1. Background
ER generally facilitates a rapid evaluation of the patient and it is usually accessed by patients in critical condition. ER plays a key role in the management of patients with chronic diseases, as well as in the use of pain therapies in the end-of-life care (EOLC) (1, 2) and in critical events leading to death (3-5); this can be observed especially in people with locally advanced or metastatic cancer. Patients with advanced cancer can often present new symptoms such as exacerbation of existing diseases or comorbidities, complications of treatment, and consequences of disease progression. Added to this are the difficulties to access the healthcare system and territorial support, the lack of an approach and an environment that balances the decisive action with sensitivity, privacy, and centrality of the person (6). Starting from these observations, it has been established that the Italian ER, which are often overcrowded and provide assistance to multiple patients at the same time, are not adequate to treat patient with cancer, who are in need of urgent care. Patients with cancer require, indeed, a multidisciplinary approach by doctors who collaborate to guarantee the best diagnostic and therapeutic options. In contrast, preventive medicine and family physicians, who play an active role in raising awareness of cancer prevention and identifying cancer-related symptoms, are unable to recognize the presence of a tumor in many cases, and consequently refer patients to the specialist; for this reason, ER hospitalization becomes an inevitable part of the treatment of patients with cancer.
2. Objectives
In our hospital we conducted a 22-month trial in the ER, under the supervision of our Oncology Department, with the aim of both promoting de-hospitalization and improving diagnostic and therapeutic performance, saving, also, on healthcare costs.
3. Methods
A total of 1,414 patients admitted to the ER of the Antonio Cardarelli Hospital, from May 2018 to March 2020 (for a total of 340 observation days), were observed by an Experimental First Aid Oncology Service, active 6 hours a day, 5 days a week. A protocol required the accepting physician to transfer patients with suspected cancer to the oncologist in the ER was developed, who acted as supervisor and coordinator. A first consultation was carried out together with one or more specialists identified by the supervisor such as the surgeon, gastroenterologist, bronchologist, vascular radiologist, geneticist, and others, in the context of the emergency. Once the patients were framed, a dedicated nurse (CM) took them in charge in the MTB they were referred to. Based on their characteristcs, patients were divided into 4 categories:
1- Patients with a known cancer diagnosis and already in oncological treatment, who arrive to ER for complications directly or indirectly related to the worsening of the disease;
2- Patients who show complications due to ongoing cancer treatments;
3- Patients who not responsive anymore to oncological treatments due to the worsening of the disease; this category mainly included patients in the terminal phase of the disease;
4- Patients who receive first diagnosis of cancer in the ER. Each individual cohort of patients was addressed to different therapeutic diagnostic paths according to each patients’ needs and their oncological disease stage.
Non-discharged patients were directed to ordinary hospitalization in a medical or surgical department for further diagnosis or to overcome the acute phase. Toxicities related to the treatment were directly dealt with the oncology department. Patients in the terminal phase of the disease were moved to the analgesic therapy unit present in the hospital or directed to hospice facilities in the area or home care activated through the Campania Oncology Network (ROC). Conversely, patients with first diagnosis were de-hospitalized and entrusted with individual Multidisciplinary Tumor Board (MTB).
