1. Introduction
The most common GI tract mesenchymal tumor is the gastrointestinal stromal tumor (GIST) (1). In the past, GIST was one of the difficult treated tumors that showed a low response to chemoradiotherapy (2, 3). Firstly, the efficacy of imatinib was shown in metastatic GIST and, then, the efficacy of imatinib was seen in the treatment of this type of tumors and used for adjuvant and neoadjuvant therapy (4-10).
GISTs are commonly presented with abdominal pain or gastrointestinal (GI) bleeding that may be acute with the presentation of upper or lower GI bleeding as melena, hematemesis, and hematochezia or chronically with symptoms of anemia such as malaise, dyspnea, and other symptoms of anemia. Other less common presentations of GIST are mass, weight loss, and sign and symptoms of obstruction as nausea, vomiting, obstipation, etc. Some rare presentations as perforation are reported in literatures (11-18).
Small size tumors may be asymptomatic and lead to delay in diagnosis. On the other hand, in other symptomatic patients, most of their symptoms are non-specific and this behavior often causes over 50% of patients diagnosed with a case of GIST to have metastasis at the first presentation and postpone diagnosis and treatment (15-19).
2. Case Presentation
A 31-year-old man presented to our hospital with 10 days history of acute onset epigastric pain that increased gradually with nausea and coffee ground vomiting. He had a history of anorexia and weight loss one month ago. When he arrived, his vital signs were normal.
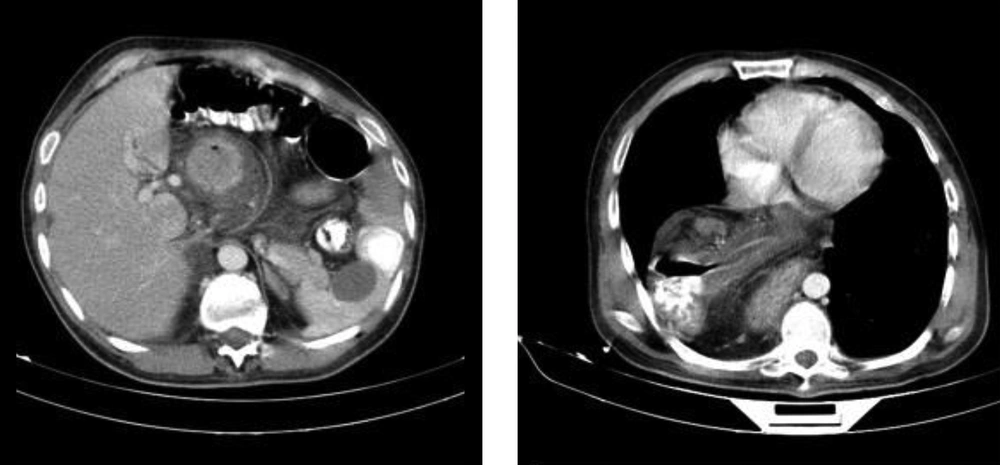
Abdominal examination revealed mild tenderness in the epigastrium and other parts of the abdomen were soft and without tenderness. Laboratory data showed white blood cell count, electrolytes were normal, and renal and liver function tests were in the normal range and a hemoglobin level of 5.2 g/dL (hypochromic, microcytic). Plain abdominal radiography was unremarkable and a CT scan of thorax and abdomen was, therefore, done; large paraesophageal hernia, thickened, and enhancing mass in gastric antrum near the diaphragmatic hiatus with localized perforation and abscess around it were detected (Figure 1). After resuscitation and packed cell infusion, the patient was transferred to the operating room for urgent laparotomy.
