 | 0.44 (0.38-0.50) | 0.50 (0.41-0.60) | 0.37 (0.29-0.45) | 1.12 (1.03-1.21) | 1.33 (1.19-1.47) | 0.92 (0.81-1.03) | 2.57 (2.21-2.98) | 2.63 (2.17-3.20) | 2.48 (1.97-3.12) | 0.81 (0.75-0.86) | 0.95 (0.86-1.03) | 0.67 (0.60-0.74) | 1.41 (1.23-1.62) |
| Hepatic flexure | 212 | 0.11 (0.08-0.14) | 0.11 (0.07-0.16) | 0.10 (0.06-0.15) | 0.29 (0.24-0.33) | 0.35 (0.28-0.42) | 0.23 (0.17-0.28) | 2.64 (1.97-3.55) | 3.08 (2.08-4.57) | 2.16 (1.38-3.39) | 0.21 (0.18-0.23) | 0.24 (0.20-0.28) | 0.17 (0.14-0.21) | 1.38 (1.05-1.82) |
| Transverse colon | 480 | 0.30 (0.25-0.35) | 0.33 (0.26-0.40) | 0.27 (0.20-0.34) | 0.58 (0.52-0.64) | 0.73 (0.63-0.84) | 0.43 (0.35-0.51) | 1.93 (1.60-2.34) | 2.25 (1.76-2.88) | 1.58 (1.18-2.13) | 0.45 (0.41-0.49) | 0.55 (0.48-0.61) | 0.36 (0.30-0.41) | 1.53 (1.28-1.85) |
| Splenic flexure | 205 | 0.18 (0.14-0.21) | 0.20 (0.14-0.26) | 0.15 (0.10-0.20) | 0.22 (0.18-0.26) | 0.22 (0.16-0.27) | 0.22 (0.17-0.28) | 1.25 (0.94-1.65) | 1.06 (0.72-1.56) | 1.51 (1.00-2.27) | 0.20 (0.17-0.23) | 0.21 (0.17-0.25) | 0.19 (0.15-0.23) | 1.11 (0.84-1.46) |
| Descending colon | 594 | 0.39 (0.33-0.44) | 0.41 (0.33-0.50) | 0.36 (0.28-0.44) | 0.74 (0.66-0.81) | 0.82 (0.71-0.93) | 0.65 (0.56-0.75) | 1.91 (1.61-2.26) | 2.00 (1.58-2.52) | 1.81 (1.41-2.33) | 0.57 (0.53-0.62) | 0.63 (0.56-0.70) | 0.52 (0.45-0.58) | 1.22 (1.03-1.44) |
| Sigmoid colon | 2807 | 2.16 (2.02-2.30) | 2.46 (2.25-2.67) | 1.86 (1.68-2.03) | 3.21 (3.06-3.37) | 3.49 (3.27-3.72) | 2.94 (2.74-3.14) | 1.49 (1.38-1.61) | 1.42 (1.28-1.58) | 1.58 (1.41-1.77) | 2.73 (2.62-2.83) | 3.00 (2.85-3.16) | 2.45 (2.31-2.59) | 1.23 (1.14-1.32) |
| Overlapping sites of colon | 93 | 0.10 (0.07-0.13) | 0.10 (0.06-0.14) | 0.10 (0.05-0.14) | 0.08 (0.06-0.11) | 0.10 (0.06-0.13) | 0.07 (0.04-0.11) | 0.85 (0.56-1.29) | 0.93 (0.53-1.64) | 0.76 (0.41-1.42) | 0.09 (0.07-0.11) | 0.10 (0.07-0.12) | 0.08 (0.06-0.11) | 1.18 (0.78-1.78) |
| Colon, unspecified | 4528 | 4.16 (3.97-4.34) | 4.67 (4.39-4.95) | 3.64 (3.39-3.88) | 4.53 (4.35-4.71) | 5.05 (4.79-5.32) | 4.01 (3.78-4.25) | 1.09 (1.03-1.16) | 1.08 (1.00-1.17) | 1.10 (1.01-1.21) | 4.36 (4.23-4.49) | 4.88 (4.68-5.07) | 3.84 (3.67-4.01) | 1.27 (1.20-1.35) |