4. Results
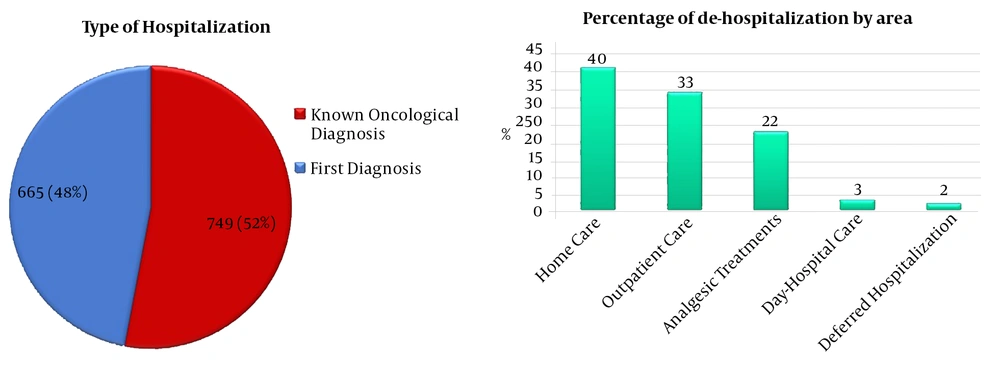
Patients diagnosed with lung or pleural carcinoma were 405; 219 patients were diagnosed with gastric carcinoma, 213 subjects were diagnosed with kidney tumor, and 74 patients were diagnosed with pancreatic cancer. Breast cancer was diagnosed in 70 patients; 64 subjects were instead diagnosed with prostate cancer; 59 were gynecological cancer diagnosis while those related to the oropharyngeal sphere were 44. The cases with biliary tract tumors were 31, hepatocarcinoma (HCC) were 30, and the sarcomas were 28. The remaining 63 patients were diagnosed with other tumors, not reaching the 2% (Table 1). These data were comparable to those collected nationwide. Among these 1,414 patients were observed, 48% (665 patients) received the first diagnosis of cancer in the ER, while 52% (749 subjects) was already aware of the oncological pathology (Figure 1A). Furthermore, 484 patients (34%) were de-hospitalized, 40% of whom were placed in home care; 33% was directed to outpatient clinic care (MTB); 22% were directed to analgesic therapies; 3% to day hospital, and the last 2% were hospitalized in a deferred hospitalization (Figure 1B). So far, we do not have all the complete statistical data but we can say something about the lung. Preliminary data showed us that the median hospitalization time for lung cancer patients who followed the study was 10 days, compared with 16 days for patients who were not screened for cancer in the ER.
A, Schematic representation of the distribution of the 1,414 patients admitted to the ER. 48% of them received the first tumor diagnosis at the oncological ER; B, The histograms schematically represent the percentages of de-hospitalization by area. The total percentage number of de-hospitalized patients is 33%.
| Cancer TypesA | Patients (N = 1,414)B | Male/FemaleC | Age ± SEMD | First DiagnosisE |
|---|---|---|---|---|
| Lung/pleura | 405 (29) | 314/91 | 66.9 ± 1.3 | 229 (57) |
| Gastrointestinal | 219 (15) | 131/88 | 66.6 ± 1.4 | 106 (48) |
| Bladder/kidney | 213 (15) | 164/49 | 68.4 ± 1.5 | 90 (42) |
| Unknown | 114 (8) | 70/44 | 65.7 ± 1.7 | 84 (73) |
| Pancreas | 74 (5) | 44/30 | 65.4 ± 1.4 | 38 (51) |
| Breast | 70 (5) | 0/70 | 62.6 ± 1.7 | 19 (27) |
| Prostate | 64 (5) | 64/0 | 72.5 ± 1.0 | 17 (27) |
| Gynecological | 59 (4) | 0/59 | 60.7 ± 1.5 | 16 (27) |
| Head/neck | 44 (3) | 37/7 | 62.2 ± 1.1 | 12 (27) |
| Others | 152 (11) | 106/46 | 64.3 ± 1.8 | 60 (39) |
aThe table shows A, types of diagnosis. In the group “others” all those tumors that did not reach 2% of the total were included; B, the total number of diagnoses for each type of cancer; the percentage of cases out of the total is indicated in brackets; C, male/female cases; D, the average age as mean ± SEM; E, number of cases per pathology, which received the first diagnosis in the ER expressed as an absolute value and as a percentage (in brackets).