After laparotomy, the abdomen was explored. In exploration, the total part of the stomach was herniated in right hemithorax in the paraesophageal route. The stomach was released from crosses of the diaphragm and delivered from right hemithorax to abdomen. Next, a large perforated antral mass was detected in the stomach. Another part of the abdomen was explored and no evidence of liver and peritoneal metastases and pathology of other organs was not seen. There was no contamination from the perforation in the thorax and abdomen and we did not have the pathology of this tumor; so, we planned for an oncosurgeric procedure. After releasing the stomach, hernia repair, subtotal gastrectomy, and roux-en-y antecolic gastrojejunostomy were performed (Figure 2). The patient was uneventfully recovered on the postoperative period and discharged on the fifth postoperative day.
2.1. Pathology
The incidence of GIST is 0.1% to 3% of all the gastrointestinal tumors that are mesenchymal tumors of the digestive tract, which arise from the interstitial cells of Cajal. They are mostly presented in the stomach and small intestine (20) with abdominal mass (5%-50%), hemorrhage, obstruction (5%), and rarely perforation as its symptoms (21, 22).
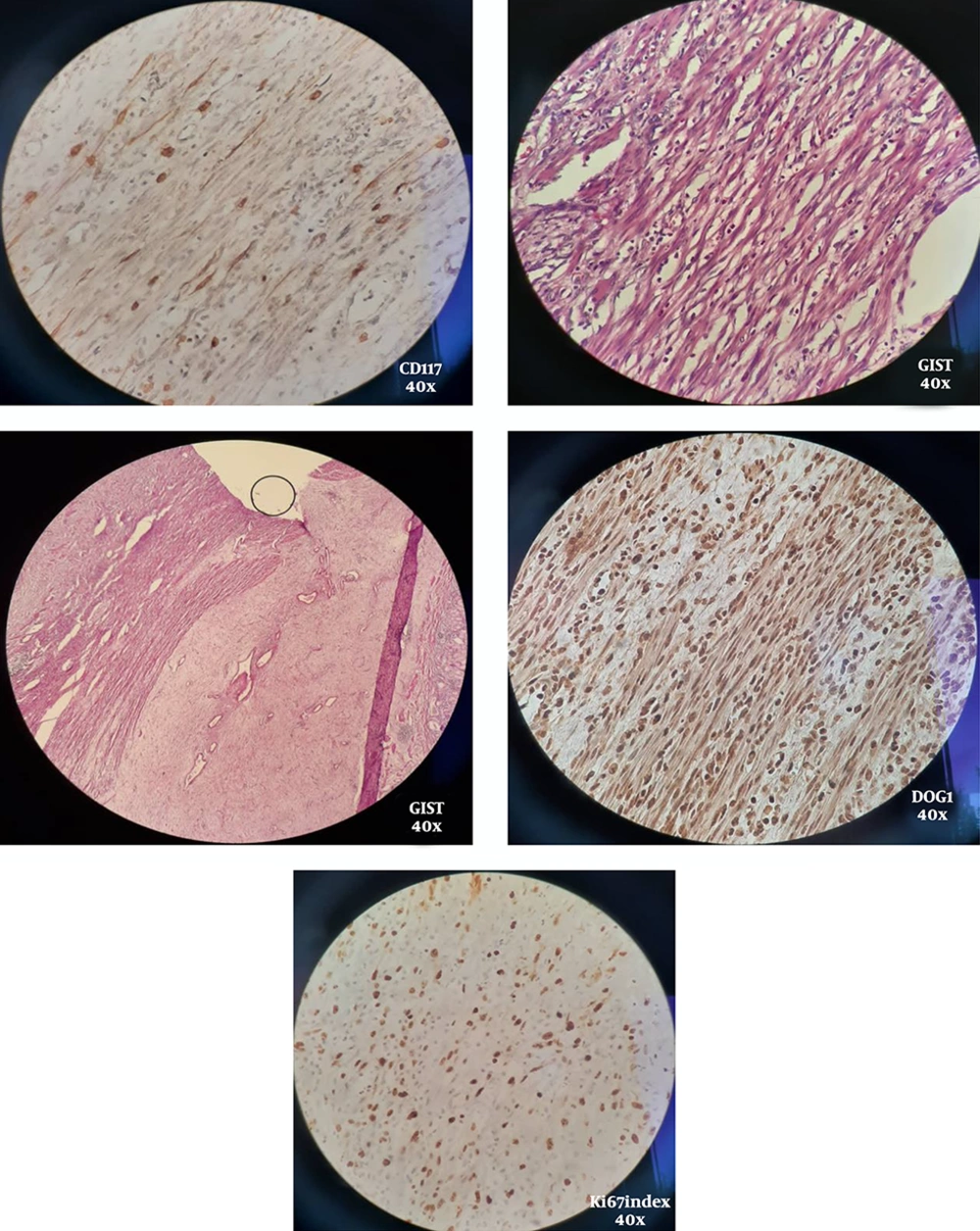
There are 3 morphologic types; Spindle (70%), epitheliod (20%), round cell, and admixture (23, 24).