| Rectosigmoid | 1451 | 1.25 (1.15-1.36) | 1.38 (1.23-1.53) | 1.12 (0.99-1.26) | 1.49 (1.38-1.59) | 1.81 (1.65-1.97) | 1.16 (1.04-1.29) | 1.18 (1.07-1.32) | 1.32 (1.15-1.51) | 1.04 (0.88-1.22) | 1.38 (1.31-1.45) | 1.61 (1.50-1.72) | 1.14 (1.05-1.23) | 1.41 (1.27-1.57) |
| Rectum | 4033 | 3.16 (3.00-3.32) | 3.64 (3.40-3.89) | 2.67 (2.46-2.88) | 4.37 (4.20-4.55) | 5.35 (5.08-5.63) | 3.40 (3.19-3.61) | 1.38 (1.30-1.47) | 1.47 (1.35-1.60) | 1.27 (1.15-1.41) | 3.80 (3.68-3.92) | 4.55 (4.36-4.73) | 3.06 (2.91-3.21) | 1.49 (1.40-1.59) |
| Total | 16280 | 12.76 (12.43-13.08) | 14.38 (13.89-14.87) | 11.11 (10.68-11.54) | 18.03 (17.68-18.39) | 20.84 (20.29-21.38) | 15.27 (14.81-15.73) | 1.41 (1.37-1.46) | 1.45 (1.39-1.51) | 1.37 (1.31-1.44) | 15.58 (15.34-15.83) | 17.80 (17.43-18.17) | 13.36 (13.05-13.68) | 1.33 (1.29-1.37) |
Abbreviations: CI, confidence interval; SRR, standardized rate ratio.
a ASR: The age-standardized incidence rate of colorectal cancer per 100 000 person-years, using new WHO standard population.
b M group: The morphology group based on the third version of ICD-O; C group: The topography group based on the third version of ICD-O.
Overall, The ASR of CRC was 15.58 (95% CI: 15.34 - 15.83) per 100 000 person-years. Also, the ASR in males and females was 17.80 (95% CI: 17.34 - 15.83) and 13.36 (95% CI: 13.05 - 13.68) per 100 000 person-years, respectively. The results showed that the SRR (ASR rate ratio of males to a female) was 1.33 (95% CI: 1.29 - 1.37), which indicates significantly higher ASR in males compared to females during the study period. By using the 95% CI of SRR, the ASR of males and females were not different in Appendix, Splenic flexure, and overlapping site of the colon from 2006 to 2015 (Table 3).
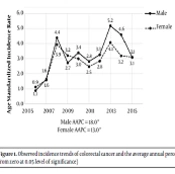
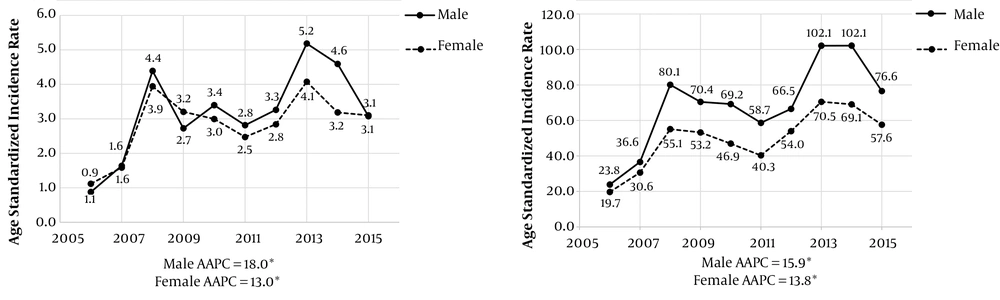
Figure 1 showed the overall trend of ASR in age < 50 and age ≥ 50 by males and females. Based on the results, the ASR was much higher in age ≥ 50 compared to age < 50. Furthermore, the difference of ASR between males and females was lower for age < 50 in comparison to age ≥ 50. All AAPCs in age < 50 and age > 50 were positive, indicating a significant upward trend of ASR.