5. Discussion
Almost 4% of the Italian population has a history of oncological disease. For 40% of this population, the diagnosis of cancer is more recent than 5 years and it is assumed that a relevant part still has active disease or clinical results of the treatments received. The size of these people’s access to ER is therefore potentially significant. Data from the United States indicates that the incidence of patients with cancer among all the patients accessing the Emergency and Acceptance Departments (DEA) is about 3%. Furthermore, the hospitalization rate of patients with cancer is higher than the rest of the population. The most frequent reason for urgent hospitalization for patients with cancer is the presence of symptoms and, in most cases, the symptoms are related to the progression of the disease (7). A second reason for accessing to ER is the toxicity of anticancer treatments; serious events that may not be solved in an outpatient basis (4). Twenty-two months of emergency oncological experience have allowed us to highlight several critical issues and therefore to hypothesize what the mandatory changes would be forbetter and more effective management of the patients with cancer in the ER. The general underestimation by specialist doctors of the incidence and severity of symptoms is well documented in literature (8). A more accurate detection of the symptoms could certainly lead to a better control and would therefore allow to intercept at least a part of the needs before they turn into a real emergency. The pain is still the most common reason for hospitalization. There is no doubt that more efficient ways of reporting to both the family doctor and the specialized referral center would lead to better timely symptom management. As regards the toxicities of oncological treatments, the containment of unscheduled access is probably obtainable through a better selection of patients at the entrance and adherence to the guidelines on the management of the main side effects (9). But above all, it is the ability to intercept events early and prevent their worsening which probably has a major effect on hospitalization. Experiences related to regular toxicity monitoring through nursing care, phone calls, and more refined telemedicine tools have shown a reduction in serious toxicities and a reduction in unscheduled access to the hospital (10). This involves a change in the internal organization of the oncological department, the implementation of internal alarm systems, and above all a greater integration with territorial medicine. The last observation concerns the high number of tumors diagnosed for the first time in the ER in our hospital. These data are in contrast with what happens in northern Italy where the rate of first cancer diagnosis in the ER is lower. This difference could be caused by a lack of prevention and treatment of oncological diseases by the territorial medicine of Southern Italy (11-13). Lung tumors, disseminated tumors of unknown origin, colon tumors, kidney tumors, and pancreatic tumors represent tumors that are more frequently diagnosed at first in our ER. The absence of valid screening and prevention programs could justify this higher frequency compared to other type of cancer, such as breast cancer and gynecological cancers, where preventive medicine plays an important role. In this cohort of patients, routine ER imaging may reveal the first cancer diagnosis in the absence of overt cancer symptoms. the patients suddenly discovered to have a tumor and they had the first approach to their oncological disease in an ER. Our experience allowed us to develop a better level of assistance for these patients; once, indeed, that these patients pass the clinical urgency phase, are de-hospitalized directly from the ER and directed to outpatient clinic or Day Hospital paths with specialized medical teams, the MTB. The support of a professional nurse and the CM represents the trait d’union between the medical team and domiciled patients. The presence of the MTB, specific for each kind of cancer, facilitates the diagnosis and treatment of the patient, who is directed to approved diagnosis and therapy procedures in a multidisciplinary context, according to a specific Diagnostic Therapeutic Assistance path (PDTA), avoiding unnecessary and inconsistent examinations, not in agreement with guidelines.
5.1. Conclusions
Based on our 22-months experience in oncological ER, we can conclude that a better integration between oncology, palliative care, territorial medicine, emergency medicine, and MTB could improve the quality and efficiency of services, reducing redundant, and inappropriate services. This experimental protocol has allowed us to promptly activate paths dedicated to individual neoplastic pathologies, drastically reducing the physiological waiting times, typical of a traditional hospitalization, allowing to speed up diagnosis times, and consequently reducing the days of hospitalization. The preliminary statistical data available allowed us to argue that the average hospitalization time for patients with lung cancer who followed the trial was 10 days, compared to 16 days for patients who did not undergo cancer screening in the ER. Another relevant result that demonstrates the improvement in the quality and efficiency of medical services by including first aid in the management of patients with cancer concerns de-hospitalization. In fact, thanks to the experimental protocol we applied, we were able to de-hospitalize 484 patients directly from the ER, that is to say more than 34% of the total. These patients without the “filter” of the oncological ER would all have been hospitalized with negative effects on the efficiency of the health system and on its costs.
A health policy based on these goals would guarantee a better quality of care and, at the same time, lead to a decrease in healthcare costs. The creation of a permanent and full-time first aid oncology unit could be the first, essential step to achieve these goals.