The majority of GISTs (80%-90%) have a mutation in the C_KIT gene (80%) or platelet-derived growth factor receptor (PDGFR_alpha), which code the type III receptor tyrosine kinases; therefore, they are positive for KIT (CD117) protein staining (25).
About 95% of GISTs are positive for KIT by Immunohistochemistry. In the remaining 5%, proper morphologic findings along with DOG1 immunoreactivity can be diagnostic.
Microscopic findings revealed a spindle cell neoplasm. These cells contained eosinophilic cytoplasm and inconspicuous nucleoli.
Cut sections show a CD117 and DOG1 positive spindle cell type GIST (Figure 3).
The greatest dimension of the tumor is 8cm and the mitotic rate is > 5/5 mm2; therefore, the tumor is in the high-risk category for progressive disease on Miettinen’s criteria. Margins are clear and also 7 reactive lymph nodes are submitted with no vascular invasion.
Follow-up pathology revealed that the tumor was GIST. Tumor size was 8*5*5 cm with a clear margin and 7 dissected lymph nodes were reactive. Pathologic stage was PT3N0Mx.
He was discussed in a multidisciplinary team and further treatment with tyrosine kinase inhibitors was started.
3. Discussion
Epidemiological studies show that GIST occurs about 6.8 to 14.5 cases per million individuals every year and the mean age is 60 (26-28). The most common site for GISTs is in the stomach (51%). Other sites are the small intestine with 36% of tumors, colon with 7%, rectum with 5%, and esophagus with 1% of all GISTs (29).
The most common symptom is gastrointestinal bleeding that may present with acute melena and hematemesis with subsequent anemia. Other symptoms may present with weakness and abdominal pain and less commonly with distension, as well as discomfort due to a tumor-induced mass effect (30). Incidentally, the diagnosis of GIST occurred in 15% to 30% of patients after their death and autopsy, or patients who underwent surgery for other reasons, and this tumor was found during surgery (31).
The symptom of our patient was abdominal pain and upper GI bleeding. The operative finding was perforation of the antrum and right-sided paraesophageal hernia. Also, most previous studies such as Roy et al. (26) and Hosamani et al. (13) showed perforation of GIST on the small intestine and Meckel's diverticulum. In the patient presented here perforation was in the antrum. Skipworth et al. (Roy et al., 2012) (29) reported perforation in the stomach. The reason for the lower risk of gastric perforation is unclear but it may due to the thickness of the gastric wall compared to the large and small bowel. Perforated GISTs should undergo an operation for emergency surgical resection. The mortality rate of gastrointestinal tract perforation for all reasons is high (> 25%). Though perforation of Gastric GIST is extremely rare, it should be kept in mind while dealing with GIST, stomach, or perforation peritonitis.
3.1. Conclusions
In this study, we described one of the rarest of a gastric GIST presenting with perforation. GISTs should be in the differential diagnosis of all patients, who are diagnosed with GI tract masses and GI tract perforation. Our case shows that there is a need for more attention to new upper GI symptoms in all age groups to prevent dangerous consequences.