5. Discussion
The incidence of CRC is a growing concern in Eastern Mediterranean countries (21, 22). To this point, the current study was performed to analyze the data collected from 16 280 CRC records provided by 3 leading universities of Iran, including Tehran University of Medical Sciences, Iran University of Medical Sciences, and Shahid Beheshti University of Medical Sciences during 10 years (2006 and 2015). The ASR of CRC was 15.58 (95% CI: 15.34 - 15.83) per 100 000 person-years. The results indicated that the overall trend of ASR in CRC cases older than 50 years old was significantly higher than patients with age less than 50. Besides, the incidence of CRC was more in the male subjects. Most of the tumors were detected in the rectum, sigmoid, and colon. An AAPC of adenocarcinoma was higher in males. The association between higher CRC incidence and aging was demonstrated in the previous study in Iran that is in line with our findings. It can be defined by the genetic mutations due to molecular changes by aging including disruption of DNA repair mechanisms and cell growth regulation systems, increased inflammation, and decreased immune system function (16). However, with the growing trend of obesity and type 2 diabetes, the risk factors of CRC may change this pattern (22). Austin et al. reported an increasing trend in CRC incidence rate among young adults (< 50 years) in the USA (23).
The impact of gender as a risk parameter in CRC incidence is remained uncertain (24). However, several studies reported a higher proportion of neoplasia in males (25-27). A meta-analysis indicated that the risk of being diagnosed with CRC in men is twice that of women (28). Our analysis also revealed a higher incidence of CRC. Lieberman et al. stated a 5-years delay in the incidence of CRC in females (29). A study in the east of England reported no significant gender difference for CRC (30). The tumor location parameter is seemed to have a meaningful impact on CRC incidence. The first impression is that the tumor growth at the common colon sites such as descending colon, sigmoid, and rectum regions facilities the screening and increases the chance of cancer diagnosis. However, about two-thirds of CRC adenomas have been reported to detect beyond the sigmoid region and probability in an unspecified location of the colon area (31). The present study also showed the highest number of CRC incidence in all studied topographies, unspecified colon regions, as well as the rectum and sigmoid colon sites. On the other hand, the incidence of CRC tumors at transverse and colon sites of the CRC samples collected from 2011 to 2015 were significantly higher than those from 2006 to 2010. This is probably because of applying the more advanced screening tools in the last years, which facilitated the diagnosis process. As mentioned earlier, CRC is one of the most common cancers in Iran. In a study on the Iranian CRC population in 2003, colon cancer was ranked as the fourth most prevalent cancer in Ardabil (Province of north-west) with an ASR of 7.86 and 5.89 per 100 000 per year in males and females, respectively (32). This report was confirmed by a similar study in 2005, confirming a sharp increase of colon cancer in the Iranian population (33). Accordingly, Pahlavan et al. reported that the ASR of CRC in some provinces of Iran was higher than most of the Asian countries, and suggested the impact of westernization of Iranian diet and lifestyle (34).
In our study, the ASR of CRC increased from the second period of study (2011 - 2015) in comparison to the first period (2006 - 2010). This may be defined by the improvement of data collection and quality control process in the National Cancer Registration System in Iran and lifestyle.
5.1. Conclusions
According to the National Cancer Registration System, the coverage of the registry had a growing trend particularly in 2013. The rising trend is partially due to improvement in data collection, westernized lifestyle, and environmental risks. Cancer control programs need to be adjusted based on the status of cancer incidence, mortality, and risk factors in Tehran Province. Therefore, the results of this study could provide comprehensive information on the patterns of the epidemiology and morphology of CRC in the Tehran metropolis and could be useful for policymakers in the development of more precise CRC control programs.